Paediatric psoriasis has been associated with school absenteeism, limitation of physical activities, psychiatric disorders and, in the longer term, with sexual dysfunction and addictions. This raises the hypothesis that childhood onset psoriasis may affect patients’ educational development, and further social and professional outcomes. This study evaluated the relationship between childhood onset psoriasis and patients’ educational and socioeconomic characteristics, and the development of addictions in adulthood. This cross-sectional ancillary study captured patients’ characteristics at baseline in the French PSOBIOTEQ registry. Data in adulthood included: educational (baccalaureate) and socioeconomic (working activity) groups, smoking status (self-reporting of being a current smoker vs past smoker or non-smoker), alcohol consumption (defined as at least 1 glass of alcoholic beverage per day), and living conditions (alone/family/social institutions; child at home). A total of 1,960 patients were included, of whom 26.2% had childhood onset psoriasis. In multivariate analyses, childhood onset psoriasis was associated with smoker status (p = 0.02). No association was observed with educational level, working activity, living conditions, or alcohol consumption. This study provides reassuring data overall with regard to the impact of childhood onset psoriasis on major social outcomes. Evidence for some association with addictive behaviours paves the way for larger prospective studies assessing in depth the social and educational impact of this disease.
Key words: psoriasis; children; adolescent; socioeconomic data; educational level; alcohol; tobacco.
Accepted May 4, 2022; Epub ahead of print May 4, 2022
Acta Derm Venereol 2022; 102: adv00733.
DOI: 10.2340/actadv.v102.2484
Corr: Emmanuel Mahé, Dermatology Department, Hôpital Victor Dupouy, 69 rue du Lieutenant-Colonel Prud’hon, FR-95100 Argenteuil, France. E-mail: emmanuel.mahe@ch-argenteuil.fr
SIGNIFICANCE
This study evaluated the relationship between childhood onset psoriasis and patients’ educative and socioeconomic characteristics, and the development of addictions in adulthood in 1,960 patients included in the PSOBIOTEQ registry. In multivariate analyses, childhood onset psoriasis was associated with smoker status. No association was observed with educational level, working activity, living condition, or alcohol consumption. This study provides reassuring data overall with regard to the impact of childhood onset psoriasis on major social outcomes. Evidence for some association with addictive behaviours paves the way for larger prospective studies assessing in depth the social and educational impact of this disease.
INTRODUCTION
Psoriasis affects 0.5–2% of European children, and in roughly one-third of cases of plaque psoriasis the disease starts during childhood (1–3). Recent data suggest that paediatric onset of psoriasis does not influence the prevalence of cardiovascular and metabolic comorbidities, nor of psoriatic arthritis, and does not seem to influence disease severity in adulthood (4–6). On the other hand, nail psoriasis in childhood has been suspected to be a clinical predictor for more severe disease course over time in paediatric psoriasis, and is associated with a higher prevalence of psoriatic arthritis (7, 8).
In addition to its physical impact, psoriasis in childhood affects quality of life, and has been associated in childhood with cognitive impairment, limitations in sports activities, and psychiatric symptoms, such as attention deficit disorder or attention deficit hyperactivity disorder, and later on the occurrence of sexual dysfunctions and the development of addictions (excessive tobacco and/or alcohol consumption, drug abuse) (8–14). This set of data raise the hypothesis that early psoriasis onset may affect young patients’ educational development, and later social and professional outcomes. The aim of this study was therefore to investigate the relationship between childhood onset of psoriasis and patients’ major educational and socioeconomic outcomes, as well as the development of addictive behaviours in adulthood.
METHODS
PSOBIOTEQ is the French prospective, observational, multicentre registry of adults with moderate-to-severe psoriasis receiving systemic treatments including methotrexate, cyclosporine, and biologics (15, 16). All included patients receive systemic treatment, defining a severely affected population, which is likely to show a higher disease impact on quality of life, and on psychosocial outcomes.
The current cross-sectional ancillary study captured patients’ characteristics at baseline including psoriasis subtype and severity, current psoriatic treatments, and comorbidities (psoriasis arthritis, obesity, and chronic inflammatory bowel disease) (7). Self-reported data in adulthood included: educational (baccalaureate) and socioeconomic (working activity) groups, smoking status (self-reporting of being a current smoker vs past smoker or non-smoker), alcohol consumption (defined as at least 1 glass of alcoholic beverage per day), and living conditions (alone/family/social institutions; child at home).
