Trichotillomania is formally classified as a mental health disorder, but it is commonly diagnosed by dermatologists. The aim of this systematic review is to assess the diagnostic value of trichoscopy in diagnosing trichotillomania. The analysis identified the 7 most specific trichoscopic features in trichotillomania. These features had the following prevalence and specificity: trichoptilosis (57.5%; 73/127 and 97.5%, respectively), v-sign (50.4%; 63/125 and 99%), hook hairs (43.1%; 28/65 and 100%), flame hairs (37.1%; 52/140 and 96.5%), coiled hairs (36.8%; 46/125 and 99.6%), tulip hairs (36.4%; 28/77 and 89.6%), and hair powder (35.6%; 42/118 and 97.9%). The 2 most common, but least specific, features were broken hairs and black dots. In conclusion, trichoscopy is a reliable new diagnostic method for hair loss caused by hair pulling. Trichoscopy should be included as a standard procedure in the differential diagnosis of trichotillomania in clinical practice.
Key words: trichotillomania; hair-pulling disorder; trichoscopy; dermoscopy; dermatoscopy.
Accepted Jun 28, 2021; Epub ahead of print Jun 29, 2021
Acta Derm Venereol 2021; 101: adv00565.
doi: 10.2340/00015555-3859
Corr: Lidia Rudnicka, Department of Dermatology, Medical University of Warsaw, Koszykowa 82A, PL-02-008 Warsaw, Poland. E-mail: lidia. rudnicka@dermatolodzy.com.pl
SIGNIFICANCE
Trichotillomania is a hair loss condition, which is classified as a mental health disorder. The affected person pulls out their own hair until areas of alopecia are visible on the scalp. The patient (often a child) is usually not likely to admit that they are pulling their own hair. This review determined 7 hair-related features that can help the dermatologist identify hair pulling and protect the patient from being misdiagnosed and mistakenly treated as having alopecia areata (which is hair loss with similar appearance). The hair abnormalities are visible when using a special non-invasive magnifying technique, called trichoscopy.
Trichotillomania (hair-pulling disorder) is characterized by a recurring habit of pulling out of one’s hair, resulting in hair loss (1). Diagnosis of trichotillomania is usually based on clinical examination. According to the Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-5) criteria trichotillomania belongs to the obsessive-compulsive and related disorders group. The DSM-5 diagnostic criteria for trichotillomania are: (i) recurrent pulling out of one’s hair, resulting in hair loss; (ii) repeated attempts to decrease or stop hair pulling; (iii) the hair pulling causes clinically significant distress or impairment in social, occupational, or other important areas of functioning; (iv) the hair pulling or hair loss is not attributable to another medical condition (e.g. a dermatological condition); and (v) the hair pulling is not better explained by the symptoms of another mental disorder (e.g. attempts to improve a perceived defect or flaw in appearance in body dysmorphic disorder) (2). Patients visiting dermatologists’ offices often do not fulfil these psychiatric criteria. In a significant proportion of patients only criterion (i) is fulfilled (3). Clinically, trichotillomania presents as a patchy alopecia (4, 5). The pull-test is negative (3, 5). The scalp is the most common location (72.8%) (4). The vertex area is commonly affected with a so-called tonsure or “Friar Tuck” pattern of baldness (3, 5). Other common locations of trichotillomania include eyebrows (56.4%), eyelashes (52.6%), and pubic area (50.7%) (4). Beard is rarely affected (4.3%) (4). Diagnosis of trichotillomania can be challenging, especially when patients deny or are unaware of hair pulling or do not meet all the psychiatric criteria.
Trichoscopy is widely used to diagnose patients with hair and scalp disorders (3, 6). Several studies were performed to identify the typical trichoscopic features of trichotillomania. However, no large-scale analysis of the specificity and sensitivity of trichoscopic findings in trichotillomania has been performed to date. The aim of this study was to evaluate the role of trichoscopy in diagnosing trichotillomania by identifying characteristic trichoscopic features of the disease and assessing the sensitivity and specificity of each trichoscopic finding.
