Removal of the deep fascia is recommended in therapy for dermatofibrosarcoma protuberans, but its necessity in the context of micrographic surgery is unclear. A retrospective clinicopathological analysis of 48 patients with dermatofibrosarcoma protuberans treated by micrographic surgery was performed, to determine in which tumours fascia preservation was feasible and safe. Histologically, 93% of tumours on the trunk and extremities and 14% of tumours in the head and neck region were fully located above the fascia. Localization on the head and neck was the only significant risk factor for tumour extension beyond the subcutis (p<0.001). Overall, 44% of tumours were completely excised above the fascia and 56% with deeper excisions. Two deeply infiltrating tumours (4%) on the head recurred, but in none of these lesions was the fascia spared. These results show that micrographic surgery allows fascia preservation in superficial tumours outside the head and neck region.
Key words: dermatofibrosarcoma protuberans; fascia; histology; micrographic surgery; Mohs surgery.
Accepted Sep 2, 2021; Epub ahead of print Sep 7, 2021
Acta Derm Venereol 2021; 101: adv00561.
doi: 10.2340/00015555-3915
Corr: Maximilian Gassenmaier, Department of Dermatology, Eberhard Karls University of Tübingen, Liebermeisterstr. 25, DE-72076 Tübingen, Germany. E-mail: maximilian.gassenmaier@med.uni-tuebingen.de
SIGNIFICANCE
Dermatofibrosarcoma protuberans is a rare, locally aggressive, cutaneous, soft tissue sarcoma. Excision of the deep fascia is recommended to achieve tumour clearance, but its necessity in the context of micrographic surgery is unclear. This study investigated 48 tumours excised with micrographic surgery at a tertiary referral centre to determine whether and for which tumours the preservation of the fascia is feasible and safe. The results showed that most dermatofibrosarcoma protuberans were completely epifascial in location, and that the infiltration depth depended on the tumour site. Fascia preservation in superficial dermatofibrosarcoma protuberans was not associated with an increased risk of recurrence.
INTRODUCTION
Dermatofibrosarcoma protuberans (DFSP) is an uncommon cutaneous sarcoma and represents a slow-growing, locally aggressive, soft tissue tumour with low metastatic potential. DFSP most commonly affects the trunk and proximal extremities and occurs in all age groups, with a peak age incidence between 25 and 45 years (1).
Clinically, DFSP begins as an asymptomatic skin-coloured plaque that evolves slowly into a nodular or multinodular tumour over months to years (2). Due to the asymmetrical growth behaviour and eccentric projections, tumour boundaries cannot be reliably identified preoperatively. Tentacle-like proliferations of bland tumour cells further complicate the histological margin assessment and explain the high rate of local recurrences (2). Histologically, DFSP is a spindle-cell tumour with often storiform growth pattern and low proliferation rate. The treatment of choice is complete excision of the tumour by micrographic surgery (MS) or wide local excision (WLE) with safety margins of 2–3 cm (3, 4). MS removes cancerous cells, under 3-dimensional microscopic control, until clear margins are achieved and preserves as much of the healthy tissue as possible (5, 6). This results in a smaller defect size, better cosmetic outcome and lower recurrence rate compared with WLE (2, 7, 8).
DFSP is usually fixed to the overlying skin, but recurrent and long-standing tumours may invade deeper structures, such as the fascia, skeletal muscle, and bone (9). Based on experiences with WLE, the excision of the deep fascia (hereinafter referred as “fascia”) seems important to achieve tumour clearance (10), and the European consensus-based interdisciplinary guideline recommends this procedure even independently of the surgical technique (11). On the other hand, the necessity of the fascia resection in the context of MS has not yet been studied systematically and is not addressed in the German DFSP guideline (4). A recent update on the treatment of DFSP proposed that the fascia may be preserved in superficial tumours (12) and this approach has been followed in our clinic for many years.