Definitions
Childhood onset psoriasis (COP) was defined as disease onset before the age of 18 years, and adult onset psoriasis (AOP) as disease onset after the age of 18 years.
The “lower socioeconomic” group includes, notably, labourers and farmworkers, the “upper socioeconomic” considers populations such as skilled workers, teachers, nurses, heads of companies, (17), while the “Others” group includes homemakers, both male and female, and people with no professional activity (i.e. retired persons, students, and unemployed persons). Life in social institutions includes retirement homes, homes for people in social difficulty.
Body mass index (BMI) at inclusion was derived from the patients’ body weight (in kg) divided by the height (in kg/m–2). Overweight was defined as a BMI ≥ 25.0 kg/m–2, and obesity as a BMI ≥ 30.0 kg/m–2.
Statistical analysis
Factors associated with age at onset (i.e. COP or AOP) were identified by univariate analyses (Student’s t-test for quantitative variables and χ2 or Fisher’s exact test for categorical variables, as appropriate). Univariate and multivariate analyses were performed (with logistic regression with forward selection of factors with a p-value below 0.2 in univariate analysis) to explain different outcomes of interest (educational level, working activity, living condition, being a current smoker, or alcohol consumption). All tests were 2-tailed and p-values < 0.05 were considered statistically significant.
RESULTS
From July 2012 to June 2016, 2,176 patients were included in the PSOBIOTEQ registry. For 216 patients, age at onset of psoriasis was missing and ultimately 1,960 patients were included, 513 (26.2%) with COP and 1,447 (73.8%) with AOP (Fig. 1). The mean age at inclusion was 47.8 years, and 40.8% of cases were female. The mean age at psoriasis onset was 11.4 years in COP and 36.6 in AOP. Plaque psoriasis was the predominant clinical type (86.6%), and psoriatic arthritis was identified in 9.5% of patients (Table I).

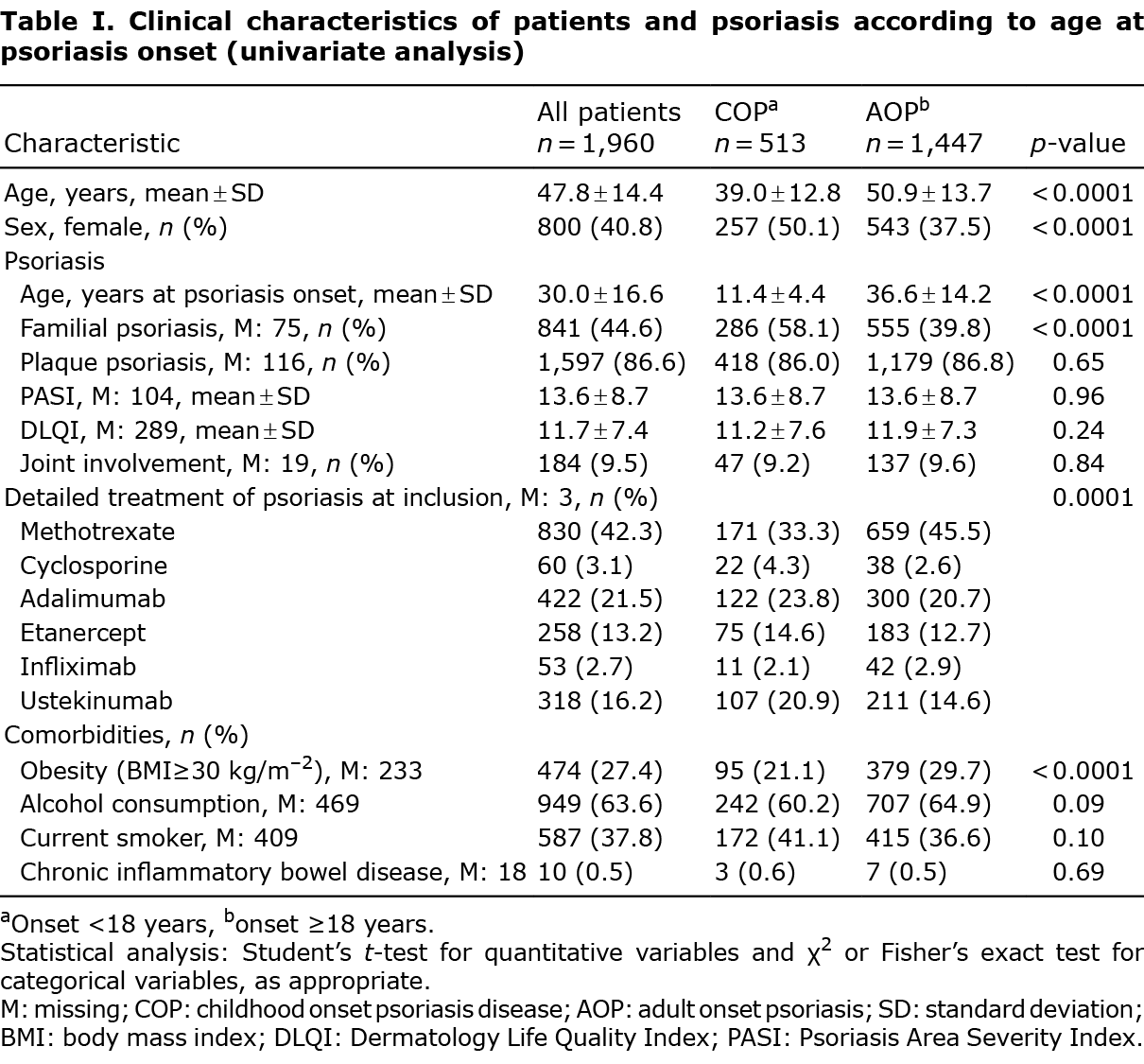
In univariate analysis, in comparison with AOP patients, those with COP were significantly younger (p < 0.0001), more frequently female (p < 0.0001), had a history of familial psoriasis (p < 0.0001), and were less likely to be obese (p < 0.0001). Methotrexate was started more frequently in AOP group, and ustekinumab in the COP group (p < 0.0001) (Table I).
In univariate analysis COP was associated with a higher educational level (p = 0.001), and with a higher representation of lower socioeconomic group (p = 0.0002). Age at psoriasis onset had no impact on living conditions (Table II).

