The use of sunscreens is recommended to limit the impact of sun exposure on the skin. The objective of this study was to examine the relationship between sunscreen sales and melanoma in 4 different countries with diverse sunscreen regulations. Data from publicly available databases were examined for Sweden, England, Australia, and the USA from 1999 to 2018. The association between incidence of melanoma and sunscreen sales was estimated using a generalized estimating equation, and modelling was used to predict melanoma cases. Incidence of melanoma was positively associated with sunscreen sales in England, Australia, and the USA, and negatively associated with sunscreen sales in Sweden. Growth rates in melanoma cases of 0.42%, 16.7%, 19.1% and 12.2% were predicted for Sweden, England, Australia, and the USA, respectively. The differences observed between England, Australia, and the USA, on the one hand, and Sweden, on the other hand, are consistent with the adoption of strong regulations requiring the use of ultraviolet A blocking agents in sunscreens.
Key words: sunscreen; ultraviolet rays; ultraviolet A; melanoma; epidemiology.
Accepted Mar 17, 2021; Epub ahead of print Mar 18, 2021
Acta Derm Venereol 2021; 101: adv00480.
doi: 10.2340/00015555-3788
Corr: Samar Merhi, Department of Dermatology, Epidemiology in dermatology and evaluation of therapeutics (EpiDermE EA 7379, University Hospital Henri Mondor), University Paris-Est Créteil (UPEC), FR-94010 Créteil, France. E-mail: samar-merhi@hotmail.com
SIGNIFICANCE
The use of sunscreens is considered to be protective against skin cancer. These products should be used appropriately and manufactured with a ultraviolet A:ultraviolet B ratio of 1:3 in order to be protective, or else, as shown in this study, sunscreen might increase the risk of melanoma.
INTRODUCTION
Skin cancer is the most prevalent form of cancer. While melanoma accounts for only 1% of skin cancers, it causes the majority of deaths due to skin cancer worldwide (1, 2) and its incidence has been increasing in the USA and Europe (3, 4).
The aetiology of melanoma is complex, but research has estimated that exposure to ultraviolet (UV) radiation accounts for 70% of cases of melanoma (5, 6). As a result, public health officials recommend the use of sun-protective equipment, including sunscreen, to limit the impact of sun exposure on the skin (7). A meta- analysis assessing the relationship between melanoma and sunscreen use showed that the conclusions of different studies vary widely (8). However, all these studies rely on the subjects’ recollection regarding sunscreen application, rather than a non-biased measurement. A relatively recent ecological study by Williams et al. (9) showed that incidence of melanoma is positively associated with income and sunscreen sales, while controlling for UV exposure. Ecological studies compare incidences or rates of a disease at the population level rather than at an individual level. Their work, however, does not describe inter-country variations, as is provided in the current study.
The aim of this ecological study was to assess the relationship between sunscreen sales and incidence of melanoma in 4 countries with different sunscreen regulations, while adjusting for UV and income. Over the past 5 years, there has been a strong emphasis on the development of so-called “broad-spectrum” sunscreens, which block both UVB and UVA. However, to date, there is little evidence to support their success at an epidemiological level.
MATERIALS AND METHODS
England, Sweden, Australia, and the USA were selected for several reasons. First, they have similar sex ratios, a high proportion of people with skin type I, and have publicly-available incidence of melanoma and UV data. Secondly, these countries follow distinct legislation for sunscreen manufacturing and labelling.
UV index
UV irradiance data were obtained from government-run UV-index instruments: the Swedish Meteorological and Hydrological Institute, the Department of Environment Food and Rural Affairs in the UK, the Australian Radio Protection And Nuclear Safety Agency, and the National Oceanic and Atmospheric Administration in the USA. The maximum UV index per day for each UV-index measuring instrument was obtained. Mean UV index per calendar year and median UV index for each country were calculated.
Melanoma incidence
Melanoma incidence data were obtained from government-run databases: Sweden’s National Board of Health and Welfare, the Office for National Statistics in the UK, the Australian Institute of Health and Welfare, and the United States Center for Disease Control and Prevention. For a given year, the melanoma incidence crude rate was calculated by dividing the number of new cases by the total population in the same year.
