SHORT COMMUNICATION
Similar Levels of Disease Severity Correspond to a Greater Burden of Illness in Women Compared with Men with Hidradenitis Suppurativa
Tonia SAMELA1,2, Anna DATTOLO1, Giorgia CORDELLA2, Valeria ANTINONE2, Simona MASTROENI1, Roberta FUSARI1, Luca FANIA3 and Damiano ABENI1
1Clinical Epidemiology Unit, 2Clinical Psychology Unit, and 3Dermatology Unit, IDI-IRCCS, Via dei Monti di Creta, 104, IT-00167 Rome, Italy. E-mail: t.samela@idi.it
Citation: Acta Derm Venereol 2022; 103: adv00856. DOI https://doi.org/10.2340/actadv.v103.4426.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Nov 8, 2022; Published: Jan 27, 2023
Competing interests and funding: The authors have no conflicts of interest to declare.
INTRODUCTION
Hidradenitis suppurativa (HS) has a considerable impact on quality of life (QoL), with intense pain and pruritus, high degrees of physical disability (1), and relevant psychiatric comorbidity (2). It is possible to conceptualize dermatological diseases as multifactorial conditions with 3 dimensions: “disease”, an organic phenomenon, which can be identified by objective means (3, 4); “illness”, the subjective state of patients; and “sickness”, defined by how the sociocultural context interprets health statuses (5). Sex-associated differences in HS (6, 7) have been reported, but sex-specific QoL in HS has rarely been addressed. The aim of this study was to assess whether the same clinical severity, estimated through the International HS Severity Score System (IHS4), corresponds to different illness severity in men and women. To the best of our knowledge, this is the first time that a combination of such measures is used to estimate the illness load of HS.
MATERIALS AND METHODS
This cross-sectional, observational study was approved by the Istituto Dermopatico dell’Immacolata IDI-IRCCS Ethical Commettee. Data were collected from December 2015 to the end of 2020 at IDI-IRCCS, Rome, Italy. Details of the registry (i.e. inclusion/exclusion criteria, clinical severity measures, and patient-reported outcomes (PROs)), in which consecutive patients were enrolled, have been described in detail elsewhere (8).
The IHS4 was used as a continuous score, with several PROs: Skindex-17 (9), Dermatology Life Quality Index (DLQI) (10), and 12-item General Health Questionnaire (GHQ-12) (11).
Patients who agreed to participate completed the study PRO and the sociodemographic form. A dermatologist recorded the clinical severity and features on standardized case-report forms. Categorical variables were described as number and percentage, and continuous variables were categorized and then described using absolute and relative frequencies; significances were calculated by Fisher’s test or Pearson’s χ2 test. Spearman’s ρ coefficient was used to measure sex-specific correlations between PROs.
“Illness/disease” ratios were computed, to answer the question: “how much impairment, in terms of illness, is caused by each point of the IHS4?”. PRO scores were divided by the IHS4 score (IHS4=0 was recoded as 1). This procedure was performed for both sexes, to detect differences in the impact of disease on illness. The same strategy was applied to each item of the PRO, to compute the item-specific/IHS4 ratio.
RESULTS
A total of 452 registered patients were analysed: 273 women (60.4%); 52.0% with severe HS (i.e. IHS4≥11) (Table I).