In multivariate analyses, COP was associated with smoker status (OR [95% CI]: 1.56 [1.17-2.07]; p = 0.02), while no significant association was observed with educational level, nor with working activity, living condition or alcohol consumption (Table III).

DISCUSSION
This large-scale, real-life study did not detect any statistically significant association of an onset of psoriasis in childhood with outcomes in adulthood, such as educational level, living conditions, alcohol consumption, or working activity. On the other hand, COP was associated with a smoking status in adulthood, in contrast to data from a previously reported study (6).
A limitation of this study is the absence of quantitation of cumulative exposure and actual consumption of addictive substances, emphasizing the need for further studies capturing these important items with more granularity. Investigating this link is especially important considering the increased prevalence of cardiometabolic comorbidities, including atherosclerotic diseases, in mainly severe psoriasis in adulthood. Furthermore, such correlation calls for further investigations in young psoriasis patients and early stress, body image alteration in adolescence, all factors that have been related to increased risk of addictive behaviours in other settings (18). Some parameters are missing to establish the lack of impact of COP on socioeconomic and educational dimensions, and it remains plausible that characteristics of patients in childhood, such as psoriasis severity, treatments used and patients’ clinical responses, the parents’ social, cultural and educational level, and consultations of other specialists, such as psychiatrists, might increase self-confidence, quality of life, and therefore reduce depression, as well as student absenteeism. Moreover, we restricted the study to patients with moderate-to-severe psoriasis, since, in the PSOBIOTEQ registry, only adults on systemic treatment were included.
Results from the univariate analysis must be considered with caution, especially the observation that adults with COP show a higher educational level, but also a higher representation of people of lower working class. French educational strategies since the beginning of the 1980s, aiming for a 100% rate of high school diploma graduates at the population level, may partly account for this apparent paradox, by increasing the educational level in younger people. However, multivariate analysis corrects this paradox.
