Dystrophy and Yellowish Discolouration of a Finger-nail in a 22-month-old Infant: A Quiz
Gi Ung Ha, Yong Hyun Jang and Jun Young Kim*
Department of Dermatology, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, 130 Dongdeok-ro, Jung-gu, Daegu 41944, South Korea. *E-mail: 198kjy@hanmail.net
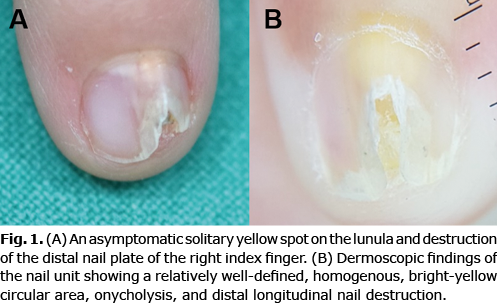
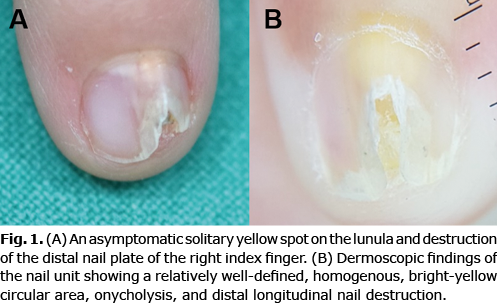
A 22-month-old female infant presented with distal dystrophy of the nail plate of her right index finger, which had persisted for 5 months. The nail also showed longitudinal ridging, onycholysis, and a small yellow spot on the lunula (Fig. 1A). She did not have any underlying diseases. No symptoms and signs, including itching, oozing, pain, and tenderness, were reported. Dermoscopy showed the presence of a relatively well-defined homogenous, bright-yellow circular area in the proximal area of the nail plate (Fig. 1B). Ultrasound revealed a 4.4×1.9×3.4-mm soft-tissue mass with calcified spots between the nail and the distal phalangeal bone. However, no specific bony abnormalities were identified on finger X-ray, and no abnormal laboratory results associated with calcium metabolism were obtained.
What is your diagnosis? See next page for the answer.
Dystrophy and Yellowish Discolouration of a Finger-nail in a 22-month-old Infant: A Commentary
Acta Derm Venereol 2022; 102: adv00778.
DOI: 10.2340/actadv.v102.2478
Diagnosis: Subungual juvenile xanthogranuloma
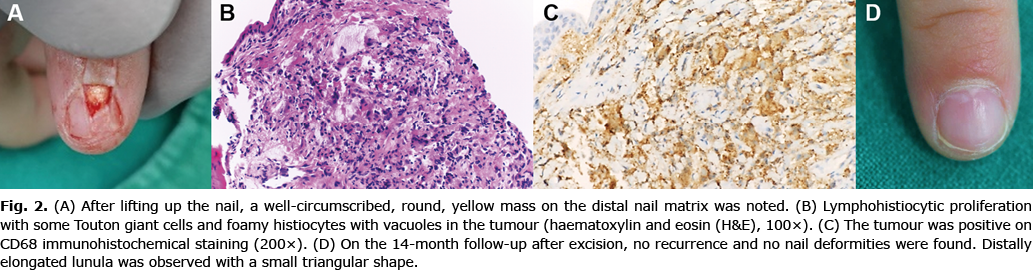
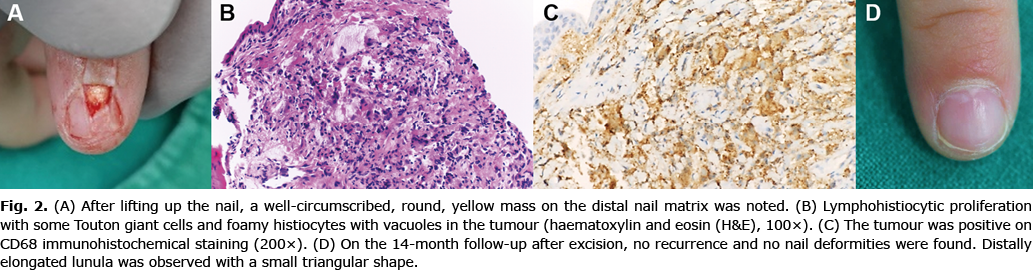
Excisional biopsy was performed to obtain an accurate diagnosis and to repair the nail deformity. Under general anaesthesia, her nail was lifted up using the window technique, revealing a well-defined, round, yellow mass (Fig. 2A). The mass was located above the distal nail matrix, and was completely removed. Histological analysis of the excised tissue showed dense lymphohistiocytic proliferation and some Touton giant cells and foamy histiocytes with vacuoles in the tumour (Fig. 2B). On immunohistochemical staining, the tumour was found to be positive for CD68 (Fig. 2C), but negative for S-100 and cytokeratin. A diagnosis of subungual juvenile xanthogranuloma (JXG) was made. Fourteen months after the surgery, a distally elongated lunula was observed with a small triangular shape, without recurrence or sequelae, including nail deformity or onycholysis (Fig. 2D).