Sunscreen sales
Sunscreen sales, expressed in litres, were obtained for the years 1999 to 2018, and sunscreen sales projections (2020–2023) from Euromonitor International, a company specializing in market research data (http://www.euromonitor.com). To compare sunscreen sales across countries for a given year, sunscreen sales by the population of the country in that year was normalized and this ratio multiplied by 100,000 (final unit: litres per 100,000 people). For the case of England, Euromonitor provides sunscreen sales for the UK only, and therefore to estimate sales for England, this study examined the pro-rata amount by population.
Income data
Income data were obtained from the World Bank database, expressed as gross domestic product per capita in constant 2011 international dollars purchasing power parity (GDP-PPP).
Statistical analysis
The least-squares method was used to estimate trends in incidence of melanoma, UV index, sunscreen sales, and GDP-PPP from 2004 to 2018.
To assess the relationship between each independent variable and incidence of melanoma, a bivariate analysis was performed using generalized estimating equations (GEE) on all countries pooled together and on each country separately. Furthermore, multivariable analysis was performed using GEE to evaluate the association between incidence of melanoma and sunscreen sales. Since the latency period between exposure and development of melanoma is approximately a decade (10), the values of sunscreen sales for a specific year were taken as the independent variable, controlled for the yearly mean UV index and GDP-PPP while considering 2- and 9-year gaps in melanoma data, as the dependent variable. Two- and 9-year gaps were the closest and widest feasible ranges for the statistical analysis in view of the available data.
Unstandardized regression coefficient beta was generated from GEE analysis and used in calculation of the forecast incidence of melanoma in the different countries.
IBM SPSS Statistics for Windows, version XXI (IBM Corp., Armonk, NY, USA) was used for statistical analysis, and significance level was set at α=0.05.
RESULTS
Descriptive analysis
Fig. 1 shows the UV index variation over the years in Sweden, England, Australia, and the USA. The highest UV index mean was found in Australia (6.66 ± 0.31) and the lowest in Sweden (0.32 ± 0.01). There is no clear pattern of increase in UV Index in Sweden, England, and Australia (p > 0.05); however, there was an increasing trend of UV index in the USA (β = 0.047; p < 0.001).

The highest sunscreen sales were in the USA (9,836.05 ± 1,448.632 liters per 100,000 population) and the lowest in Sweden (5,370.14 ± 1,269.94 liters per 100,000 population). Fig. 1 shows the by-country increase in normalized sunscreen sales. The mean yearly increase rates were 4.9%, 2.3%, 5.6%, and 2.7% in Sweden, England, Australia, and the USA, respectively. Trends analysis of sunscreen sales in the different countries showed a significant increase in Sweden, England, Australia, and the USA (p = 0.011, 0.001, < 0.001, < 0.001, respectively). Furthermore, the analysis showed a significant increase in overall sunscreen sales (p ≤ 0.001).
A significant increase in GDP-PPP was found at the level of all countries. The USA has the highest GDP-PPP, and England has the lowest GDP-PPP (mean 49,852.39 ± 3,103.72 and 34,340.2 ± 1,240.365 USD ($), respectively).
The highest melanoma crude rate was found in Australia (mean 58.30 ± 18.26 liters per 100,000 population) and the melanoma crude rate increases over time in all countries, with a mean of 7% in Sweden, 1.6% in England,12.5% in Australia, and 4.4% in the USA (Fig. 1). Furthermore, the trend was found to be positively significant (p < 0.001) in the whole sample.
Relationship between crude rate of melanoma and other parameters
Multiple GEE analysis was performed to assess the association between incidence of melanoma as the dependent variable and UV index, sunscreen sales, and income separately. At the 2-year gap, the results showed a significant relationship between melanoma and UV in the overall sample, Australia and the USA (β = 2.508, 39.266, 6.11; p = 0.005, < 0.001, < 0.001, respectively), and a non-significant association in Sweden and England. Furthermore, melanoma was positively significantly associated with GDP-PPP in all countries for a 9-year gap (β = 0.002, 0.001, 0.006 and 0.001; p < 0.001)). In addition, melanoma was positively associated with sunscreen in Sweden (β = 0.003, p = 0.002), Australia (β = 0.012, p < 0.001) and the USA (β = 0.002, p < 0.001) for a 2-year lapse and in all countries for a 9-year lapse (β = 0.003, 0.002, 0.01, 0.002; p < 0.001) (Table I).

Similarly, this study used a GEE model to estimate the relationship between melanoma and sunscreen sales while adjusting for UV index and income as confounders. multicollinearity was found between sunscreen sales and income in the overall sample, and in England, Australia, and the USA individually for a 2-year gap, and in all countries for a 9-year gap. Therefore, the income was removed from the overall and country-specific 9-year gap analysis for Sweden, England, Australia, and the USA.