We report here our experience and clinical outcomes of 48 patients with primary DFSP who were treated with MS. The aim of this study was to determine whether and for which tumours the preservation of the fascia is feasible and safe and which clinical factors are associated with extension of DFSP beyond the subcutis.
MATERIALS AND METHODS
A retrospective review of the dermatopathology database of the Department of Dermatology of the University Hospital Tübingen was performed between 2004 and 2017, and 48 patients with a diagnosis of primary DFSP and at least 2-year follow-up were identified. All patients were treated with MS under tumescent anaesthesia. Primary excisions included at least the subcutaneous fat, and deeper layers were removed if deemed necessary by the surgeon. Surgical specimens were formalin-fixed and paraffin-embedded for an improved interpretation of the histology. Excisions were repeated until all margins were reported tumour-free (5). After the first resection, the wound was either temporarily covered until the final margins were confirmed to be negative, or primarily closed if negative margins were likely.
All excision specimens of the primary tumour and recurrences were histologically reviewed to confirm the diagnosis and to evaluate the margins and depth of the excision. The microscopic excision depth was compared with the data in the surgical reports, and in the case of discrepant findings, the histological excision depth was considered. If the tumour extent could not be determined from the separately embedded tumour because it reached the lower margin, additional step sections were made from the separately embedded base to determine the maximum tumour depth. Tumour specimens and margins were routinely evaluated by haematoxylin and eosin staining and immunohistochemistry with CD34 antibody (CD34 class II, clone QBEnd-10, dilution 1:100, Dako/Agilent, Santa Clara, CA, USA) was performed on an automated immunostainer (Leica Bond-MAX, Leica Biosystems, Nussloch, Baden-Wuerttemberg, Germany) when required. Clinical information was retrieved from medical records, and tumour size, margin width, number and maximum depth of the excisions were determined from the operative reports. Postoperative follow-up included a physical examination and sonography of the regional lymph nodes every 6 months for 3 years and every 12 months thereafter for at least 2 years.
Statistical calculations were performed with IBM SPSS version 26, and p-values < 0.05 were considered statistically significant. Univariate analyses were performed with the χ2 test or Fisher’s exact test, when appropriate. The study was approved by the ethics committee of the University Hospital Tübingen (project number 091/2020BO2).
RESULTS
Clinicopathological data
The clinicopathological data are summarized in Table I. A total of 48 patients (26 (54%) female and 22 (46%) male) with primary DFSP were treated with MS. Median age at diagnosis was 43 years (interquartile range (IQR) 31–50 years) and median follow-up time was 50 months (IQR 37–73). No metastases were recorded during the study period. Most tumours were located on the trunk (65%), followed by the head and neck area (15%), lower extremities (13%), and upper extremities (8%). A total of 108 excisions were performed on 48 patients and all tumours could be completely excised. Ten patients underwent outpatient surgery only and the remaining 38 patients were admitted as inpatients. Overall, complete excision, wound closure and postoperative surveillance required a median length of hospital stay (both outpatient and inpatient presentations) of 4 days (range 1–30). Closure techniques included direct closure (88%), local flaps (6%), skin grafts (4%), and healing by secondary intention (2%).
