Persistent Pain and Itch in Gluteal Cleft and Perineum: A Quiz
Mari Karjalainen1, Harry Kujari2, and Niina Hieta1*
Departments of 1Dermatology and 2Pathology, Turku University Hospital and University of Turku, PO Box 52, FIN-20521 Turku, Finland. *E-mail: niina.hieta@utu.fi
A 66-year-old female patient was referred to the dermatology clinic with a suspected dermatological condition because of anogenital symptoms. She was using vaginal suppositories containing 10 mg oestradiol twice a week for postmenopausal symptoms and 1–4 tablets of 47.5 mg metoprolol per day for cardiac arrhythmia as needed. She had previously been treated for occasional genital herpes simplex viral infections for over 10 years. Three years prior to the current presentation, a slowly growing perineal papule, approximately 10 mm in size, had been surgically removed. Histology showed a benign intradermal naevus.
The patient reported severe itching, stinging sensation, and intermittent rash in the gluteal cleft, perineum, and perianal region, with onset of symptoms 7 months previously. Ultrapotent or mid-potent corticosteroid creams alleviated the symptoms only slightly when used twice a day for 2–3 weeks.
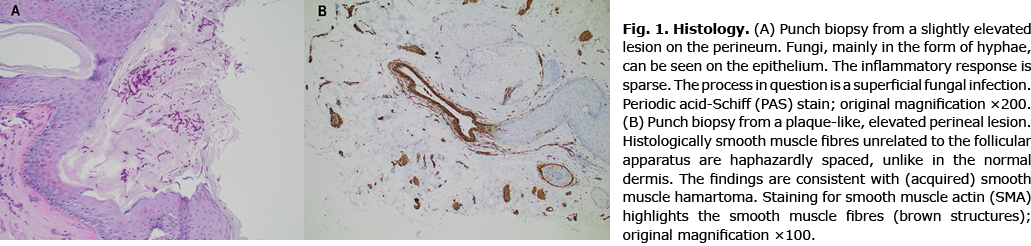
Physical examination revealed a round, swollen, erythematous plaque 20 mm in diameter in the perineum and only mild erythema in the gluteal cleft. A biopsy specimen was taken from the perineal lesion, and histopathological examination showed a fungal infection (Fig. 1A). The patient was treated with topical econazole-triamcinolone cream and oral itraconazole (100 mg daily) for 4 weeks. The symptoms were partially alleviated, but there was still a burning sensation in the perianal region and gluteal cleft (Fig. 2).
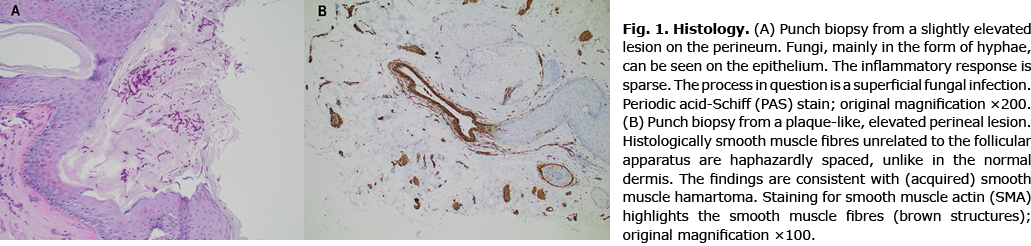

A new punch biopsy was taken from the perineum, where the physical examination showed slightly erythematous red plaques with small yellowish papules resembling irritated hair follicles (Fig. 2A). The biopsy showed intersecting smooth muscle cell strands in the reticular dermis (Fig. 1B). The histology was suspicious for vulvar smooth muscle hamartoma. The histology in a punch biopsy from the slightly erythematous perianal skin was negative for any notable changes. The first biopsy taken from the perineal skin was re-examined and showed smooth muscle cells in the dermis. Ultrasound did not show visible changes in the skin or subcutaneous fat of the perineum and gluteal cleft.
What is your diagnosis? See next page for answer.
Persistent Pain and Itch in Gluteal Cleft and Perineum: A Commentary
Acta Derm Venereol 2022; 102: adv00753.
DOI: 10.2340/actadv.v102.2436
Diagnosis: Atypical herpes simplex viral infection
The patient started regular treatment with valaciclovir (500 mg, 1 tablet daily). The symptoms completely subsided in 1 week. During the following 4 months, the patient twice felt a slight burning sensation returning. Using valaciclovir (500 mg, 1 tablet twice a day) for 3–4 days without any additional local treatment halted the symptoms again. The patient had been previously diagnosed with herpes simplex infection, but she had only used oral treatment when typical herpetic lesions appeared. Recurrent anogenital herpes simplex infection may not always present with typical erosions. Erythema, pruritus, or burning sensation may be the only symptoms (1).
Smooth muscle hamartoma (SMH) is a rare benign proliferative disorder of the smooth muscle. It usually arises from the arrector pili, vessel wall, mamillary, vulvar, or dartos muscles. Congenital SMH most often presents as a single patch in the lumbosacral area and may be confused with Becker’s hamartoma or congenital melanocytic naevus (2). Congenital SMHs are more common than acquired SMHs (3). There are no published cases of congenital vulvar SMH. In addition, vulvar acquired SMH is very rare, with only 2 cases reported in the literature (4, 5). The first patient had pruritic plaques and papules and was treated with antihistamines (4). The other patient had slight vulvar lichenification and experienced vulvar soreness, which was successfully treated with pain medication (5). There are no reports of a connection between herpes simplex viral infections and SMH in the literature.
In the scrotal area, acquired SMH is thought to result from lymphedema due to chronic lymphatic obstruction secondary to surgery, locoregional radiotherapy, trauma, or morbid obesity (3). It may be possible that the removal of the intradermal naevus 3 years previously caused a lymphatic obstruction leading to formation of the SMH. The patient had had no other treatments in the perineal area. Her body mass index (BMI) was 24 kg/m2 (normal).
The symptoms in this patient were concluded to result from recurrent, clinically atypical herpes simplex viral infection. The fungal infection was probably due to repeated courses of ultrapotent and mid-potent corticosteroid ointments. She also had smooth muscle cell bundles in perineal biopsies, possibly representing the third published case of acquired vulvar SMH.
REFERENCES
- Lautenschlager S, Eichmann A. The heterogeneous clinical spectrum of genital herpes. Dermatology 2001; 202: 211–219.
- Raboudi A, Litaiem N. Congenital smooth muscle hamartoma. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021. PMID: 31424772.
- Kawahira H, Fujii K, Yonezawa T, Osako Y, Kanekura T. Acquired smooth muscle hamartoma of the scrotum. J Dermatol 2022; 49: e20–e21.
- Kwon KS, Lee CW, Seo KH, Park JH, Oh CK, Jang HS, et al. Acquired vulvar smooth muscle hamartoma: a case report and review of the literature. J Dermatol 2000; 27: 56–59.
- Toeima E, Igali L, Saleh M. Acquired vulval smooth muscle hamartoma in a postmenopausal woman, with no visible lesion. J Obstet Gynaecol 2010; 30: 205–206.