| Variable | na | % |
| Overall | 452 | 100.0 |
| Sex | ||
| Men | 179 | 39.6 |
| Women | 273 | 60.4 |
| Ageb | ||
| < 29 years | 359 | 79.6 |
| > 29 years | 92 | 20.4 |
| Education | ||
| < 9 years | 160 | 35.6 |
| 9–13 years | 215 | 47.9 |
| >14 years | 74 | 16.5 |
| Body mass index, kg/m2 | ||
| < 25 | 160 | 36.6 |
| 25–29.9 | 162 | 37.1 |
| >30 | 115 | 26.3 |
| Durationc | ||
| <10 years | 279 | 61.9 |
| >10 years | 172 | 38.1 |
| International Hidradenitis Suppurativa Severity Score System | ||
| <4 | 79 | 17.5 |
| 4–10 | 138 | 30.5 |
| >11 | 235 | 52.0 |
| aTotals may vary due to missing data. bCut-off refers to median value derived from age (in years). cYears of illness from diagnosis to recruitment to the study. | ||
Weak-to-moderate IHS4-PRO correlations were observed for both sexes. For men: GHQ-12, ρ = 0.13; Skindex-17 symptoms, ρ = 0.27, psychosocial, ρ = 0.30; DLQI, ρ = 0.34. For women: GHQ-12, ρ = 0.04; Skindex-17 symptoms, ρ = 0.31, psychosocial, ρ = 0.17; DLQI, ρ = 0.29.
The Skindex-17 symptoms/IHS4 ratio was 7.84 for men vs 12.80 for women (p < 0.001); the Skindex-17 psychosocial/IHS4 ratio was 4.96 for men vs 11.44 for women (p < 0.001). The DLQI/IHS4 ratio was also higher for women: 2.35 vs 1.14 in men (p < 0.001), as was the GHQ-12/IHS4 ratio: 3.58 for women vs 1.90 for men p < 0.001).
The item-specific/IHS4 ratio revealed that differences between men and women were statistically significant for each item, except for Skindex-17 item 9 (Fig. 1). The largest item/IHS4 ratio differences between women and men were observed in sexual difficulties, embarrassment, pain, and depression.
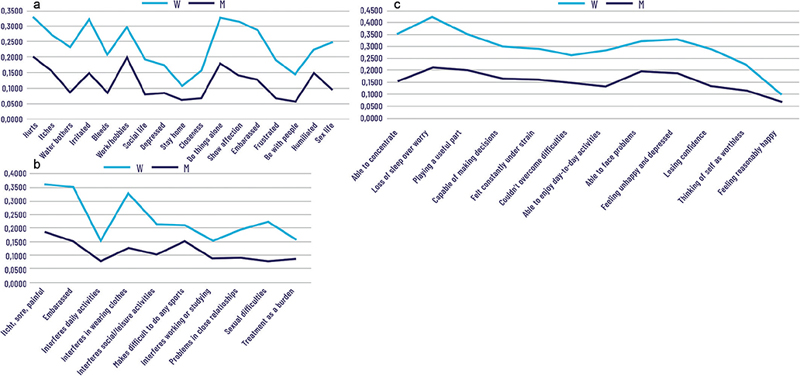
Fig. 1. Single item analysis for the (a) Skindex-17 symptoms/International HS Severity Score System (IHS4) ratio, (b) Dermatology Life Quality Index (DLQI)/IHS4 ratio, and (c) 12-item General Health Questionnaire (GHQ-12//IHS4 ratio: mean values, separately for men and women. Note: differences between men and women are all statistically significant (i.e. p < 0.050), except for (a) item “water bothers”, p = 0.068, and (b) “makes difficult to do any sport, p = 0.120. W: women; M: men.
DISCUSSION
In this study, an increase of a single point of the IHS4 corresponds to vastly different degrees of impairment in women and men in all the aspects of QoL, highlighting the fact that “objective measures” of disease severity may have substantially different meaning for men and women. More specifically, the same degree of HS severity has greater impact and consequences on the actual well-being of women compared with men.
It is possible that the same disease leads to different illness perceptions among the sexes. Several studies have highlighted the role of psychological factors in illness perception among women and men (12), and health researchers have proposed Stress Theory as an explanatory model for sex differences in health. Female’s poorer health could derive from combinations of employment and family roles. It is plausible that these sociological factors may impact patients’ sickness perception. Moreover, women are also often socialized to want to be thin and attractive (13). It is plausible that psychological factors mediate the effect of social roles and positions on patient’s illness perception (1).