Various subungual tumours that can cause nail deformities in children include epidermal cyst, subungual exostosis, haemangioma, and pyogenic granuloma. An epidermal cyst rarely involves the subungual area, but is almost always accompanied by a history of trauma. A subungual exostosis mainly involves the great toenails. Not only the bone, but also the bony tumour, is visible on X-ray. A subungual haemangioma can involve any soft tissue, but shows a purple-reddish colour change, which disappears when compression is applied. A pyogenic granuloma is a solitary mass with a bright-red colour, which bleeds easily.
This case was distinguished from all of the above- mentioned conditions. Nail deformity was noted, but it was an asymptomatic and proximally located yellow subungual mass in a young child. The tumour was diagnosed as JXG on histological examination. However, the dermoscopic findings did not correspond to JXGs in other locations, which have a red-yellow centre, discrete erythematous halo, or branched telangiectasia (1). The authors hypothesized that the tumour was compressed by the nail, and the vascular component disappeared on dermoscopic evaluation.
JXG is a type of non-Langerhans cell histiocytosis. It usually presents on the face, neck, and upper trunk, but rarely on the nail units (2, 3). JXG lesions undergo spontaneous involution over a period of 3–6 years, but if any cosmetic concern or risk to vital functions exists, the lesion should be treated (4). The treatment of choice of cutaneous JXG is surgical excision, and CO2 laser, intralesional steroid injection, cryotherapy, or low-dose radiotherapy are treatment alternatives (3). However, the subungual area is a rare location for JXG. Furthermore, accurate diagnosis is sometimes difficult because of the subungual location of the tumour and due to concerns about cosmetic disfigurement, i.e. the potential for the nail deformity to become more severe; subungual JXGs often need surgical excision.