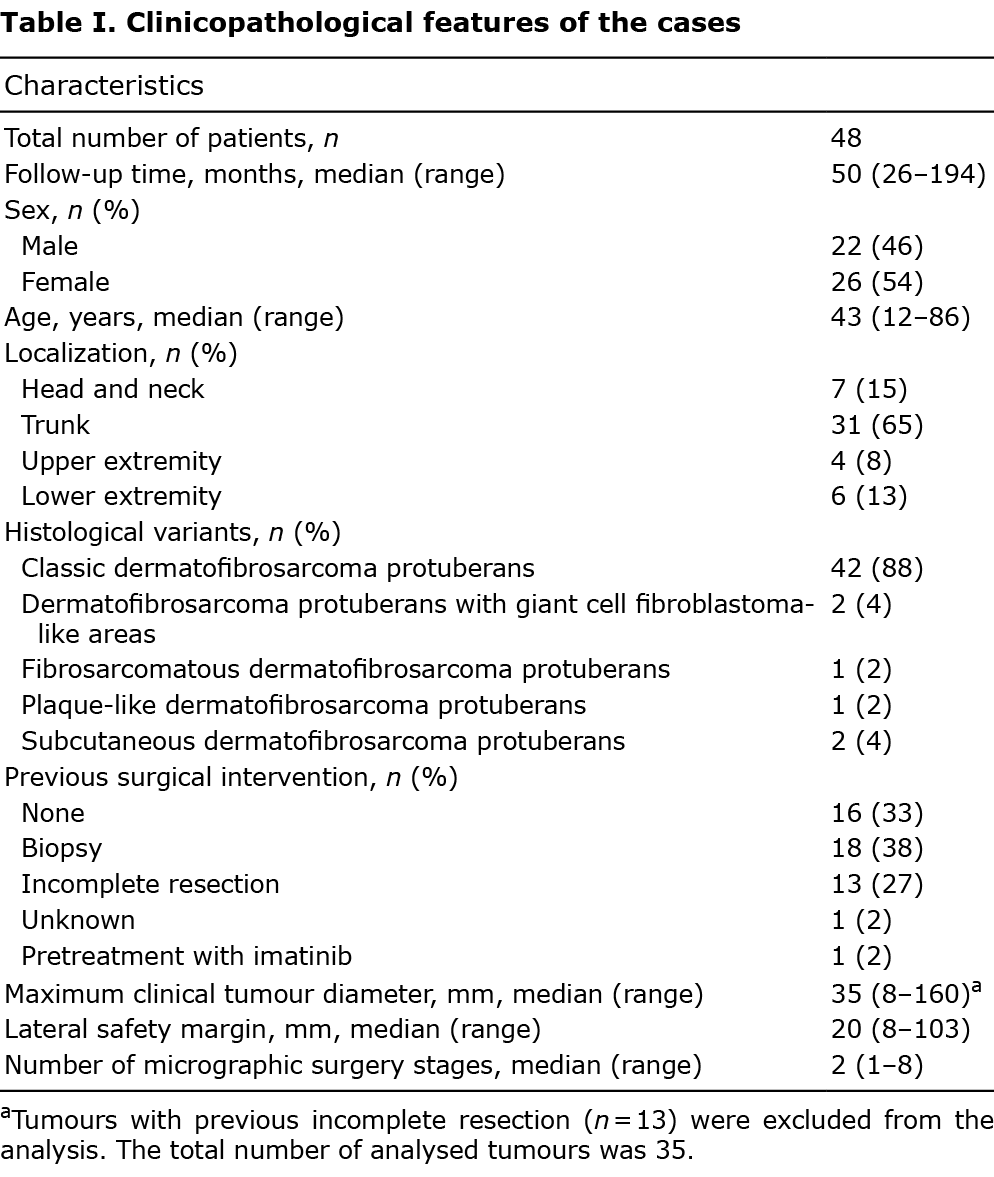
Before the patients were referred to our clinic, tumours had already been biopsied or incompletely excised in 65% of cases, and one patient had been pre-treated with imatinib (Table II, case 4).

Comparison of excision depth with depth of tumour extension
Table II compares the maximum histological resection depth with the maximum depth of tumour extension. Sixty percent of DFSP on the extremities, and 48% of tumours on the trunk, but none of the tumours in the head and neck area, were completely excised above the fascia (Fig. 1). Two tumours (4%) were situated completely in the reticular dermis, 37 tumours (77%) infiltrated the subcutis, 4 tumours (8%) the fascia, and 5 tumours (10%) muscle, galea aponeurotica and periosteum, respectively. Tumour extension was confined to the dermis and/or subcutis in 93% of cases on the trunk and extremities, but in only 14% of cases in the head and neck area (Fig. 2). Tumour localization was the only significant risk factor (p < 0.001) for tumour extension beyond the subcutis in a univariate analysis (Table III).