It remains plausible among patients in childhood, characteristics such as psoriasis severity, treatments used and patients’ clinical responses, the parents’ social and educational level, and consultations with other specialists, such as psychiatrists, might increase self-confidence, quality of life, and therefore reduce depression, as well as student absenteeism.
It is notable that health insurance coverage and access to treatments remain universal in France, theoretically favouring optimal management of patients with psoriasis. Indeed, more than 95% of the French population is covered by public health insurance, and severe psoriatic disease may even sometimes justify full reimbursement of patients’ care by public health insurance. Based on these demographic features, one hypothesis is that patients having access to tertiary care centres, which are mainly involved in the PSOBIOTEQ registry, are more optimally managed at an early stage of their disease, resulting in a reduced impact of psoriasis. An alternative hypothesis is that higher levels of disease severity in childhood or adolescence, which were not specifically measured in this study, may define a more impacted population that could not be identified due to limitations inherent in a real-life registry. In line with this latter hypothesis, we recently showed the reluctance of French dermatologists to use systemic and biologic treatments in children with psoriasis (19), suggesting the existence of suboptimal management of patients with COP despite reimbursement of the drugs.
Despite the limitations discussed above, this study delivers overall reassuring data with regard to the impact of early onset psoriasis on global social, familial, and professional outcomes. It also provides a rationale for larger prospective studies to provide greater in-depth assessments of the respective impacts of better-defined gradients of disease severity on educative, cognitive and socio-professional and psychological outcomes.
ACKNOWLEDGEMENTS
The PSOBIOTEQ registry is supported by unrestricted research grants from the French Ministry of Health (PHRC AOM 09 195), the French Drugs Agency (ANSM), AbbVie, Janssen, Pfizer, and MSD France. The sponsor is the Département à la Recherche Clinique et au Développement (DRCD), Assistance Publique–Hôpitaux de Paris. The PSOBIOTEQ Registry is under the aegis of the French Society of Dermatology (Société Française de Dermatologie) and its Groupe de Recherche sur le Psoriasis. None of the private funders has had any role in the design of this ancillary study, in its data management, in the analysis or interpretation of the data, in the preparation or approval of this manuscript, or in the decision to submit this manuscript for publication. They received the manuscript for information before submission.
Conflicts of interest: EM has undertaken paid activities as consultant, advisor, or speaker for AbbVie, Janssen, Celgene, Leo Pharma, Lilly, Amgen, and Novartis; FT is head of the Clinical Research Unit of La Pitié-Sélpêtrière hospital and of the Centre de Pharmacoépidémiologie (Cephepi) of the Assistance Publique – Hôpitaux de Paris – the latter having received research funding, grants and fees for consultant activities from a large number of pharmaceutical companies, and made non-discrimatory contributions of the salaries of its employees, but has received no personal remuneration; DJ has undertaken paid activities as consultant, advisor, or speaker for AbbVie, Celgen, Novartis, Lilly, Janssen, Pfizer, and Merck Sharpe & Dohme; CP for AbbVie, Amgen, Boehringer Ingelheim, Celgene, GSK, Janssen, Leo Pharma, Lilly, Novartis, and Pfizer; MM-B for AbbVie, Amgen, Celgene, Janssen, Leo Pharma, Lilly, MSD, Novartis, and Pfizer; MV for MSD, Pfizer, AbbVie, Janssen, Lilly, Leo Pharma, and Novartis; M-ARfor Pfizer, Leo Pharma, Janssen, Galderma, AbbVie, Novartis, Pierre Fabre, Merck, and BMS; N. Beneton for Pfizer and Janssen; PJ for Roche, GSK, Lilly, Principabio, Sanofi Aventis; OCfor Boehringer-Ingelheim, AbbVie, and Novartis; HB for AbbVie, Almirall, Biocad, Boehringer-Ingelheim, Janssen, Kyowa-Kirin, Leo Pharma, Novartis, UCB, and grant support from Boehringer-Ingelheim, Janssen, Leo Pharma, Novartis, Pfizer. The other authors have no conflicts of interest to declare.
REFERENCES
- Gelfand JM, Weinstein R, Porter SB, Neimann AL, Berlin JA, Margolis DJ. Prevalence and treatment of psoriasis in the United Kingdom: a population-based study. Arch Dermatol 2005; 141: 1537-1541.