The results are summarized in Table II. A positive association was found between melanoma and sunscreen sales for 2- and 9-year gaps (odd ratio (OR) 1.00, 1.003; p = 0.011, < 0.001, respectively) in the overall sample after controlling for UV and GDP-PPP. In the 2-year gap analysis, a significant positive association was demonstrated for England, Australia, and the USA (OR 1.006, 1.012, 1.002; p = 0.014, < 0.001, < 0.001; respectively). However, a significant inverse association was found in Sweden (OR 0.998, p < 0.001). In the 9-year gap analysis, a significant positive association was found for all countries (OR 1.003, 1.001, 1.001 and 1.002; p < 0.001, respectively). In other words, an increase in 1 liter per 100,000 population in sunscreen sales increases the risk of melanoma by 0.3%, 0.1%, 0.1% and 0.2% in Sweden, England, Australia, and the USA, respectively.

Predictive model
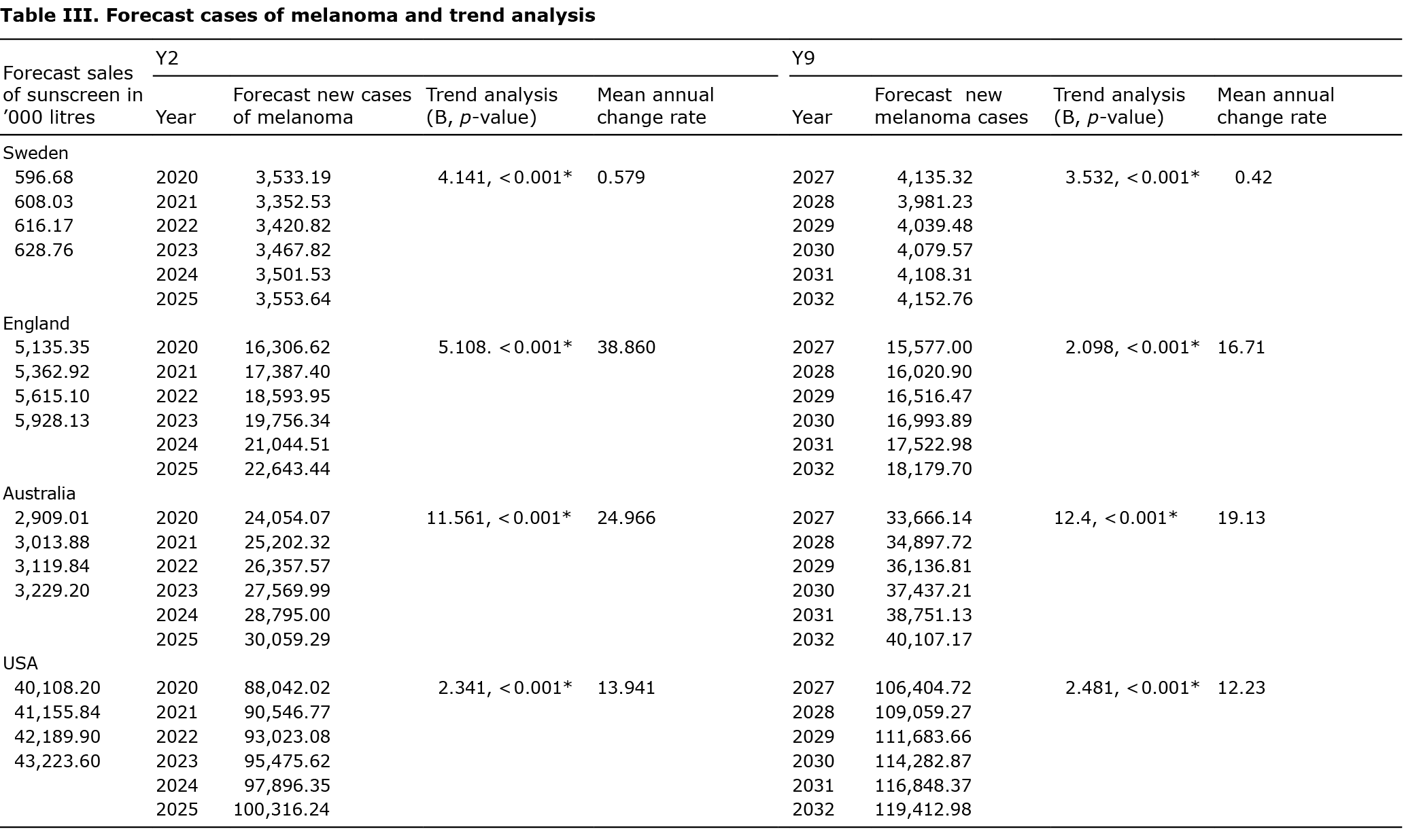
Unstandardized beta from GEE analysis between incidence of melanoma and sunscreen was used to predict melanoma cases in each country for the years 2020 to 2023 based on the sunscreen predictions retrieved from Euromonitor. The results of the analysis are shown in Table III. In fact, a significant increase in melanoma cases is expected from 2020 to 2023 in Sweden, England, Australia, and the USA for a 2-year gap and from 2027 to 2032 for a 9-year gap.
