QUIZ SECTION
A Child with Hoarseness and Recurrent Cheek Erosions: A Quiz
Deyu SONG and Sheng WANG
Department of Dermatology, West China Hospital, Wuhou District, Sichuan University, Chengdu 610041, China. E-mail: wangsheng1892@126.com
Citation: Acta Derm Venereol 2024; 104: adv31737. DOI: https://doi.org/10.2340/actadv.v104.31737.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Feb 12, 2024
Competing interests and funding: The authors have no conflicts of interest to declare.
A 5-year-old boy exhibited delayed healing of erosions on his cheeks without the presence of blisters since the age of 2 years. Previously diagnosed with eczema, he remained unresponsive to multiple topical therapies. In addition, he had a history of hoarseness since birth.
On physical examination, scattered granulation tissue, atrophic scars, and crusts were observed on the face (Fig. 1A), along with subungual granulation tissues (Fig. 1B). No erosions or blisters were evident elsewhere on his body or within his mouth.
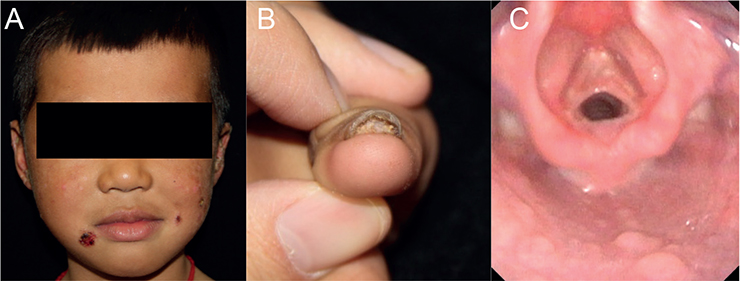
Fig. 1. Clinical features of the patient. (A) Scattered granulation tissue, atrophic scars, and crusts on the face. (B) Subungual granulation of fingernails. (C) Laryngoscopy showing bilateral vocal cord adhesion.
Video laryngoscopy demonstrated bilateral vocal cord adhesion (Fig. 1C). Bacterial and fungal cultures from the erosions demonstrated negative results. No anomalies were detected on abdominal and urinary ultrasonography, hearing test, and dental or ophthalmologic examination.
What is your diagnosis?
Differential diagnosis 1: Laryngo-onycho-cutaneous syndrome
Differential diagnosis 2: Hydroa vacciniforme
Differential diagnosis 3: Chronic mucocutaneous candidiasis
Differential diagnosis 4: Atopic dermatitis
See next page for answer.
ANSWERS TO QUIZ
A Child with Hoarseness and Recurrent Cheek Erosions: A Commentary
Diagnosis: Laryngo-onycho-cutaneous syndrome
Histopathological analysis indicated an abundance of granulation tissue and mixed inflammatory cell infiltration (Fig. 2). Further genetic study revealed a pathogenic homozygous missense mutation (c.171+1G>A) in the LAMA3 gene. Based on these findings, a diagnosis of laryngo-onycho-cutaneous (LOC) syndrome was made. After a 2-month treatment with 0.5% topical timolol, moderate improvement was observed in the facial lesions. Due to the absence of breathing obstruction symptoms and potential post-surgical granulation tissue formation, the patient’s parents declined a surgical procedure for releasing vocal cord adhesions.
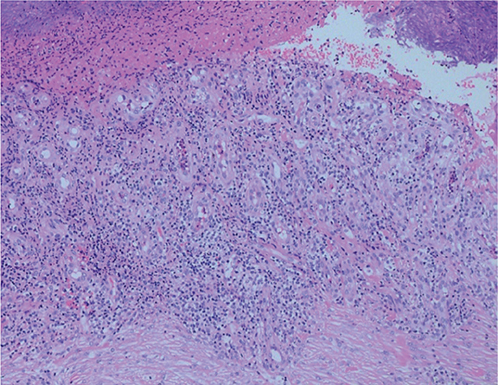
Fig. 2. Histological findings. Haematoxylin-eosin staining of the biopsy specimen taken from a skin lesion revealed epidermal necrosis, prominent vascular proliferation, and infiltration of abundant lymphocytes and neutrophils (original magnification ×100).
Laryngo-onycho-cutaneous syndrome (OMIM 245660) is a localized form of autosomal recessive junctional epidermolysis bullosa (EB) characterized by delayed wound-healing and mucosal granulation (1).
The prevalence of LOC is uncertain, but exceptionally rare, with less than 100 reported cases globally. However, potential underdiagnosis exists. Most typical cases of LOC are attributed to mutations in the LAMA3 gene, specifically within the N-terminal domain of LAMA3A, which encodes the laminin-a3a isoform (2). Loss of this N-terminal region is believed to contribute to the pronounced granulation tissue response in patients with LOC (2).
Unlike other EB types marked by widespread blistering, patients with LOC present with minimal blistering and prominent granulation tissue, often leading to misdiagnosis (3). Notably, slow-healing facial erosions constitute one of the hallmark features of LOC. Healed lesions frequently result in atrophic, pigmented scars, which may be mistaken for conditions such as eczema or hydroa vacciniforme. Granulation tissue can develop in the larynx, nail beds, and ocular surface, inducing early-onset hoarseness, recurrent nail loss and formation of symblepharon (2, 3). Recognition of these distinctive features may facilitate earlier identification of LOC. Although these findings can also been seen in other types of EB occasionally, genetic testing serves to confirm the diagnosis by identifying mutations in the N-terminal region of LAMA3A.
The management of LOC requires a comprehensive, multidisciplinary approach and long-term follow-up (3). Chronic erosions could be treated with topical steroids or topical timolol (4). However, disease severity varies, with prognosis contingent on the extent of mucosal involvement. The growth of granulation tissue in the larynx and adjacent structures can lead to airway obstruction and, in severe cases, premature mortality (2, 3). Consequently, repeated endoscopic investigations are recommended. Patients with severe larynx symptoms may require surgical intervention, such as tracheostomy. Due to the high frequency of ocular involvement, consultation with an ophthalmologist is also advisable. Genetic counselling is crucial for affected families to comprehend the risk of recurrence and make informed decisions regarding future pregnancies.
ACKNOWLEDGEMENT
This study was approved by the Ethics Committee Biomedical Research, West China Hospital of Sichuan University.
REFERENCES
- Barzegar M, Mozafari N, Kariminejad A, Asadikani Z, Ozoemena L, McGrath JA. A new homozygous nonsense mutation in LAMA3A underlying laryngo-onycho-cutaneous syndrome. Br J Dermatol 2013; 169: 1353–1356.
- McLean WH, Irvine AD, Hamill KJ, et al. An unusual N-terminal deletion of the laminin alpha3a isoform leads to the chronic granulation tissue disorder laryngo-onycho-cutaneous syndrome. Hum Mol Genet 2003; 12: 2395–2409.
- Bardhan A, Bruckner-Tuderman L, Chapple ILC, et al. Epidermolysis bullosa. Nat Rev Dis Primers 2020; 6: 78.
- Chiaverini C, Passeron T, Lacour JP. Topical timolol for chronic wounds in patients with junctional epidermolysis bullosa. J Am Acad Dermatol 2016; 75: e223–e224.