The wide disparity in sex-specific disease perception is further highlighted by the single-item analysis, which revealed a strong discrepancy in illness/disease ratio scores between men and women, with women invariably showing the higher impact of illness. This pattern was consistently confirmed through all PROs and, in particular, for shame/embarrassment, introversion, isolation, and withdrawal experienced by women. For men, the greatest impact of disease concerns everyday life activities, as men seem to be more focused on operational thinking and action, and identifying their self-image in relation to their actions. Women, instead, seem to focus their self-perception on the relational and social consequences of their health problems. However, sex roles are culture-specific, hence these results should be transferred with caution to different geographical areas.
In conclusion, this study is innovative, in that it shows sex-related differences in illness and sickness of HS while accounting for clinical severity. In addition, the PROs/IHS4 measure offers manageable and directly interpretable information on the actual situation of the individual patient. It could be used in clinical practice to evaluate individual patients.
While these results should be confirmed in other cultures, it could now be hypothesized that different cut-offs for clinical severity of HS may be warranted for men and women.
ACKNOWLEDGEMENT
This work was supported in part by the “Progetto di Ricerca Corrente 2021 – RC4.3” of the Italian Ministry of Health, Rome, Italy.
REFERENCES
- Sampogna F, Fania L, Mazzanti C, Pallotta S, Panebianco A, Mastroeni S, et al. The impact of hidradenitis suppurativa on general health is higher than that of hypertension, congestive heart failure, type 2 diabetes, myocardial infarction and depression. J Eur Acad Dermatol Venereol 2020; 34: e386–e388.
- Matusiak Ł, Szczęch J, Bieniek A, Nowicka-Suszko D, Szepietowski JC. Increased interleukin (IL)-17 serum levels in patients with hidradenitis suppurativa: Implications for treatment with anti-IL-17 agents. J Am Acad Dermatol 2017; 76: 670–675.
- Engert V, Grant JA, Strauss B. Psychosocial factors in disease and treatment – a call for the biopsychosocial model. JAMA Psychiatry 2020; 77: 996–997.
- Hofmann B. On the triad disease, illness and sickness. J Med Philos 2002; 27: 651–673.
- Twaddle A. Disease, illness and sickness revisited. Disease, illness and sickness: three central concepts in the theory of health 1994; 18: 1–18.
- Bianchi L, Caposiena Caro RD, Ganzetti G, Molinelli E, Dini V, Oranges T, et al. Sex-related differences of clinical features in hidradenitis suppurativa: analysis of an Italian-based cohort. Clin Exp Dermatol 2019; 44: e177–e180.
- Yee D, Collier EK, Atluri S, Jaros J, Shi VY, Hsiao JL. Gender differences in sexual health impairment in hidradenitis suppurativa: a systematic review. Int J Womens Dermatol 2021; 7: 259–264.
- Sampogna F, Fania L, Mastroeni S, Fusari R, Napolitano M, Ciccone D, et al. Correlation between depression, quality of life and clinical severity in patients with hidradenitis suppurativa. Acta Derm Venereol 2020;100: adv00319.
- Nijsten TEC, Sampogna F, Chren MM, Abeni DD. Testing and reducing Skindex-29 using Rasch analysis: Skindex-17. J Invest Dermatol 2006; 126: 1244–1250.
- Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI) – a simple practical measure for routine clinical use. Clinical Clin Exp Dermatol 1994; 19: 210–216.
- Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997; 27: 191–197.
- Gijsbers van Wijk CMT, Huisman H, Kolk AM. Gender differences in physical symptoms and illness behavior: a health diary study. Soc Sci Med 1999; 49: 1061–1074.
- Gove WR. Sex differences in mental illness among adult men and women: an evaluation of four questions raised regarding the evidence on the higher rates of women. Soc Sci Med (1967) 1978; 12: 187–198.