MATERIALS AND METHODS
A literature review was performed by searching 3 databases: PubMed, Scopus and EBSCO. The search terms “trichotillomania” and “hair pulling disorder” combined with “trichoscopy”, “dermoscopy”, “dermatoscopy”, “videodermoscopy” or “videodermatoscopy” were used. Moreover, references of all relevant articles were checked for further publications. Original studies and case series published in English were eligible for quantitative analysis. Trichoscopic features that were reported in at least 10 patients with trichotillomania in studies with a control group were included in the quantitative analysis. If the study was conducted using both polarized and non-polarized trichoscopy, the data from polarized mode was used in this analysis. Studies with incomplete epidemiological data, such as unknown number of patients or frequency of trichoscopic findings, case reports, animal studies, reviews or book chapters were excluded. Articles considering the frequency of trichoscopic features based on the number of patches instead of the number of patients were also excluded (Fig. 1). The review presents the frequency of the most characteristic trichoscopic features of trichotillomania. Their sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated. The review also considers trichoscopic findings that are commonly observed, but are not disease-specific. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors. Prevalence ranges and prevalence mean values are based on all studies in which particular trichoscopic features were evaluated. Sensitivity, specificity, PPV, NPV are based only on original studies that included patients with trichotillomania and other hair diseases. Calculation methods are shown below:
|
Mean value= |
Number of patients with trichotillomania (TTM) and given feature |
|
Total number of patients with TTM |
|
|
Sensitivity= |
Number of patients with TTM and given feature |
|
Number of patients with TTM and given feature + Number of patients with TTM without given feature |
|
|
Specificity= |
Number of patients without TTM and without given feature |
|
Number of patients without TTM and without given feature + Number of patients without TTM with given feature |
|
|
PPV= |
Number of patients with TTM and given feature |
|
Number of patients with TTM and given feature + Number of patients without TTM with given feature |
|
|
NPV= |
Number of patients without TTM and without given feature |
|
Number of patients without TTM and without given feature + Number of patients with TTM without given feature |

RESULTS
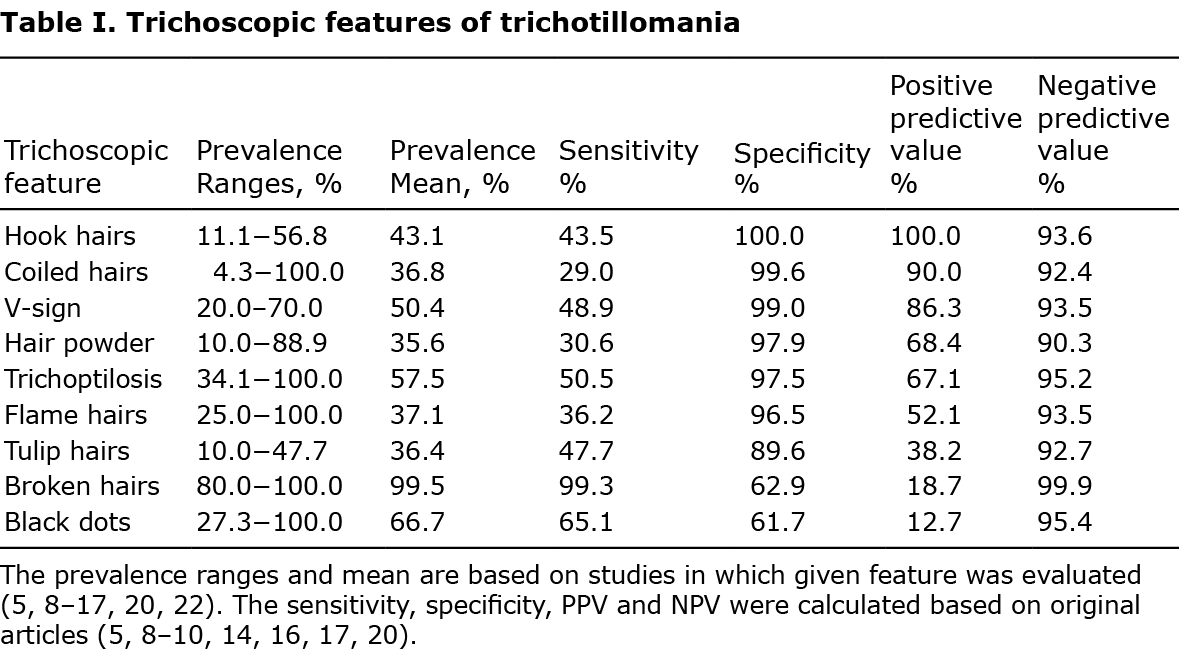
The review found 13 articles (10 original studies and 3 case series), which were selected and included in the quantitative analysis, as shown on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram in Fig 1. Overall, 203 patients with trichotillomania were included in the systematic review. The results of the quantitative analysis are shown in Table I and described below.