Two patients (4%) with DFSP on the head had a local recurrence after 11 and 94 months, respectively. In both cases, review of the original slides and supplemental CD34 immunostains showed residual tumour in the margins. The recurrences could be completely excised with MS and no further recurrences were recorded. None of the 21 tumours that were completely excised above the fascia recurred after a median follow-up time of 50 (IQR 37–65) months. Tumours in the head and neck area had a significantly higher recurrence rate (2/7, 29%) than tumours on other sites (0/41; p = 0.019).
Maximum histological excision depth and tumour extension did not differ significantly with respect to the macroscopically visible tumour size (maximum tumour diameter) and there was no significant correlation between maximum tumour diameter and width of surgical margins (Fig. S1).
DISCUSSION
DFSP is a mesenchymal tumour of intermediate malignancy, and is typically located in the reticular dermis and subcutis (2, 13). Surgical treatment of DFSP is challenging, as the tumour diffusely infiltrates the surrounding tissue and may also affect deeper structures (9). Complete excision with meticulous histological evaluation of all peripheral and deep margins is the mainstay of DFSP treatment (11). A systematic review assessed the efficacy of MS for the treatment of DFSP and found a lower recurrence rate after MS (1.11%; 95% confidence interval (95% CI), 0.02–6.03%) compared with WLE (6.32%; 95% CI, 3.19–11.02%) (7).
MS is based on the adjustment of surgical margins according to the individual tumour growth. The advantage over WLE lies not only in the tissue-sparing properties, but particularly in the precise tumour mapping with almost complete visualization of the margins. In contrast, it is estimated that less than 0.5% of the actual resection margin is histologically evaluated after conventional excision (14). These differences explain the superior outcome of MS compared with WLE despite reduced peripheral safety margin (7, 15). Serial excisions by MS until tumour-free margins are achieved is a well-established method in surgical therapy for cutaneous malignancies (16). If the principle of MS is trusted, there is no rationale to do this only for horizontal and not also for vertical tumour extensions and to require here the excision of an additional layer, such as the fascia.
Based on current data, it is unclear whether microscopically controlled complete excision of DFSP with sparing of the fascia is safe, as previous studies either categorically removed the fascia (17) or did not comment on the resection status of the fascia (18, 19). This lack of evidence may explain why the current European consensus-based interdisciplinary guideline for the treatment of DFSP recommends the removal of the fascia independently of the surgical technique (11).
The current study shows that: (i) preservation of the fascia is safe in case of tumour extension not beyond the subcutis; and (ii) the infiltration depth of DFSP depends on localization. The current data demonstrate that 93% of tumours (38/41) on the trunk and extremities, but only 14% of tumours (1/7) in the head and neck area, were confined to the dermis and subcutis. Overall, 81% of tumours (41/48) did not extend beyond the subcutis, which is consistent with previous studies in which 77% of DFSP neither showed neuromuscular, osseous (20) nor fascia infiltration (10). However, site-dependent differences in the tumour extension were not investigated in any of these studies. The histological analysis in the current study shows that the vast majority of tumours could have been removed completely above the fascia, and deeper excisions were required in only a minority of tumours, most of which were located on the head. Furthermore, there is no evidence that preserving the fascia is associated with an increased risk of recurrence.