DISCUSSION
This study examined the association between sunscreen sales and melanoma rates in 4 developed countries with different legislation on UVA-protection sunscreens; England, Australia, Sweden, and the USA, between 1999 and 2018.
The results show that incidence of melanoma is positively associated with sunscreen sales, after controlling for the UV index in Sweden, England, Australia, and the USA for a 9-year gap; however, incidence of melanoma is negatively associated with sunscreen sales in Sweden for a 2-year gap.
Similarly to other studies, the current results show a significant association between incidence of melanoma and UV index in Australia and the USA, but not in England and Sweden (11, 12). A previous study conducted in 20 different countries found a negative correlation between incidence of melanoma and latitude (higher UV index). However, no clear pattern was observed in European countries, including Sweden and England (13). The significant increase in the UV trend in the USA may be due to the high consumption of ozone-depleting substances compared with European countries and Australia, leading to increased penetration of UV rays (14). Furthermore, in line with experimental studies, the current study found that sun exposure and cumulative UV radiation accelerate the appearance and development of melanoma (15).
The current study also found a positive relationship between melanoma and GDP-PPP; which increases with income (16), similar to findings from other studies (17). Previous studies have found that people with higher education, higher income, and lower unemployment had higher incidence of melanoma (9, 18). This association may be related to the fact that, in countries with higher income, people have more money to spend on activities such as tanning beds or vacations in warmer climates (19, 20). Furthermore, awareness of cancer and access to screening tests is higher in wealthy societies, and wealthier individuals are more likely to see a dermatologist and to diagnose pigmented lesions early (21), which would increase the incidence of melanoma recorded among people of this socio-economic status. In addition, high sunscreen sales were directly related to vacations and holidays, and hence to wealthier populations (22).
A significant increase in incidence of melanoma was also found with higher sunscreen sales in Sweden, England, Australia, and the USA in the 9-year gap analysis. However, this association was inversed in Sweden for the 2-year gap analysis. The relationship between melanoma and sunscreen is highly controversial; while some studies showed a protective effect of the latter, others depicted a positive or no relationship. Different meta-analysis, including case-control studies, cohorts, and cross-sectional studies, did not show any significant association between melanoma and sunscreen use (8, 23–25). In line with these findings, many studies suggest that sunscreen use might increase melanoma risk by encouraging users for longer sunbathing and hence for more UV exposure. This is reinforced by randomized trials and meta-analysis, showing that people who use higher sun-protection factor (SPF) sunscreens sunbathe more than those who use lower SPF (26, 27). It is notable that the majority of the population in the 4 studied countries have sensitive skin that burns easily; people with this skin type are at higher risk of developing melanoma and use more sunscreen than people with skin that tans but does not burn (28).