Trichoscopic findings in trichotillomania
Trichoptilosis. Trichoptilosis presents as longitudinal splitting of fractured distal hair shafts. It is a common finding in healthy, long hairs that have not been cut for a while, but in trichotillomania it affects short hairs instead. It can occasionally be detected in different types of alopecia, including traction alopecia, alopecia areata, tinea capitis, and primary cicatricial alopecias (3, 7). The incidence rate of trichoptilosis varied between 34.1% and 100% (mean 57.5% (73/127)) of patients with trichotillomania (5, 8–13).
V-sign. This term was introduced by Rudnicka et al. in 2012 (3). A v-sign is formed when 2 or more hair shafts of a single follicular unit are pulled simultaneously and break at the same length above the scalp’s surface. Normal, regrowing terminal hairs after shaving may look similar, but they cover the whole field of view, whereas the v-sign in trichotillomania is surrounded by long terminal hairs (5). The v-sign is another feature that is characteristic of trichotillomania, with an estimated specificity of 99%. The frequency of the v-sign in trichotillomania varied between 20% and 70% (mean 50.4% (63/125)) (5, 9, 11, 13–16).
Hook hairs. Hook hairs or question mark hairs are partially coiled hairs (5). They are the most specific finding of trichotillomania, with the frequency of 11.1–56.8% (mean 43.1% (28/65)) (5, 14, 15). Hook hairs were also reported in traction alopecia (3).
Flame hairs. Flame hairs result from traumatic pulling anagen hairs. They are observed as hair residues that are semi-transparent, wavy and cone-shaped. Flame hairs were first described by Rakowska et al. (5) in 2014 and suggested as a specific sign for trichotillomania. In analysed studies they were detected in patients with trichotillomania with the incidence rate between 25% and 100% (mean 37.1% (52/140)) (5, 9, 11, 13–15, 17). However, flame hairs were also described in acute chemo- and radiotherapy-induced alopecias, alopecia areata, traction alopecia, and central centrifugal cicatricial alopecia (17, 18).
Coiled hairs. Coiled hairs are broken telogen/catagen hairs that curl back (19). They are similar to pigtail hairs, but can be distinguished by their irregular appearance and frequently frayed ends (5). Coiled hairs are highly specific of trichotillomania (99.6%), with the incidence rate varying between 4.3% and 100% (mean 36.8% (46/125)) (5, 8, 9, 11–14). They can also be observed in traction alopecia (3).
Tulip hairs. Tulip hairs were first named by Rakowska et al. (5) in 2014. They are described as short hairs with darker, tulip flower shaped ends, which form due to diagonal hair shaft fracture (5). The frequency of tulip hairs in trichotillomania varied between 10% and 47.7% (mean 36.4% (28/77)) (5, 11, 13, 15). They can be found in alopecia areata and traction alopecia (3, 5).
Hair powder. Hair powder (black powder/sprinkled hairs) is another term introduced by Rakowska et al. (5) in 2014. It develops as a result of total hair shaft damage, when only a sprinkled hair residue is visible (5). The incidence rate of hair powder in trichotillomania was estimated between 10% and 88.9% (mean 35.6% (42/118)) (5, 9, 11, 13–15). Recently, hair powder was described in traction alopecia and alopecia areata (9, 14).
Broken hairs. Broken hairs were detected in almost every case of trichotillomania (mean 99.5%; 182/183), but they have a low calculated PPV (18.7%) (5, 8–12, 14–16, 20–22). They are common in other alopecias, especially traction alopecia, alopecia areata, and tinea capitis. In trichotillomania and traction alopecia hairs are broken at different levels above the scalp, which can be useful in making the diagnosis (3, 5, 9, 10, 13, 14).
Black dots. Black dots were detected in 27.3–100% of patients with trichotillomania (mean 66.7% (122/183)) with a low calculated PPV (12.7%) (5, 8–16, 20–22). Black dots are pigmented residues of hairs broken or destroyed at the scalp level (3). They are not specific and can be recognized in alopecia areata, chemotherapy-induced alopecia, dissecting cellulitis, tinea capitis, and traction alopecia (18, 23–25). According to Rakowska et al. (5) black dots found in trichotillomania and tinea capitis are variable in diameter and shape (round, oval, irregular), whereas those in alopecia areata tend to be similar in size and shape.