The fascia is only a thin barrier against tumour invasion (21), and infiltration of the fascia without deeper growth was the exception in the current study (8% of DFSP). This observation does not seem to be related to the predominance of epifascial tumours in the current study cohort. Llombart et al. (22) examined overall larger and partly fibrosarcomatous transformed DFSP, of which 59% were localized above the fascia and 29% infiltrated the muscle and periosteum. However, even in this study, infiltration of the fascia without growth beyond was found in only 12% of cases. DFSP usually arises in the reticular dermis and almost invariably involves the subcutis, which results in a characteristic histological honeycomb appearance (2). The thickness of the subcutis therefore plays a crucial role in how fast the tumour infiltrates deeper structures and this may explain why tumours at localizations with thin subcutis (head and neck) are more likely to infiltrate fascia and muscle than those at localizations with thicker subcutis (trunk and extremities). Moreover, it has been shown that subcutaneous DFSP, a rare subtype with no or only minimal dermal involvement and frequent infiltration of the muscle and periosteum, has a predilection for the head (22). Although, in the current study, none of the tumours on the head met the strict criteria of subcutaneous DFSP (23), as more than minimal dermal involvement was identified on step sections, it was still notable that the dermal portion of these tumours was usually less pronounced and the centre of these tumours deeper than that of tumours outside the head (Fig. 1). This could additionally contribute to a more infiltrative growth.
Recently, Hao et al. (12) proposed in an update on the diagnosis and treatment of DFSP that superficial tumours without invasion of the underlying fascia “may be directly excised without dissecting underlying fascia”. However, how superficial and deep tumours can be differentiated preoperatively is unclear. The current study demonstrates that tumour localization, but not the macroscopically visible tumour size, is a good surrogate parameter for this classification. The need for a site-specific adjustment of the excision depth has already been recognized by other authors. Parker et al. (24) showed in their case series that all tumours on the scalp and forehead required excisions through the periosteum, whereas those at other locations could be completely removed by cutting through the fascia. The current study comes to similar conclusions, but questions the categorical necessity of the fascia resection in the setting of MS. The superficial location of DFSP on the trunk and extremities suggests that primary excision of these tumours down to, but not including, the fascia is sufficient in most cases. Deeper excisions can then be performed in a second step according to the histological margin assessment if necessary. Tumours in the head and neck showed an overall more infiltrative growth and a greater variation in infiltration depth, ranging from predominantly subcutaneous tumours to tumours infiltrating into the periosteum. This underscores the need for individualized treatment concepts in this area and that MS with its accurate mapping of tumour extensions is the method of choice. Even though excising the fascia does not add significant morbidity in most cases, there are sensitive locations (flexures, e.g. groin, face and neck) where the fascia has a relationship to important nerves and vessels (25). Thus, sparing the fascia may also result in fewer postoperative complications and reduced morbidity. The fascia is not a meaningless muscle envelope, but is richly vascularized and contains well-developed lymphatic channels (26). It has been shown that preservation of the fascia reduces the incidence of postoperative lymphoedema after lymph node dissection (27) and leads to fewer seromas, less time until drain removal, drain output and shorter hospital stay after abdominoplasty (28). In addition, fascia-derived stem cells may represent a source for musculoskeletal tissue repair (29) and it has been shown that scars are more severe when the fascia is injured surgically (30).
The recurrence rate in the current study (4%) is in line with previously published case series despite a less aggressive surgical approach (7). It is noteworthy that both patients with local recurrences in our study had positive microscopic margins. This demonstrates that, if follow-up is sufficiently long, even small tumour remnants can lead to recurrences and confirms the findings of Bowne et al. (20) who identified positive margins as the most important risk factor for local recurrence in a multivariate analysis.
Limitations
This study has several limitations. The follow-up time may not be long enough to record all local recurrences. Recurrent tumours after MS tend to occur later than those after WLE and the mean time to occurrence was 68 months after MS in a systematic review (2, 7). Furthermore, the tumours in this retrospective study were not removed strictly according to uniform criteria. Some epifascial tumours were removed including the fascia or muscle according to the individual evaluation of the surgeon, while others were removed above the fascia. Thus, it cannot be excluded that more infiltrating tumours were treated more aggressively. Importantly, the results of the current study are from a single institution and a broader application of the method will ultimately require external validation at other centres.
Conclusion
This study shows that MS of DFSP allows the identification of cases with possibility of fascia preservation and confirms site-specific differences in the infiltration pattern of DFSP, which should be incorporated in surgical planning.
ACKNOWLEDGEMENTS
The authors thank Petra Leber and Corinna Kirchner for providing excellent technical assistance.
