Symmetrical White Transparent Papules: A Quiz
Zhen-Ting Lin, Jiang-Wei Cheng, Hao Guo* and Jiu-Hong Li*
Department of Dermatology, The First Hospital of China Medical University, 155N Nanjing Street, Shenyang 110001, PR China. *E-mail: guohao27@126.com, pfkl2011@126.com
A 42-year-old man presented to our department with oedema and thickening of his hands. Lesions were present, occurring as multiple pinhead-sized white symmetrical, transparent papules on the wrists, palms, and dorsum of his hands (Fig. 1) within 3 min of immersion into water, accompanied by burning sensations. The papules resolved within 30–60 min after drying, and may have developed due to frequent handwashing during the COVID-19 pandemic. The patient was treated with topical hydrocortisone ointment for 2 months after previously being diagnosed with chronic eczema, which was largely ineffective. Routine laboratory test results, including serology for syphilis and HIV antibodies, were negative or within normal limits. At the same time, the man reported a 10-year history of hyperhidrosis and denied any history of cystic fibrosis (CF), family histories of significant skin disorders, or using of non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin or celecoxib. A biopsy was taken from his left palm.

What is your diagnosis? See next page for answer.
Symmetrical White Transparent Papules: A Commentary
Acta Derm Venereol 2022; 102: adv00720.
DOI: 10.2340/actadv.v102.2488
Diagnosis: Aquagenic syringeal acrokeratoderma
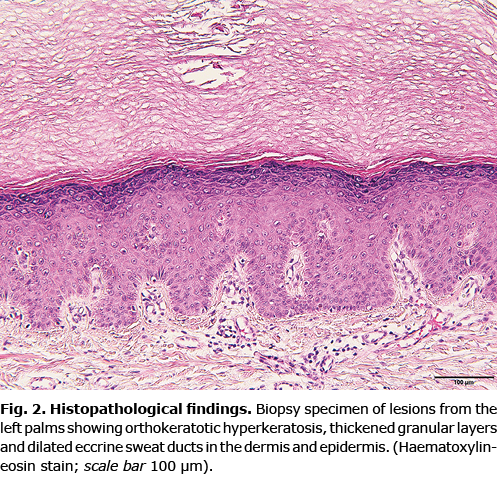
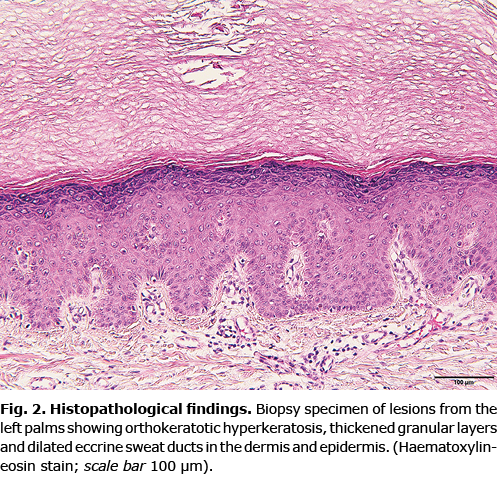
A skin biopsy specimen from the left palm revealed orthokeratotic hyperkeratosis, thickened granular layers, and dilated eccrine sweat ducts in the dermis and epidermis, meanwhile, dilated sweat duct ostia (acrosyringium) passing through the stratum corneum (Fig. 2). Histopathological examination was consistent with a diagnosis of aquagenic syringeal acrokeratoderma (ASA).
Based on the clinical manifestations, contact history, and non-specific pathological examination, a diagnosis of ASA was formulated. The patient was treated with topical hydrocortisone urea ointment and immersing both hands into formalin. In the meantime, washing the hands was not recommended unless necessary. The patient was treated with botulinum toxin injection for hyperhidrosis. After 2 months, the symptoms were obviously improved.
ASA is a rare and transient acquired palmoplantar keratoderma, characterized by white symmetrical, transparent, papules. It mostly affected the palms and occasionally the soles, and is seen predominantly in adolescence and women. ASA demonstrates “hand in the bucket sign” after a brief immersion in water (1). In the current case, the patient was a middle-aged man, and the sites involved were the dorsal hands and palms, which is a rare clinical presentation. This case is the first report of this disease in a middle-aged man in both dorsal hands according to previous literature (1–5).