Yellow dots with black peppering. Yellow dots with black peppering (containing a black dot, mostly in the central part), were first described in trichotillomania by Inui et al. (21) in 2008. Isolated cases were also reported in alopecia areata (5, 9). As they were present only in 11% (8/73) of patients with trichotillomania, they were not included in the quantitative analysis. In contrast, yellow dots without black peppering are mainly associated with alopecia areata, but can also be found in androgenetic alopecia, chronic cutaneous lupus erythematosus, and dissecting cellulitis (26). In trichotillomania, they were described as very sparse and irregularly distributed, unlike most cases of alopecia areata (5).
Burnt match-stick sign. The sign was first reported by Malakar et al. (22) in 2017, as a dark bulbar proximal tip with a linear stem of variable length. As there were only 4 cases described in the literature (3 in trichotillomania and 1 in traction alopecia (14, 22)) this feature was not included in the evaluation of specificity and sensitivity.
Haemorrhages. The first description of haemorrhages in trichoscopy of trichotillomania was published in a case report by Peralta & Morais (27) in 2012. They show as a red, perifollicular dots and are caused by traumatic hair pulling (11). In the study conducted by Elmas et al. (13), hemorrhages were detected in 40% (8/20) of the patients with trichotillomania. Moreover, follicular micro-haemorrhages were described as a unique sign for detecting coexisted trichotillomania in patients with alopecia areata, since these conditions often coexist (11, 28, 29).
Mace sign. This sign was first described in 3 cases by Malakar et al. (15) in 2016, and suggested as an exclusive sign of trichotillomania. The mace sign presents as broken terminal hairs, which are uniform in diameter and pigmentation with a bulging distal end that resembles a mace. In the study performed by Elmas et al. (13) the mace sign was reported in 45% (9/20) of patients with trichotillomania.
Branched hairs. The term branched hairs was introduced in 2020 by Elmas et al. (13). Branched hairs are described as hair shafts with obliquely detached pieces. They form as a result of pushing hair shafts linearly from the distal to the proximal end. They were reported in 40% (8/20) of patients with trichotillomania (13).
Concentric hairs. Concentric hairs are another novel finding, described by Elmas et al. (13). Concentric hairs are broken hairs presenting as a central black dot surrounded with a black circle. They are probably caused by attenuation of hair cortex associated with repetitive trauma. They were described in 35% (7/20) of patients with trichotillomania (13).
Angulated hairs. Angulated hairs is a term introduced in 2017 by Khunkhet et al. (9). They are described as fractured hairs forming a sharp angle along the hair shaft, regardless of the number of fracture sites. The term covers zigzag hairs, checkmark hairs, and trichorrhexis nodosa (9). In 2020, Elmas et al. (13) reported this sign in 40% (8/20) of patients with trichotillomania.
Exclamation mark hairs. Exclamation mark hairs are rare in trichotillomania. They are described as hairs with thin proximal ends and thicker distal ends. Exclamation mark hairs are a hallmark feature of alopecia areata (30); however, they can also be present in trichotillomania, tinea capitis, chemotherapy-induced alopecia, anagen effluvium, and severe intoxication (31). According to Rudnicka et al. (3) there are slight differences between exclamation mark hairs in these 2 diseases; in trichotillomania they tend to have a flat distal end and a pigmented proximal end, whereas in alopecia areata they usually have an uneven, ragged, distal end and a hypopigmented proximal end. Exclamation mark hairs were observed in 33.3% (23/69) of patients with trichotillomania, with sensitivity 80.8% and PPV of only 11.4%.
Other trichoscopic findings
Other reported trichoscopic features of trichotillomania were not characteristic or common. They included: upright re-growing hairs, vellus hairs, and yellow dots.
Locations other than scalp
Trichotillomania may affect any site of the body (32). According to available case reports, trichoscopic features of eyebrows and scalp trichotillomania are similar, and include: irregularly broken hairs, black dots, coiled hairs, hook hairs, trichoptilosis, v-sign, flame hairs, tulip hairs, yellow dots, and haemorrhages (33, 34). Trichoscopy of eyelashes trichotillomania presents irregularly broken hairs, black dots, and flame hairs (35). In beard trichotillomania, a new trichoscopic finding called the ”pluck out sign” has recently been described in the literature. It consists of round haemorrhages around hair shafts and, according to the authors, can be very suggestive of trichotillomania (4, 36).
