Halo (Sutton) naevus is a type of benign melanocytic naevus characterized by a bright rim occurring around an existing naevus. Halo naevi usually occur as solitary lesions in children and adolescents, with a mean age of development of 15 years, often with a familial tendency (1). Halo naevi are found in approximately 1% of young adults, with no sex predilection. The 2 most common sites for their development are the trunk, followed by the scalp (2).
Optical super-high magnification dermoscopy (OSHMD) is a new, state-of-the-art dermoscopy modality, which enables up to 400× magnification of the skin, often allowing the examiner to identifiy pigmented single cells and differentiate cell types (e.g between keratinocytes and melanocytes). Due to its high resolution, OSHMD enables the imaging of lesions at unprecedented quality, which can be useful, especially when standard dermoscopy does not show essential details. To our knowledge, no OSHMD image of a halo naevus has been published to date.
CASE REPORT
A healthy Caucasian 6-year-old boy presented with an asymptomatic lesion of the scalp, which had developed a few months previously. Clinically it was a 4-mm symmetrical dark-brown macule with peripheral hypopigmentation. The patient’s personal and family history was negative for vitiligo and melanoma.
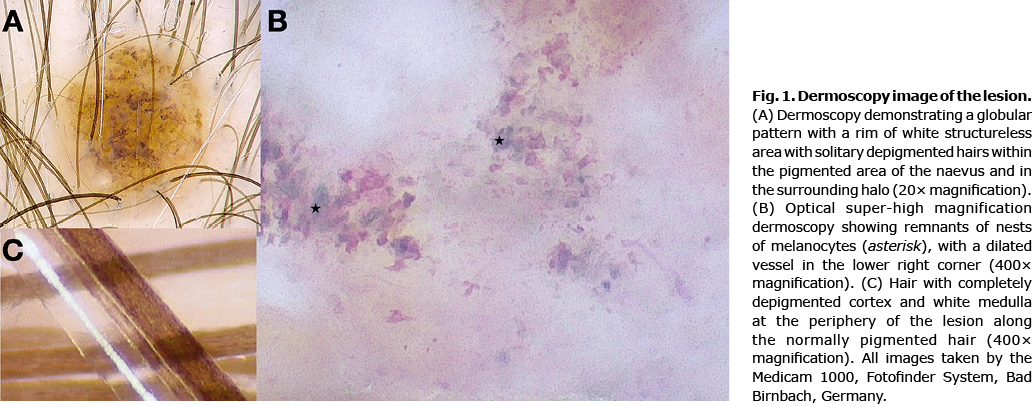
Under 20× dermoscopy (Medicam 1000, Fotofinder System, Bad Birnbach, Germany) the lesion presented a globular pattern with a rim of white structureless area with solitary depigmented hairs within the pigmented area of the naevus and in the subtly visible surrounding halo (Fig. 1A). OSHMD with 400× magnification revealed remnants of nests of melanocytes with a dilated vessel (Fig. 1B). Moreover, OSHMD revealed, with striking detail, the structure of a hair with completely depigmented cortex and white medulla at the periphery of the lesion along the normally pigmented hair (Fig. 1C). These aspects were indicative of halo naevi and were barely visible under conventional dermoscopy.
At 6-month follow-up the naevus did not show any significant changes.
DISCUSSION
The 2 most dominant dermoscopic patterns of halo naevi are globular and homogeneous, with the globular type being more prevalent in children (1). The halo phenomenon around the naevus is the result of a lymphocyte-mediated regression that can also be observed around many other benign and malignant skin lesions, including melanoma (3, 4). Although melanoma with regression usually has more irregular areas of depigmentation, and melanoma with halo-like depigmentation is extremely rare in children, its possible presence should be taken into account and detailed dermoscopy analysis could be important for the differential diagnosis.
OSHMD can help to distinguish between naevus and melanoma, due to its high resolution, and the potential to capture details not achievable in standard dermoscopy, including differentiation of the morphology and even the colours of the cells (5, 6). The current case showed depigmented hair and whitish areas around regular melanocytes, favouring the diagnosis of halo naevus.
To our knowledge, this is the first report of the dermoscopic structures of halo naevus visualized with OSHMD; however, further studies should be performed on larger series of cases in order to evaluate the diagnostic usefulness of this type of dermoscopy.
REFERENCES
- Kolm I, Di Stefani A, Hofmann-Wellenhof R, Fink-Puches R, Wolf IH, Richtig E, et al. Dermoscopy patterns of halo nevi. Arch Dermatol 2006; 142: 1627–1632
- Nedelcu R, Dobre A, Brinzea A, Hulea I, Andrei R, Zurac S, et al. Current challenges in deciphering sutton nevi – literature review and personal experience. J Pers Med 2021; 11: 904.
- Zeff RA, Freitag A, Grin CM, Grant-Kels JM. The immune response in halo nevi. J Am Acad Dermatol 1997; 37: 620–624.
- Mooney MA, Barr RJ, Buxton MG. Halo nevus or halo phenomenon? A study of 142 cases. J Cutan Pathol 1995; 22: 342–348.
- Cinotti E, Tognetti L, Campoli M, Liso F, Cicigoi A, Cartocci A, et al. Super-high magnification dermoscopy can aid the differential diagnosis between melanoma and atypical naevi. Clin Exp Dermatol 2021; 46: 1216–1222
- Dusi D, Rossi R, Simonacci M, Ferrara G. Image gallery: the new age of dermoscopy: optical super-high magnification. Br J Dermatol 2018; 178: e330.