Sunscreen with a majority of UVB filters could provide users with a false sense of protection since individuals will be less likely to burn, while, in parallel, increasing exposure to UVA (29). Regulatory guidelines in the European Union recommend a minimum UVA to UVB ratio of 1:3, since 2012, for all marketed sunscreen products (30). At the same time, in the USA and Australia, regulators did not impose any ratio (31, 32). Recently, however, the US Food and Drug Administration (US) FDA and the Australian government have started reviewing these guidelines (33). The use of a UVA:UVB ratio of 1:3 in Sweden, as per the European guidelines, is the major regulatory difference between the studied countries; this may at least partially explain the results from Sweden in the current study. In fact, a protective effect of sunscreens was found when considering a 2-year gap, where sunscreen data ranged from 1999 to 2018, including years after 2012 in which the new regulations were established; however, sunscreens were shown to be a risk factor for the 9-year gap analysis, where sunscreen data were considered only from 1999 to 2009. In fact, in the latter period, i.e. 1999–2009, the regulation imposing a UVA:UVB ratio of 1:3 was still not effective. Furthermore, this finding is reinforced by the predictive model where the increase in melanoma rate decreased from a mean of 7% (1999–2018) to 0.6% (2020 to 2025) in Sweden, while it increased from 1.6% to 39% in England, 12.5% to 25% in Australia, and 4.4% to 14% in the USA for the same time-period. Indeed, UVA (315–400 nm) penetrates deeper than UVB into the skin, through the epidermis and dermis, releasing highly mutagenic reactive oxygen species. Furthermore, 90% of UVA reaches the earth and can pass through windows and fabrics and remains constant throughout the year, whereas 10–15% of UVB reaches the surface mostly in summer (34–36). For this reason, higher protection against UVA is as essential as UVB filters in sunscreens for prevention from melanoma. The risk/benefit ratio of the use of sunscreen should always be weighed carefully, as a recent study has pointed out the risk of systemic exposure of active ingredients with possible endocrine-disrupting effects (avobenzone, oxybenzone, octocrylene, and ecamsule) in sunscreen products under recommended usage conditions (37). Several studies have found a protective effect of sunscreen use on incidence of melanoma; however, these studies have many biases, including sampling bias, recall bias on UV exposure and an imprecise definition and patterns of “sunscreen use”. Furthermore, the protective effect of sunscreens in melanoma was shown among individuals who “optimally” used sunscreens. In contrast, optimal sunscreen use (multiple application, full skin coverage, etc.) is not routinely followed due to the lack of knowledge.
Finally, despite the fact that UV is a well-known risk factor for melanoma (5, 6, 38), only a few studies controlled for this confounder. In fact, among all cited references, and studies that were included in the meta-analysis, only Savoye et al. (39) used a self-completed questionnaire on UV, Ghiasvand et al. (40) assessed exposure at different latitudes, and Klug et al. (41) adjusted for UVB intensity of residences.
The current study has several limitations. First, it only describes associations, not causations. Secondly, melanoma was assessed using crude rates, not age-standardized rates, for better comparability between the 4 countries; this would overestimate the disease incidence. Thirdly, this study did not consider the types of melanoma and pathology details; in fact, early diagnosis due to awareness campaigns lead to higher incidence of melanoma. Moreover, sunscreen sales were used as a whole without age or SPF specifications, due to a lack of availability of such information. Furthermore, this is an ecological study and cannot adjust for potential individual confounders. Finally, the study is limited by the availability of data from 2004 to 2018 in terms of incidence of melanoma, sunscreen sales, UV index and GDP (PPP); a more extensive timeline would be more representative. To the best of our knowledge, this is the first ecological multinational study to assess the relationship between incidence of melanoma and sunscreen sales while controlling for UV index. Secondly, official national data were used to estimate the incidence of melanoma and UV index, leading to more reliable results. Furthermore, an essential confounder was included; the yearly mean UV index, which was not controlled for in previous studies.
This study suggests that legislation requiring sunscreen to block UVA has a positive impact on the incidence of melanoma. More research, using age-standardized sunscreen sales for a longer timeframe, is needed, especially in less developed countries. Furthermore, additional awareness campaigns on the correct and optimal use of sunscreens are required in order to minimize intentional sunbathing associated with sunscreen use.
ACKNOWLEDGEMENTS
This study used publicly available data, and is thus exempt from requiring ethics approval.
The authors are grateful to ELDP for acquiring the sunscreen sales from Euromonitor International.
PK, SB and ELPD were, or are still, employees of Shade, a company manufacturing wearable UV sensors.
The other authors have no conflicts of interest to declare.
REFERENCES
- Matthews NH, Li W-Q, Qureshi AA, Weinstock MA, Cho E. Epidemiology of Melanoma. In: Ward WH, Farma JM, editors. Cutaneous melanoma: etiology and therapy. Brisbane (AU): Codon Publications; 2017 [cited 2019 Dec 11]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK481862/.
- Melanoma Skin Cancer Statistics. The American Cancer Society. [cited 2019 Sep 20]. Available from: https://www.cancer.org/cancer/melanoma-skin-cancer/about/key-statistics.html.