Monitoring of treatment
In patients with trichotillomania, a significant increase in capillary density, the presence of i-hairs and hairs in the growth phase were reported in the 6-month follow-up. I-hair has been a suggested marker of the trichotillomania remission. It presumably is a modified black dot, developing into a normal hair as the condition improves (37, 38).
DISCUSSION
This systematic review was conducted to systematize current knowledge about the trichoscopic pattern of trichotillomania. This analysis revealed the 7 most characteristic trichoscopic findings: trichoptilosis (present in 57.5% of patients), v-sign (50.4%), hook hairs (43.1%), flame hairs (37.1%), coiled hairs (36.8%), tulip hairs (36.4%), and hair powder (35.6%) (Fig. 2). Hook hairs, coiled hairs and v-sign have the highest calculated PPV (100%, 90% and 86.3%, respectively). Thus, their presence is highly indicative of trichotillomania. Although, in the current analysis, hook hairs were present only in patients with trichotillomania, they were also described in patients with traction alopecia. Thus, hook hairs should not be considered as a pathognomonic sign of trichotillomania (3).

The most common trichoscopic findings in trichotillomania were broken hairs and black dots. However, these features are not specific for trichotillomania (3).
A relatively common, but not highly specific, feature of trichotillomania is tulip hairs. The comparison between the tulip hairs (5) and the subsequently described mace sign (15) is not clear. The mace sign is presented as a bulging at the distal end of a broken hair, with a rough hair shaft that is uniform in pigmentation and darker than surrounding hairs. On the contrary, tulip hair is described as a black mark at tip of the hair with light-coloured hair shaft and dark distal end. These features may indicate that the mace sign is a variant of tulip hairs. The slight differences may result from using trichoscopy with different magnifications.
Based on the results of this analysis it may be suggested that trichoscopy should play a major role in establishing the diagnosis of trichotillomania. The available clinical criteria for trichotillomania were established on the basis of analysing groups of patients who are in psychiatric care. Many patients, in particular children and adolescents, do not all meet the criteria for trichotillomania as described in the DSM-5. Many patients fulfil only criterion (i) of DSM-5 (recurrent pulling out of one’s hair, resulting in hair loss), with no attempts to decrease or stop hair pulling and no psychiatric comorbidities. Furthermore, many patients, in particular children, do not admit recurrent pulling out of their hair, making the correct diagnosis very challenging. The first perceived symptom of the disease is loss of hair; hence dermatologists are usually the first doctors to deal with patients suspected of trichotillomania.
Trichoscopy is likely to be a helpful tool in screening patients with hair loss who are suspected of trichotillomania (3). A rapid in-office diagnosis may also accelerate treatment, which could be important for the patients, who tend to have significant functional impairment and low quality of life (1). Moreover, trichoscopy could avoid the need for semi-invasive diagnostic methods, such as scalp biopsy. In doubtful cases, trichoscopy-guided biopsy may be performed (39). The results of this systematic analysis may serve as indication as to which common trichoscopic features of trichotillomania should be considered when performing a trichoscopy-guided biopsy.
Other trichoscopic features: yellow dots with black peppering (3), burnt match stick sign (14, 22), haemorrhages (11), mace sign (15), branched hairs (13), concentric hairs (13), and angulated hairs (9) were observed in trichotillomania. These features were rare in the global analysis of all published data. Consequently, they were not included in the quantitative analysis. Some of these features may have potential in future differential diagnosis of hair loss, but further studies are needed to evaluate their significance.
This review also collected information about trichoscopic findings of trichotillomania in locations other than the scalp. These findings were similar to features found in the scalp and included irregularly broken hairs, black dots, coiled hairs, hook hairs, trichoptilosis, v-sign, flame hairs, tulip hairs, yellow dots, and various areas of haemorrhages. Güleç et al. (33) described the v-sign in eyebrow trichotillomania. However, eyebrow hairs grow in one-hair follicular units. Therefore, we suggest that the v-sign, observed in the eyebrows, was probably 2 hair shafts emerging from 2 different hair follicles, arranged in a way that imitated the v-sign.