- Augustin M, Glaeske G, Radtke MA, Christophers E, Reich K, Schäfer I. Epidemiology and comorbidity of psoriasis in children. Br J Dermatol 2010; 162: 633-636.
- Mahé E. Childhood psoriasis. Eur J Dermatol 2016; 26: 537-548.
- Ferrándiz C, Pujol RM, García-Patos V, Bordas X, Smandía JA. Psoriasis of early and late onset: a clinical and epidemiologic study from Spain. J Am Acad Dermatol 2002; 46: 867-873.
- De Jager ME, de Jong EM, Meeuwis KA, van de Kerkhof PC, Seyger MM. No evidence found that childhood onset of psoriasis influences disease severity, future body mass index or type of treatments used. J Eur Acad Dermatol Venereol 2010; 24: 1333-1339.
- Mahé E, Maccari F, Beauchet A, Lahfa M, Barthelemy H, Reguiaï Z, et al. Childhood-onset psoriasis: association with future cardiovascular and metabolic comorbidities. Br J Dermatol 2013; 169: 889-895.
- Bronckers IMGJ, Bruins FM, van Geel MJ, Groenewoud HMM, Kievit W, van de Kerkhof PCM, et al. Nail involvement as a predictor of disease severity in paediatric psoriasis: follow-up data from the Dutch ChildCAPTURE registry. Acta Derm Venereol 2019; 99: 152–157.
- Pourchot D, Bodemer C, Phan A, Bursztejn AC, Hadj-Rabia S, Boralevi F, et al. Nail psoriasis: a systematic evaluation in 313 children with psoriasis. Pediatr Dermatol 2017; 34: 58-63.
- Randa H, Todberg T, Skov L, Larsen LS, Zachariae R. Health-related quality of life in children and adolescents with psoriasis: a systematic review and meta-analysis. Acta Derm Venereol 2017; 97: 555-563.
- Ramsay B, O’Reagan M. A survey of the social and psychological effects of psoriasis. Br J Dermatol 1988; 118: 195–201.
- Bilgic A, Bilgic Ö, Akış HK, Eskioğlu F, Kılıç EZ. Psychiatric symptoms and health-related quality of life in children and adolescents with psoriasis. Pediatr Dermatol 2010; 27: 614–617.
- Carter-Pokras OD, Bugbee BA, Lauver PE, Aiken R, Arria AM. Utilizing student health and academic data: a county-level demonstration project. Health Promot Pract 2021; 22: 193–203.
- Zink A, Herrmann M, Fischer T, Lauffer F, Garzorz-Stark N, Böhner A, et al. Addiction: an underestimated problem in psoriasis health care. J Eur Acad Dermatol Venereol 2017; 31: 1308–1315.
- Caroppo F, Zacchino M, Milazzo E, Fontana E, Nobile F, Marogna C, et al. Quality of life in children with psoriasis: results from a monocentric study. Ital J Dermatol Venerol 2021; 156: 374–377.
- Sbidian E, Giboin C, Bachelez H, Paul C, Beylot-Barry M, Dupuy A, et al. Factors associated with the choice of the first biologic in a psoriasis: real life analysis from the Psobioteq cohort. J Eur Acad Dermatol Venereol 2017; 31: 2046–2054.
- Masson Regnault M, Castañeda-Sanabria J, Diep Tran MHT, Beylot-Barry M, Bachelez H, Beneton N, et al. Users of biologics in clinical practice: would they be eligible for phase III clinical studies? Cohort Study in the French Psoriasis Registry PSOBIOTEQ. J Eur Acad Dermatol Venereol 2020; 34: 293–300.
- Beck F, Guilbert P, Gautier A, editors. Baromètre Santé 2005. Edition INPES, Saint-Denis, France; 2007.
- Ewald DR, Strack RW, Orsini MM. Rethinking addiction. Glob Pediatr Health 2019 23; 6: 2333794X18821943.
- Mahé E, Bursztejn AC, Phan A, Corgibet F, Beauchet A. Management of childhood psoriasis in France. A national survey among general practitioners, pediatricians, and dermatologists. Dermatol Ther 2018; 31: e12567.