- Melanoma of the Skin – Cancer Stat Facts. SEER. [cited 2020 May 20]. Available from: https://seer.cancer.gov/statfacts/html/melan.html.
- Sacchetto L, Zanetti R, Comber H, Bouchardy C, Brewster DH, Broganelli P, et al. Trends in incidence of thick, thin and in situ melanoma in Europe. Eur J Cancer 2018; 92: 108–118.
- Dimitriou F, Krattinger R, Ramelyte E, Barysch MJ, Micaletto S, Dummer R, et al. The world of melanoma: epidemiologic, genetic, and anatomic differences of melanoma across the globe. Curr Oncol Rep 2018; 20: 1–9.
- Koh HK, Geller AC, Miller DR, Grossbart TA, Lew RA. Prevention and early detection strategies for melanoma and skin cancer: current status. Arch Dermatol 1996; 132: 436–443.
- Saraiya M, Glanz K, Briss P, Nichols P, White C, Das D; Task Force on Community Preventive Services On reducing Exposure to Ultraviolet Light. Preventing skin cancer: findings of the Task Force on Community Preventive Services On reducing Exposure to Ultraviolet Light. MMWR Recomm Rep. 2003; 52: 1–12.
- Silva ES da, Tavares R, Paulitsch F da S, Zhang L. Use of sunscreen and risk of melanoma and non-melanoma skin cancer: a systematic review and meta-analysis. Eur J Dermatol 2018; 28: 186–201.
- Williams SN, Dienes KA. Sunscreen sales, socio-economic factors, and melanoma incidence in Northern Europe: a population-based ecological study. SAGE Open 2014; 4: 2158244014559023.
- Liu T, Soong SJ. Epidemiology of malignant melanoma. Surg Clin North Am 1996; 76: 1205–1222.
- Eide MJ, Weinstock MA. Association of UV index, latitude, and melanoma incidence in nonwhite populations – US Surveillance, Epidemiology, and End Results (SEER) Program, 1992 to 2001. Arch Dermatol 2005; 141: 477–481.
- Rivas M, Rojas E, Calaf GM. Prediction of skin cancer occurrence by ultraviolet solar index. Oncol Lett 2012; 3: 893–896.
- Stang A, Becker JC, Nghiem P, Ferlay J. The association between geographic location and incidence of Merkel cell carcinoma in comparison to melanoma: an international assessment. Eur J Cancer 2018; 94: 47–60.
- United Nations Statistics division – environment statistics. [cited 2021 Jan 20]. Available from: https://unstats.un.org/unsd/environment/ODS_Consumption.htm.
- Romerdahl CA, Donawho C, Fidler IJ, Kripke ML. Effect of ultraviolet-B radiation on the in vivo growth of murine melanoma cells. Cancer Res 1988; 48: 4007–4010.
- The Relationship between Income, Consumption and GDP: a time series, cross-country analysis. Proc Econ Finan 2015; 23: 1535–1543.
- Idorn LW, Wulf HC. Socioeconomic status and cutaneous malignant melanoma in Northern Europe. Br J Dermatol 2014; 170: 787–793.
- Singh SD, Ajani UA, Johnson CJ, Roland KB, Eide M, Jemal A, et al. Association of cutaneous melanoma incidence with area-based socioeconomic indicators – United States, 2004–2006. J Am Acad Dermatol 2011; 65: S58–S68.
- Bentham G, Aase A. Incidence of malignant melanoma of the skin in Norway, 1955–1989: associations with solar ultraviolet radiation, income and holidays abroad. Int J Epidemiol 1996; 25: 1132–1138.
- Pérez-Gómez B, Aragonés N, Gustavsson P, Lope V, López-Abente G, Pollán M. Socio-economic class, rurality and risk of cutaneous melanoma by site and gender in Sweden. BMC Publ Health 2008; 8: 33.
- Johnson-Obaseki SE, Labajian V, Corsten MJ, McDonald JT. Incidence of cutaneous malignant melanoma by socioeconomic status in Canada: 1992–2006. J Otolaryngol Head Neck Surg 2015; 44: 53.
- Kojo K, Jansen CT, Nybom P, Huurto L, Laihia J, Ilus T, et al. Population exposure to ultraviolet radiation in Finland 1920–1995: exposure trends and a time-series analysis of exposure and cutaneous melanoma incidence. Environ Res 2006; 101: 123–131.