Finally, the current study analysed trichoscopic features that may be helpful in the monitoring treatment efficacy, such as an increase in capillary density, presence of i-hairs and hairs in the growth phase.
This study has some limitations. The number of studies related to trichoscopy of trichotillomania is limited, and some did not include control groups. Various topics have not yet been assessed in clinical studies, including the role of trichoscopy in locations other than the scalp and in monitoring treatment. There are only single reports about those issues and more data is required for a full analysis.
In conclusion, this systematic review found that the 7 most specific trichoscopic findings in trichotillomania are: hook hairs, coiled hairs, v-sign, hair powder, flame hairs, tulip hairs and trichoptilosis. The 2 most common trichoscopic findings are broken hairs and black dots. Diagnosis of trichotillomania is simplified by the fact that, usually, several different features mentioned above are present in a single patient, creating a so-called chaotic trichoscopic pattern. Thus, trichoscopy is a reliable new tool for identifying alopecia associated with hair pulling, and it should be included as a standard procedure in diagnosing trichotillomania.
REFERENCES
- Jafferany M, Patel A. Trichopsychodermatology: the psychiatric and psychosocial aspects of hair disorders. Dermatol Ther 2020; 33: e13168.
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association, 2013: p. 251–257.
- Rudnicka L, Olszewska M, Rakowska A. Atlas of trichoscopy: dermoscopy in hair and scalp disease. London: Springer, 2012: p. 257–275.
- Woods DW, Flessner CA, Franklin ME, Keuthen NJ, Goodwin RD, Stein DJ, et al. The Trichotillomania Impact Project (TIP): exploring phenomenology, functional impairment, and treatment utilization. J Clin Psychiatry 2006; 67: 1877–1888.
- Rakowska A, Slowinska M, Olszewska M, Rudnicka L. New trichoscopy findings in trichotillomania: flame hairs, v-sign, hook hairs, hair powder, tulip hairs. Acta Derm Venereol 2014; 94: 303–306.
- Rudnicka L, Olszewska M, Rakowska A, Kowalska-Oledzka E, Slowinska M. Trichoscopy: a new method for diagnosing hair loss. J Drugs Dermatol 2008; 7: 651–654.
- Malakar S. Trichoscopy: a text and atlas. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd, 2017: p. 73.
- Moneib HA, El-Shiemy SMH, Saudi WM, El-Fangary MM, Nabil T, Mohy SM. Hair loss among a group of Egyptian children: a clinical and dermoscopic study. J Egypt Women’s Dermatol Soc 2017; 14: 9–24.
- Khunkhet S, Vachiramon V, Suchonwanit P. Trichoscopic clues for diagnosis of alopecia areata and trichotillomania in Asians. Int J Dermatol 2017; 56: 161–165.
- Park J, Kim JI, Kim HU, Yun SK, Kim SJ. Trichoscopic findings of hair loss in Koreans. Ann Dermatol 2015; 27: 539–550.
- Ankad BS, Naidu MV, Beergouder SL, Sujana L. Trichoscopy in trichotillomania: a useful diagnostic tool. Int J Trichology 2014; 6: 160–163.
- Thakur BK, Verma S, Raphael V, Khonglah Y. Extensive tonsure pattern trichotillomania-trichoscopy and histopathology aid to the diagnosis. Int J Trichology 2013; 5: 196–198.
- Elmas Ö F, Metin MS. Trichoscopic findings of trichotillomania: new observations. Postepy Dermatol Alergol 2020; 37: 340–345.
- Said M, El-Sayed SK, Elkhouly NDE. Trichoscopic evaluation of frontal hairline recession in Egyptian female patients. J Cosmet Dermatol 2020; 19: 2706–2716.
- Malakar S, Mukherjee SS. ‘Mace sign’ – a definitive sign of trichotillomania? Our Dermatology Online/Nasza Dermatologia Online 2017; 8: 491–492.
- Nikam VV, Mehta HH. A nonrandomized study of trichoscopy patterns using nonpolarized (contact) and polarized (noncontact) dermatoscopy in hair and shaft disorders. Int J Trichology 2014; 6: 54–62.
- Miteva M, Tosti A. Flame hair. Skin Appendage Disord 2015; 1: 105–109.