The diagnosis of ASA relies mainly on the clinical manifestation and contact history, and ASA is usually considered to be primarily a clinical entity. The histopathological changes in ASA are not specific. The most recognizable features of histopathological changes that have been reported are orthohyperkeratosis with increased thickness and dilated dermal eccrine ducts (3).
The pathophysiology of ASA remains unclear, and increased sodium retention in epidermal cells contributing to increased water uptake capacity is a commonly described mechanism (6). Other theories include a decrease in stratum corneum barrier function, increased skin aquaporin expression, and increased sympathetic activity and the involvement of eccrine sweat glands, which are innervated by the sympathetic nervous system (6, 7). Similar manifestations have been observed in patients taking COX-2 inhibitors (6). It has been reported that 40–84% of patients with cystic fibrosis (CF) also developed ASA (7). We consider that, in the current patient, frequent hand washing during the COVID-19 pandemic was the main underlying cause.
The differential diagnosis includes chronic eczema, progressive symmetrical erythrokeratodermia (PSEK), and hereditary papulotranslucent acrokeratoderma (HPA) (8). Initially, ASA may easily be misdiagnosed as eczema, and when skin manifestations are found to be aggravated by immersion into water, we should reconsider the diagnosis. PSEK is characterized by stable, well-defined, erythematous, hyperkeratotic plaques, mainly affecting the knees, elbows, buttocks, head and dorsal surfaces of the hands and feet (9); HPA is characterized by yellowish-white, translucent, papules or plaques, mainly on palms and occasionally on soles, and it occurred shortly after puberty. To our knowledge, this disorder is inherited through an autosomal-dominant pattern (10).
During the COVID-19 pandemic, many people’s hygiene habits have changed. As a result of frequent handwashing and hand disinfection the frequency of ASA has greatly increased. Occurrence on the both dorsal hands of middle-aged men is still rare, and dermatologists should pay particular attention to diagnosis of this disorder.
ACKNOWLEDGEMENTS
The authors thank the patient for permission to use his photographs and clinical data.
The authors have no conflicts of interest to declare.
REFERENCES
- Angra D, Angra K, Rodney IJ. Aquagenic palmoplantar keratoderma with dorsal hand involvement in an adolescent female. JAAD Case Rep 2016; 2: 239–240.
- Luo DQ. Aquagenic acrokeratoderma: a case with family history and unusual involvements of the palms and soles, and the dorsum of fingers and toes. J Dermatol 2011; 38: 612–615.
- Rongioletti F, Tomasini C, Crovato F, Marchesi L. Aquagenic (pseudo) keratoderma: a clinical series with new pathological insights. Br J Dermatol 2012; 167: 575–582.
- Xia Q. Aquagenic acrokeratoderma: case report with no involvement of the palms. Int J Dermatol 2012; 51: 1391–1393.
- Yoon TY, Kim KR, Lee JY, Kim MK. Aquagenic syringeal acrokeratoderma: unusual prominence on the dorsal aspect of fingers? Br J Dermatol 2008; 159: 486–488.
- Darlenski R, Tsankov N. Aquagenic syringeal acrokeratoderma. J Dtsch Dermatol Ges 2012; 10: 198.
- Medhus EJ, DeVore AC, DeVore K. Aquagenic palmoplantar keratoderma therapeutic response to topical glycopyrronium. JAAD Case Rep 2021; 13: 17–19.
- Luo DQ, Li Y, Huang YB, Wu LC, He DY. Aquagenic syringeal acrokeratoderma in an adult man: case report and review of the literature. Clin Exp Dermatol 2009; 34: e907–909.
- Gray LC, Davis LS, Guill MA. Progressive symmetric erythrokeratodermia. J Am Acad Dermatol 1996; 34: 858–859.
- Sun Y, Jia H. Hereditary papulotranslucent acrokeratoderma: a simultaneous presentation in daughter and mother. Indian J Dermatol Venereol Leprol 2013; 79: 555.