Poikilodermatous and Ichthyosiform Patches all over the Body and Dark-brown Nodules on the Legs: A Quiz
Fengjie Liu, Xiqing Li, Jian-chi Ma, Liangchun Wang and Zhenrui Shi*
Department of Dermatology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, 107 Yanjiang Road W, Guangzhou 510120, China. *E-mail: zrshi1989@outlook.com
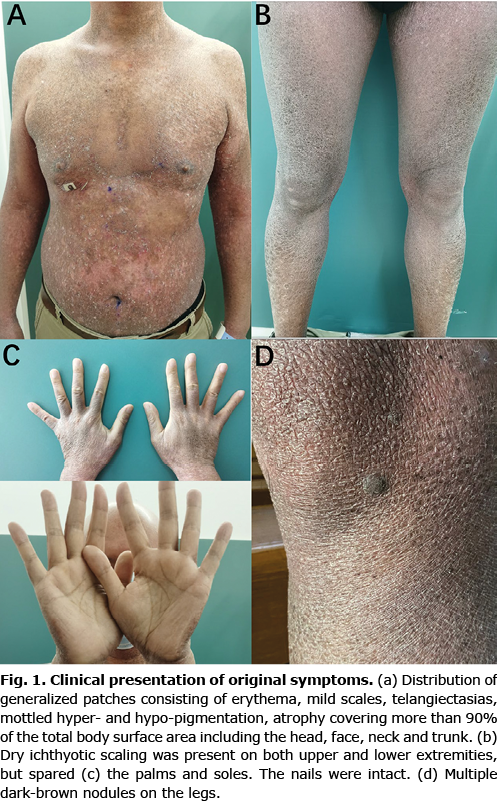
A Chinese man in his 40s was referred to our clinic with asymptomatic, erythematous patches all over his body and ichthyotic scaling on his extremities. The initial lesions had started approximately 36 years previously and presented as hypopigmented patches, mainly involving the neck, trunk, and flexor side of the arm. He had undergone topical corticosteroid and multiple traditional Chinese medicine treatments for several years without improvement. The skin lesions gradually spread all over his body and transformed into poikilodermatous patches with hair loss and ichthyotic scaling on the extremities 14 years previously. Multiple dark-brown nodules were observed on his legs 1 year previously. Physical examination revealed generalized patches consisting of erythema, mild scaling, telangiectasias, mottled hyper-, and hypo-pigmentation, and atrophy distributed among the trunk and extremities, covering more than 90% of the body surface. Dry ichthyotic scaling was observed on both upper and lower extremities, but spared his palms and soles. Twelve rice- to pea-sized, brownish-to-dark, firm nodules were found on his legs (Fig. 1). The head and axilla hair, eyebrow and lanugo hair was absent. Cervical, axillary and inguinal lymphadenopathy was noted.
What is your diagnosis? See next page for answer.
Poikilodermatous and Ichthyosiform Patches all over the Body and Dark-brown Nodules on the Legs: A Commentary
Acta Derm Venereol 2022; 102: adv00759.
DOI: 10.2340/actadv.v102.2504
Diagnosis: Poikilodermatous and ichthyosiform CD8+ mycosis fungoides with multiple eruptive dermatofibromas
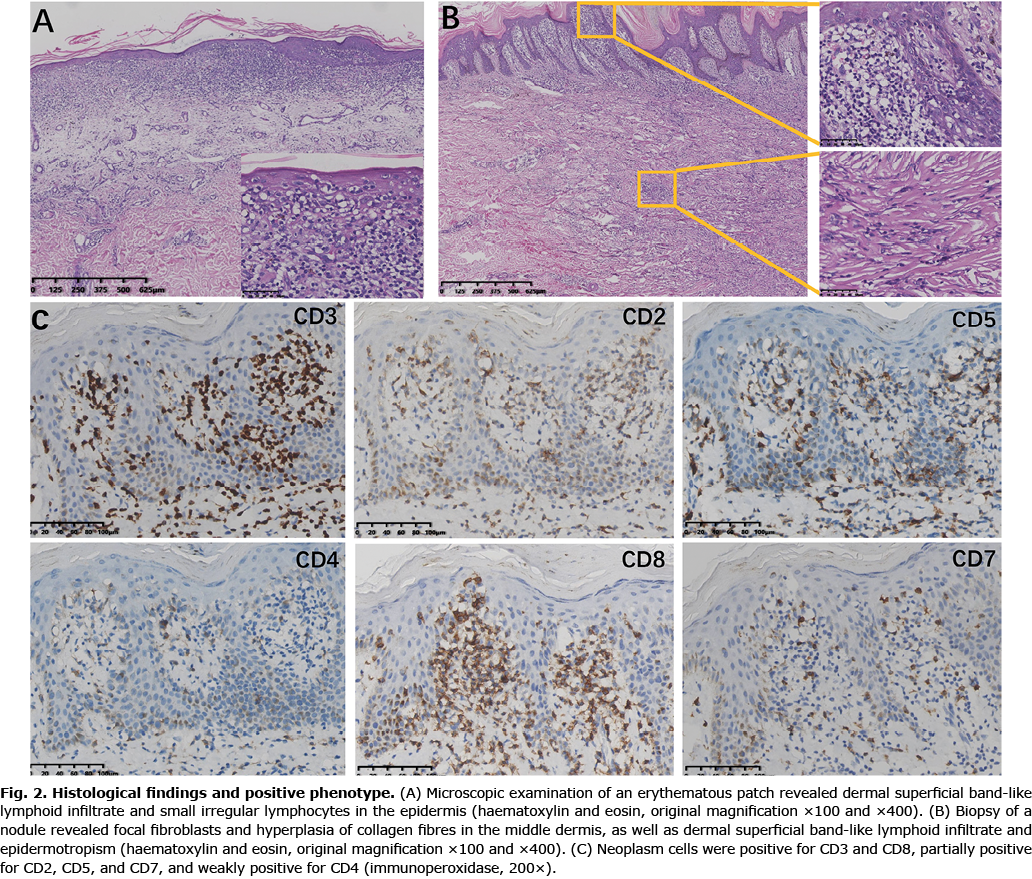
Histopathological findings of erythematous patches revealed superficial band-like lymphoid infiltration, epidermotropism with Pautrier’s microabscess and lymphoid atypia (Fig. 2A), consistent with mycosis fungoides (MF). Biopsy of a nodule showed histopathological changes in dermatofibromas (DF) including focal fibroblasts, hyperplasia of collagen fibres in the dermis and acanthotic epidermis with basal hyperpigmentation. Epidermotropism was also found in epidermis of the nodule (Fig. 2B). Immunohistochemical staining of the nodule (Fig. 2C) and erythematous patches (data not shown) showed that the atypical cells were positive for CD3 and CD8, partially positive for CD2/5/7, and weakly positive for CD4. Gene rearrangement of T-cell receptor (TCR) was positive for TCRB and TCRG. Less than 5% atypical cells were present in the circulation assessed by flow cytometry. A punch biopsy of axillary lymph node revealed dermatopathic lymphadenitis. There was no evidence of solid-organ involvement based on a computed tomography (CT) scan of the chest, abdomen and pelvis. Thus, a diagnosis of CD8+ MF of IIIA (T4N1M0B0) stage was made (1). He was treated with narrow-band ultraviolet-B phototherapy, interferon alpha-2b and methotrexate. The lesions of DF were removed by surgical excision for aesthetic reasons.
