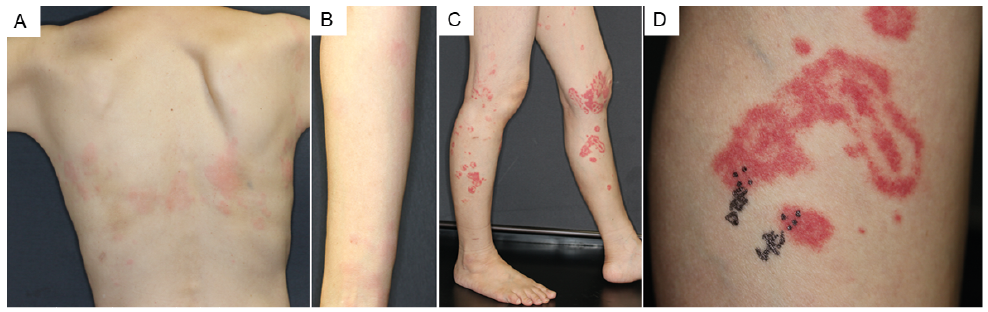
Fig. 1. (A) Erythema on the back. (B, C) Erythema gyratum repens-like eruptions on the lower limbs. (D) Erythema on the upper limb.
1Departments of Dermatology, Kyoto University Graduate School of Medicine, 54 Shogoin Kawahara-cho, Sakyo, Kyoto 606-8507, Japan, and 2Singapore Immunology Network (SIgN) and Skin Research Institute of Singapore (SRIS), Agency for Science, Technology and Research (A*STAR), Singapore, Singapore. *E-mail: gyohei@kuhp.kyoto-u.ac.jp
A 55-year-old woman had a 2-day history of multiple annular eruptions on her lower limbs (Fig. 1A, B). These eruptions started with pruritic erythema and then developed into annular purpura and presented with erythema gyratum-like manifestation. The patient also had pruritic erythema, but no purpura on her back (Fig. 1C) and upper limbs (Fig. 1D). She had been diagnosed with Sjögren’s syndrome when she was 35 years old based on dry eye, dry mouth, and seropositivity for antinuclear antibody and SS-A. Since then, she had been followed up without any treatment. Laboratory examinations revealed a high titre of IgG (1,948 mg/dl; normal, 870–1,700 mg/dl). Serum C3 and C4 levels were normal.
What is your diagnosis? See the next page for the answer.
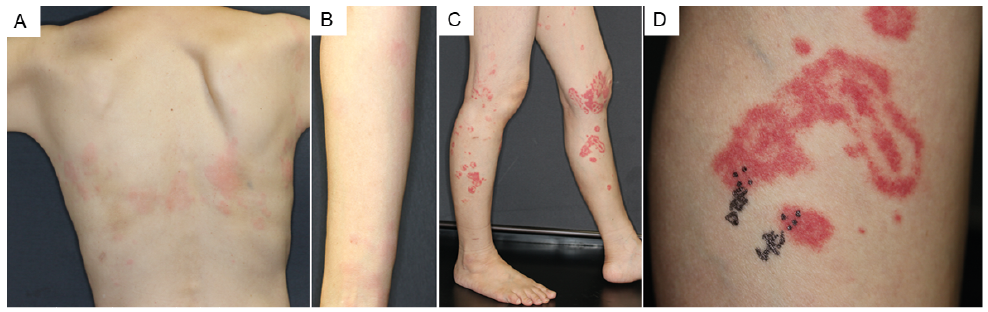
Fig. 1. (A) Erythema on the back. (B, C) Erythema gyratum repens-like eruptions on the lower limbs. (D) Erythema on the upper limb.
Acta Derm Venereol 2020; 100: adv00227.
Diagnosis: Urticarial vasculitis
Histological examination from the purpura on the left leg revealed perivascular infiltration of neutrophils, nuclear dusts, extravasated red blood cells, and fibrin deposition on vascular walls (Fig. 2A and B), suggesting the presence of leukocytoclastic vasculitis. No deposition of IgG/A and C3 was detected with direct immunofluorescence assay (data not shown). With the application of topical steroids, all of the eruptions disappeared in a few days. No recurrence of the eruptions or malignancy has been observed until now. Based on these clinical and histological manifestations, the patient was diagnosed with urticarial vasculitis, which mimicked erythema gyratum repens, occurring in a patient with Sjögren’s syndrome.
Sjögren’s syndrome is a chronic autoimmune disease that causes inflammation of the exocrine glands. Its skin manifestation is usually variable, and cutaneous vasculitis is one of the most common eruptions (1). Erythema gyratum repens is characterized by concentric erythematous rings that present a wood-grain appearance. This rash is generally considered as paraneoplastic and is sometimes associated with a variety of malignancies, most notably lung cancer and, less commonly, oesophageal, breast, and stomach cancers (2). In rare cases, erythema gyratum repens has also been associated with drugs, infectious diseases, and connective tissue diseases (3). In the current case, since the patients were not taking any medication and had no preceding infectious diseases, the eruptions on her back and legs were considered to be a series of rashes related to Sjögren’s syndrome.
A previous study showed that 89 of 558 (16%) patients with primary Sjögren’s syndrome presented with skin lesions (1). The most common skin lesion was cutaneous vasculitis, which was seen in 52 cases (58%); and among them, 11 patients presented with urticarial vasculitis. Urticarial vasculitis sometimes represents purpura and, similar to the current case, the development of erythema gyratum repens-like eruptions has also been reported (4). In the current case, the eruptions disappeared within several days and histological findings showed the existence of leukocytoclastic vasculitis, which was consistent with urticarial vasculitis.
How erythema gyratum repens represents such a unique skin manifestation remains unknown, but the involvement of immunoglobulins has been hypothesized. This is supported by the fact that granular deposition of IgG/C3 is sometimes detected by direct immunofluorescence of the skin in erythema gyratum repens (3). In the current case, purpura developed only at the lower limbs, similar to IgA vasculitis; however, no deposition of IgG/A and C3 was detected, suggesting that vasculitis was caused independent of immunoglobulin deposition.
Accumulation of further cases and laboratory results should be necessary to elucidate the pathogenesis of ery-thema gyratum repens-like eruption in Sjögren’s syndrome.
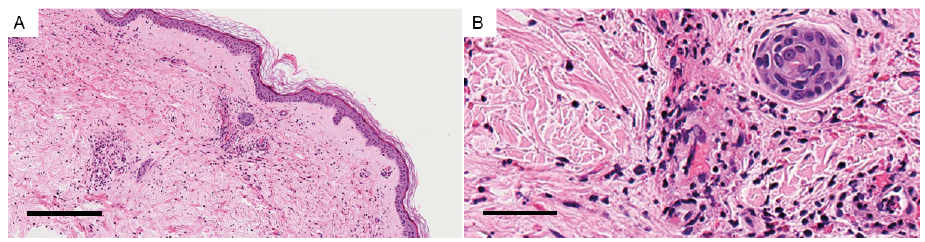
Fig. 2. (A, B) Histological analysis with haematoxylin and eosin staining from the left leg. Histopathology, showing perivascular infiltration of neutrophils, nuclear dusts, extravasated red blood cells, and fibrin deposition on vascular walls. Highly magnified view of perivascular area is shown in (B). Scale bar: (A) 250 µm and (B) 50 µm.