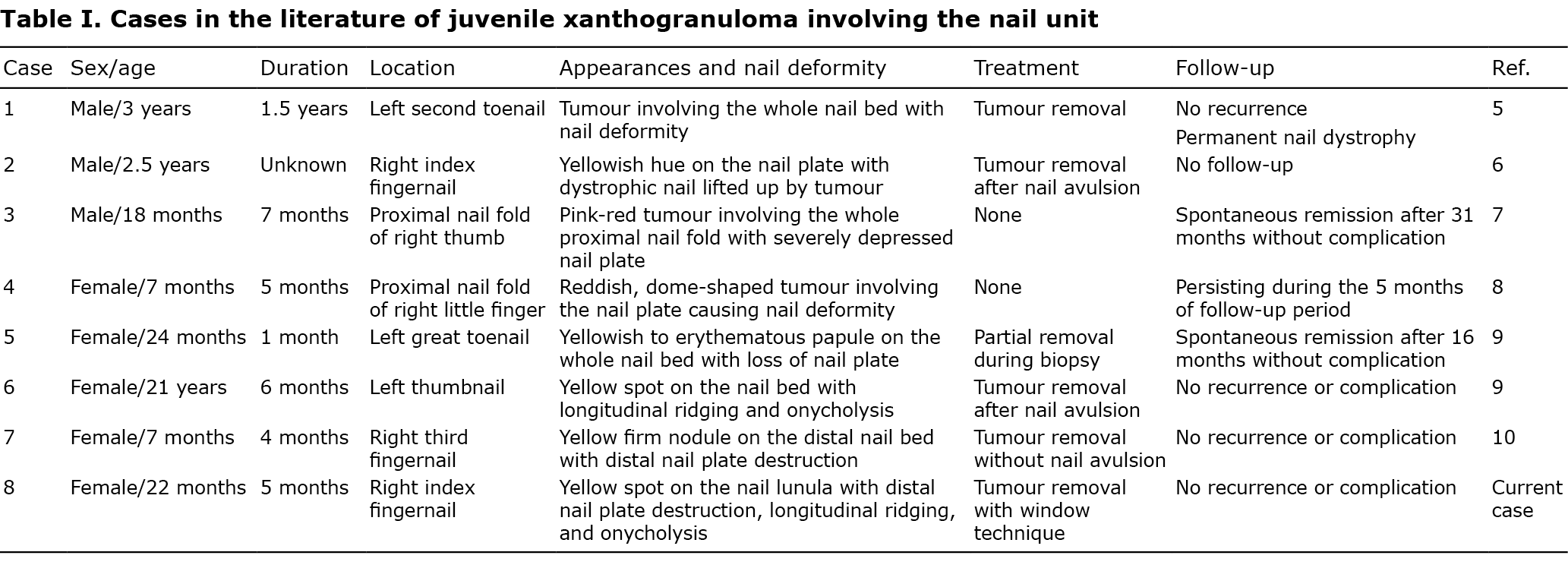
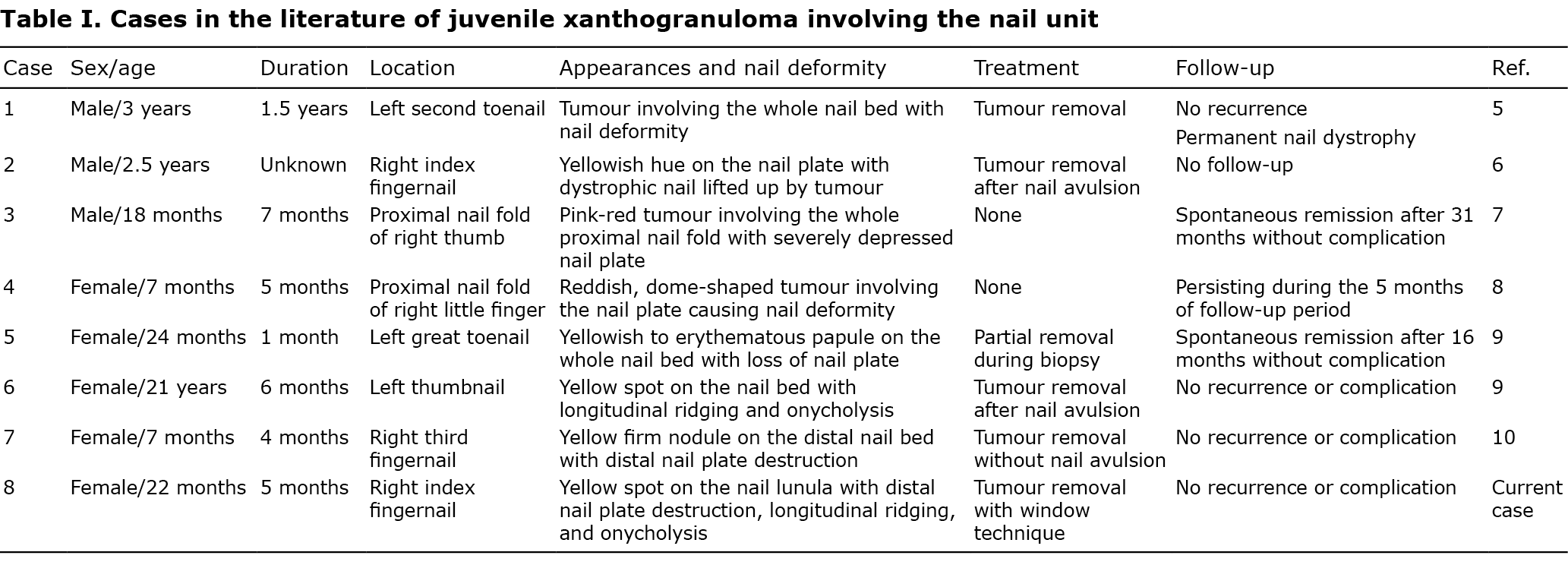
Including this case, only 8 cases (5–10) of JXG involving the nail unit have been reported, as summarized in Table I. These cases mainly involved children under 3 years of age (3 males and 5 females). Nail deformity was observed in all patients, and yellow lesions were noted in 5 of the 8 cases. All patients visited a hospital and received a diagnosis within 7 months. The timely hospital visit in each case was a result of changes in the appearance of the nail unit area due to the tumours. Three cases of subungual JXGs were not treated, whereas tumour removal was performed in the other 5. Of the 3 cases in which the tumour was not treated, spontaneous remission was observed in 2 cases, at 16 and 31 months. Of the 5 cases in which the tumour was removed, 4 cases did not recur, whereas the fifth case was lost to follow-up. Permanent nail dystrophy after tumour removal was observed only in 1 out of the 5 cases.
In conclusion, even if dermoscopic findings do not correspond to known JXG presentations, if a nail deformity with a yellow discolouration of the nail plate is observed in a young child, subungual JXG should be considered as a differential diagnosis, and a surgical approach would provide not only an accurate diagnosis but also a correction of the nail deformity.
ACKNOWLEDGEMENTS
The patient’s parents provided written consent for the use of the patient’s photographs and medical records.