MF classically presents with the stepwise appearance of patches, plaques and tumours on non-sun exposed skin. Poikilodermatous and ichthyosiform MF are 2 rare variants of MF (2). This case showed both skin manifestations of poikilodermatous and ichthyosiform lesions, which, to the best of our knowledge, has not been reported previously. Unlike classical MF, the immunohistochemical pattern of poikilodermatous MF is predominantly positive for CD8 rather than CD4, usually indicating a mild biological behaviour (3). Another distinct clinical form of MF with CD8+ phenotype is hypopigmented MF. This patient initially presented with hypopigmented patches in childhood, consistent with the clinical characteristics of hypopigmented MF (4). The patient had undergone biopsy 13 years previously, and histological examination revealed signs of superficial lymphoid infiltrate and epidermotropism (data not shown). However, the diagnosis of MF was not made at that time due to the absence of cellular atypia. This case has now evolved into stage IIIA, an advanced-stage of MF at the time of final diagnosis. The prognosis was poor and effective management should be offered to the patient. This case highlights the importance of early diagnosis of MF based on combined clinical, histopathological, molecular biological and immunopathological criteria.
DF is a common, benign, dermal tumour, often occurring as a single lesion. Multiple eruptive DFs (MEDFs) are defined as more than 5 DFs appearing within 4 months (5) and usually associated with autoimmune diseases, immunosuppressant therapy, HIV infection, haematological malignancy, pregnancy and other conditions (6). The current patient had a total of 12 DFs, half of which newly developed within 6 months, compatible with the number and eruptive nature of MEDFs. So far only 1 case with MEDF was reported in a patient with MF (7). Notably, that patient had a history of immunosuppressive treatment with systemic corticosteroids. The current patient had not received any immunosuppressants or topical treatments during the last 5 years before developing MEDFs, suggesting that the progression of MF might play a major role in inducing the developments of MEDFs.
REFERENCES
- Olsen E, Vonderheid E, Pimpinelli N, Willemze R, Kim Y, Knobler R, et al. Revisions to the staging and classification of mycosis fungoides and Sezary syndrome: a proposal of the International Society for Cutaneous Lymphomas (ISCL) and the cutaneous lymphoma task force of the European Organization of Research and Treatment of Cancer (EORTC). Blood 2007; 110: 1713–1722.
- Virmani P, Myskowski PL, Pulitzer M. Unusual variants of mycosis fungoides. Diagn Histopathol (Oxf) 2016; 22: 142–151.
- Nikolaou VA, Papadavid E, Katsambas A, Stratigos AJ, Marinos L, Anagnostou D, et al. Clinical characteristics and course of CD8+ cytotoxic variant of mycosis fungoides: a case series of seven patients. Br J Dermatol 2009; 161: 826–830.
- Castano E, Glick S, Wolgast L, Naeem R, Sunkara J, Elston D, et al. Hypopigmented mycosis fungoides in childhood and adolescence: a long-term retrospective study. J Cutan Pathol 2013; 40: 924–934.
- Ammirati CT, Mann C, Hornstra IK. Multiple eruptive dermatofibromas in three men with HIV infection. Dermatology 1997; 195: 344–348.
- Huang PY, Chu CY, Hsiao CH. Multiple eruptive dermatofibromas in a patient with dermatomyositis taking prednisolone and methotrexate. J Am Acad Dermatol 2007; 57: S81–84.
- Gualandri L, Betti R, Cerri A, Pazzini C, Crosti C. Eruptive dermatofibromas and immunosuppression. Eur J Dermatol 1999; 9: 45–47.