Conflicts of interest. MG reports grants and personal fees from Novartis, outside the submitted work. UL reports personal fees from Roche, personal fees from Novartis, personal fees from Sun Pharma, grants and personal fees from MSD, outside the submitted work. MH reports personal fees from Janssen-Cilag, outside the submitted work. SF reports personal fees from Takeda, outside the submitted work. CG reports personal fees from Amgen, grants and personal fees from BMS, personal fees from MSD, grants and personal fees from Novartis, grants and personal fees from NeraCare, personal fees from Philogen, grants from Roche, grants and personal fees from Sanofi, outside the submitted work. All other authors have no conflicts of interest to declare.
REFERENCES
- Thway K, Noujaim J, Jones RL, Fisher C. Dermatofibrosarcoma protuberans: pathology, genetics, and potential therapeutic strategies. Ann Diagn Pathol 2016; 25: 64–71.
- Bogucki B, Neuhaus I, Hurst EA. Dermatofibrosarcoma protuberans: a review of the literature. Dermatol Surg 2012; 38: 537–551.
- Monnier D, Vidal C, Martin L, Danzon A, Pelletier F, Puzenat E, et al. Dermatofibrosarcoma protuberans: a population-based cancer registry descriptive study of 66 consecutive cases diagnosed between 1982 and 2002. J Eur Acad Dermatol Venereol 2006; 20: 1237–1242.
- Ugurel S, Kortmann RD, Mohr P, Mentzel T, Garbe C, Breuninger H, et al. S1 guidelines for dermatofibrosarcoma protuberans (DFSP) – update 2018. J Dtsch Dermatol Ges 2019; 17: 663–668.
- Breuninger H, Schaumburg-Lever G. Control of excisional margins by conventional histopathological techniques in the treatment of skin tumours. An alternative to Mohs’ technique. J Pathol 1988; 154: 167–171.
- Moehrle M, Breuninger H, Rocken M. A confusing world: what to call histology of three-dimensional tumour margins? J Eur Acad Dermatol Venereol 2007; 21: 591–595.
- Foroozan M, Sei JF, Amini M, Beauchet A, Saiag P. Efficacy of Mohs micrographic surgery for the treatment of dermatofibrosarcoma protuberans: systematic review. Arch Dermatol 2012; 148: 1055–1063.
- Hafner HM, Moehrle M, Eder S, Trilling B, Rocken M, Breuninger H. 3D-Histological evaluation of surgery in dermatofibrosarcoma protuberans and malignant fibrous histiocytoma: differences in growth patterns and outcome. Eur J Surg Oncol 2008; 34: 680–686.
- Gloster HM, Jr. Dermatofibrosarcoma protuberans. J Am Acad Dermatol 1996; 35: 355–374; quiz 375–356.
- Fields RC, Hameed M, Qin LX, Moraco N, Jia X, Maki RG, et al. Dermatofibrosarcoma protuberans (DFSP): predictors of recurrence and the use of systemic therapy. Ann Surg Oncol 2011; 18: 328–336.
- Saiag P, Grob JJ, Lebbe C, Malvehy J, del Marmol V, Pehamberger H, et al. Diagnosis and treatment of dermatofibrosarcoma protuberans. European consensus-based interdisciplinary guideline. Eur J Cancer 2015; 51: 2604–2608.
- Hao X, Billings SD, Wu F, Stultz TW, Procop GW, Mirkin G, et al. Dermatofibrosarcoma protuberans: update on the diagnosis and treatment. J Clin Med 2020; 9: 1752.
- McPeak CJ, Cruz T, Nicastri AD. Dermatofibrosarcoma protuberans: an analysis of 86 cases – five with metastasis. Ann Surg 1967; 166: 803–816.
- van Delft LCJ, Nelemans PJ, van Loo E, Abdul Hamid M, Kelleners-Smeets NWJ. The illusion of conventional histological resection margin control. Br J Dermatol 2019; 180: 1240–1241.