The authors have no conflicts of interest to declare.
REFERENCES
- Palmer A, Bowling J. Dermoscopic appearance of juvenile xanthogranuloma. Dermatology 2007; 215: 256–259.
- Oza VS, Stringer T, Campbell C, Hinds B, Chamlin SL, Frieden IJ, et al. Congenital-type juvenile xanthogranuloma: A case series and literature review. Pediatr Dermatol 2018; 35: 582–587.
- Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, et al. Fitzpatrick’s dermatology. 9th edn. New York: McGraw-Hill Education; 2019, p. 2032–2034.
- Haroche J, Abla O. Uncommon histiocytic disorders: Rosai-Dorfman, juvenile xanthogranuloma, and Erdheim-Chester disease. Hematology Am Soc Hematol Educ Program 2015; 2015: 571–578.
- Frumkin A, Roytman M, Johnson SF. Juvenile xanthogranuloma underneath a toenail. Cutis 1987; 40: 244–245.
- Chang P, Baran R, Villanueva C, Samayoa M, Perrin C. Juvenile xanthogranuloma beneath a fingernail. Cutis 1996; 58: 173–174.
- Piraccini BM, Fanti PA, Iorizzo M, Tosti A. Juvenile xanthogranuloma of the proximal nail fold. Pediatr Dermatol 2003; 20: 307–308.
- Kim EJ, Kim MY, Kim HO, Park YM. Juvenile xanthogranuloma of the finger: an unusual localization. J Dermatol 2007; 34: 590–592.
- Kim JK, Kim B, Won CH, Chang SE, Lee MW, Choi JH, et al. Subungual juvenile xanthogranuloma. Korean J Dermatol 2012; 50: 354–357.
- Park CS, Lee DY, Lee JH, Lim YK, Park JH, Lee JH et al. A case of unusual juvenile xanthogranuloma on the subungual area. Ann Dermatol 2019; 31: 235–237.