- Rossi A, Caterina Fortuna M, Caro G, Cardone M, Garelli V, Grassi S, et al. Monitoring chemotherapy-induced alopecia with trichoscopy. J Cosmet Dermatol 2019; 18: 575–580.
- Miteva M, Tosti A. Hair and scalp dermatoscopy. J Am Acad Dermatol 2012; 67: 1040–1048.
- Shim WH, Jwa SW, Song M, Kim HS, Ko HC, Kim BS, et al. Dermoscopic approach to a small round to oval hairless patch on the scalp. Ann Dermatol 2014; 26: 214–220.
- Inui S, Nakajima T, Nakagawa K, Itami S. Clinical significance of dermoscopy in alopecia areata: analysis of 300 cases. Int J Dermatol 2008; 47: 688–693.
- Malakar S, Mukherjee SS. Burnt matchstick sign – a new trichoscopic finding in trichotillomania. Int J Trichology 2017; 9: 44–46.
- Polat M. Evaluation of clinical signs and early and late trichoscopy findings in traction alopecia patients with Fitzpatrick skin type II and III: a single-center, clinical study. Int J Dermatol 2017; 56: 850–855.
- Kowalska-Oledzka E, Slowinska M, Rakowska A, Czuwara J, Sicinska J, Olszewska M, et al. ‘Black dots’ seen under trichoscopy are not specific for alopecia areata. Clin Exp Dermatol 2012; 37: 615–619.
- Rudnicka L, Olszewska M, Rakowska A, Slowinska M. Trichoscopy update 2011. J Dermatol Case Rep 2011; 5: 82–88.
- Lima CDS, Lemes LR, Melo DF. Yellow dots in trichoscopy: relevance, clinical significance and peculiarities. An Bras Dermatol 2017; 92: 724–726.
- Peralta L, Morais P. Photoletter to the editor: The Friar Tuck sign in trichotillomania. J Dermatol Case Rep 2012; 6: 63–64.
- Ise M, Amagai M, Ohyama M. Follicular microhemorrhage: a unique dermoscopic sign for the detection of coexisting trichotillomania in alopecia areata. J Dermatol 2014; 41: 518–520.
- Brzezinski P, Cywinska E, Chiriac A. Report of a rare case of alopecia areata coexisting with trichotillomania. Int J Trichology 2016; 8: 32–34.
- Waskiel A, Rakowska A, Sikora M, Olszewska M, Rudnicka L. Trichoscopy of alopecia areata: An update. J Dermatol 2018; 45: 692–700.
- Rudnicka L, Olszewska M, Waskiel A, Rakowska A. Trichoscopy in hair shaft disorders. Dermatol Clin 2018; 36: 421–430.
- Grant JE, Dougherty DD, Chamberlain SR. Prevalence, gender correlates, and co-morbidity of trichotillomania. Psychiatr Res 2020; 288: 112948.
- Güleç AT. Trichoscopic features of eyebrow trichotillomania: it looks similar to scalp trichotillomania. Dermatol Pract Concept 2020; 10: e2020040.
- Adil M, Amin SS, Mohtashim M, Agrawal D. Concomitant trichotillomania, trichotemnomania and skin picking disorder in a woman. Ind J Dermatol Venereol Leprol 2020; 86: 286–289.
- Slawinska M, Opalska A, Mehrholz D, Sobjanek M, Nowicki R, Baranska-Rybak W. Videodermoscopy supports the diagnosis of eyelash trichotillomania. J Eur Acad Dermatol Venereol 2017; 31: e477–e478.
- Cutrone M, Grimalt R. The dermoscopic “pluck out sign” for beard trichotillomania. Skin Appendage Disord 2018; 4: 15–17.
- Malakar S, Mehta PR. “i hair”: A prognostic marker in alopecia areata & trichotillomania. Indian J Dermatol 2017; 62: 658–660.
- Pinto ACVD, de Brito FF, Cavalcante MLLL, de Andrade TCPC, da Silva GV, Martelli ACC. Trichotillomania: a case report with clinical and dermatoscopic differential diagnosis with alopecia areata. Anais Brasileiros de Dermatologia 2017; 92: 118–120.
- Miteva M, Tosti A. Dermoscopy guided scalp biopsy in cicatricial alopecia. J Eur Acad Dermatol Venereol 2013; 27: 1299–1303.