- Lowe GC, Onajin O, Baum CL, Otley CC, Arpey CJ, Roenigk RK, et al. A comparison of Mohs micrographic surgery and wide local excision for treatment of dermatofibrosarcoma protuberans with long-term follow-up: the Mayo Clinic Experience. Dermatol Surg 2017; 43: 98–106.
- Tolkachjov SN, Brodland DG, Coldiron BM, Fazio MJ, Hruza GJ, Roenigk RK, et al. Understanding Mohs micrographic surgery: a review and practical guide for the nondermatologist. Mayo Clin Proc 2017; 92: 1261–1271.
- Ratner D, Thomas CO, Johnson TM, Sondak VK, Hamilton TA, Nelson BR, et al. Mohs micrographic surgery for the treatment of dermatofibrosarcoma protuberans. Results of a multiinstitutional series with an analysis of the extent of microscopic spread. J Am Acad Dermatol 1997; 37: 600–613.
- Paradisi A, Abeni D, Rusciani A, Cigna E, Wolter M, Scuderi N, et al. Dermatofibrosarcoma protuberans: wide local excision vs. Mohs micrographic surgery. Cancer Treat Rev 2008; 34: 728–736.
- Wacker J, Khan-Durani B, Hartschuh W. Modified Mohs micrographic surgery in the therapy of dermatofibrosarcoma protuberans: analysis of 22 patients. Ann Surg Oncol 2004; 11: 438–444.
- Bowne WB, Antonescu CR, Leung DH, Katz SC, Hawkins WG, Woodruff JM, et al. Dermatofibrosarcoma protuberans: a clinicopathologic analysis of patients treated and followed at a single institution. Cancer 2000; 88: 2711–2720.
- Kawaguchi N, Ahmed AR, Matsumoto S, Manabe J, Matsushita Y. The concept of curative margin in surgery for bone and soft tissue sarcoma. Clin Orthop Relat Res 2004; 419: 165–172.
- Llombart B, Serra-Guillen C, Rubio L, Nagore E, Requena C, Traves V, et al. Subcutaneous dermatofibrosarcoma protuberans, a rare subtype with predilection for the head: a retrospective series of 18 cases. J Am Acad Dermatol 2017; 77: 503–511.e1.
- Diaz-Cascajo C, Weyers W, Rey-Lopez A, Borghi S. Deep dermatofibrosarcoma protuberans: a subcutaneous variant. Histopathology 1998; 32: 552–555.
- Parker TL, Zitelli JA. Surgical margins for excision of dermatofibrosarcoma protuberans. J Am Acad Dermatol 1995; 32: 233–236.
- Dzubow LM. The fasciae of the face: an anatomic and histologic analysis. J Am Acad Dermatol 1986; 14: 502–507.
- Stecco C, Tiengo C, Stecco A, Porzionato A, Macchi V, Stern R, et al. Fascia redefined: anatomical features and technical relevance in fascial flap surgery. Surg Radiol Anat 2013; 35: 369–376.
- Lawton G, Rasque H, Ariyan S. Preservation of muscle fascia to decrease lymphedema after complete axillary and ilioinguinofemoral lymphadenectomy for melanoma. J Am Coll Surg 2002; 195: 339–351.
- Xiao X, Ye L. Efficacy and safety of scarpa fascia preservation during abdominoplasty: a systematic review and meta-analysis. Aesthetic Plast Surg 2017; 41: 585–590.
- Wong HL, Siu WS, Fung CH, Zhang C, Shum WT, Zhou XL, et al. Characteristics of stem cells derived from rat fascia: in vitro proliferative and multilineage potential assessment. Mol Med Rep 2015; 11: 1982–1990.
- Jiang D, Christ S, Correa-Gallegos D, Ramesh P, Kalgudde Gopal S, Wannemacher J, et al. Injury triggers fascia fibroblast collective cell migration to drive scar formation through N-cadherin. Nat Commun 2020; 11: 5653.