- Rueegg CS, Stenehjem JS, Egger M, Ghiasvand R, Cho E, Lund E, et al. Challenges in assessing the sunscreen-melanoma association. Int J Cancer 2019; 144: 2651–2668.
- Xie F, Xie T, Song Q, Xia S, Li H. Analysis of association between sunscreens use and risk of malignant melanoma. Int J Clin Exp Med 2015; 8: 2378–2384.
- Guide to the development, evaluation and implementation of clinical practice guidelines. National Health and Medical Research Council. [cited 2020 Mar 26]. Available from: https://www.nhmrc.gov.au/about-us/publications/guide-development-evaluation-and-implementation-clinical-practice-guidelines.
- Autier P, Boniol M, Doré J-F. Sunscreen use and increased duration of intentional sun exposure: still a burning issue. Int J Cancer 2007; 121: 1–5.
- Autier P, Doré J-F, Reis AC, Grivegnée A, Ollivaud L, Truchetet F, et al. Sunscreen use and intentional exposure to ultraviolet A and B radiation: a double-blind randomized trial using personal dosimeters. Br J Cancer 2000; 83: 1243–1248.
- Wheless L, Ruczinski I, Alani RM, Clipp S, Hoffman-Bolton J, Jorgensen TJ, et al. The association between skin characteristics and skin cancer prevention behaviors. Cancer Epidemiol Biomarkers Prev 2009; 18: 2613–2619.
- Jansen R, Osterwalder U, Wang SQ, Burnett M, Lim HW. Photoprotection: part II. Sunscreen: development, efficacy, and controversies. J Am Acad Dermatol 2013; 69: 867.e1-14; quiz 881–2.
- Commission Recommendation of 22 September 2006 on the efficacy of sunscreen products and the claims. Official Journal of the European Union 2006; 265. Available from: http://data.europa.eu/eli/reco/2006/647/oj/eng.
- Labeling and effectiveness testing: sunscreen drug products for over-the-counter human use — small entity compliance guide. US Food and Drug Administration (FDA); 2019 [cited 2020 Mar 28]. Available from: http://www.fda.gov/regulatory-information/search-fda-guidance-documents/labeling-and-effectiveness-testing-sunscreen-drug-products-over-counter-human-use-small-entity.
- Australian regulatory guidelines for sunscreens. Australian Government Department of Health- Therapeutic Goods Administration; 2019 [cited 2020 Mar 28]. Available from: https://www.tga.gov.au/publication/australian-regulatory-guidelines-sunscreens-args.
- Wang SQ, Lim HW. Highlights and implications of the 2019 proposed rule on sunscreens by the US Food and Drug Administration. J Am Acad Dermatol 2019; 81: 650–651.
- Wang SQ, Setlow R, Berwick M, Polsky D, Marghoob AA, Kopf AW, et al. Ultraviolet A and melanoma: a review. J Am Acad Dermatol 2001; 44: 837–846.
- Latha MS, Martis J, Shobha V, Sham Shinde R, Bangera S, Krishnankutty B, et al. Sunscreening agents. J Clin Aesthet Dermatol 2013; 6: 16–26.
- Kamenisch Y, Ivanova I, Drexler K, Berneburg M. UVA, metabolism and melanoma: UVA makes melanoma hungry for metastasis. Exp Dermatol 2018; 27: 941–949.
- Matta MK, Florian J, Zusterzeel R, Pilli NR, Patel V, Volpe DA, et al. Effect of sunscreen application on plasma concentration of sunscreen active ingredients: a randomized clinical trial. JAMA 2020; 323: 256–267.
- National Institutes of Health summary of the Consensus Development Conference on Sunlight, Ultraviolet Radiation, and the Skin. Bethesda, MD, May 8–10, 1989. Consensus Development Panel. J Am Acad Dermatol 1991; 24: 608–612.
- Savoye I, Olsen CM, Whiteman DC, Bijon A, Wald L, Dartois L, et al. Patterns of ultraviolet radiation exposure and skin cancer risk: the E3N-SunExp Study. J Epidemiol 2018; 28: 27–33.
- Ghiasvand R, Weiderpass E, Green AC, Lund E, Veierød MB. Sunscreen use and subsequent melanoma risk: a population-based cohort study. JCO 2016; 34: 3976–3983.
- Klug HLP, Tooze JA, Graff-Cherry C, Anver MR, Noonan FP, Fears TR, et al. Sunscreen prevention of melanoma in man and mouse. Pigment Cell Melanoma Res 2010; 23: 835–837.