The COVID-19 pandemic has resulted in increased attention on infection prevention measures. This study aims to assess whether changes in hand hygiene procedures, use of personal protective equipment and moisturizers during the first year of the COVID-19 pandemic were associated with changes in the occurrence of skin symptoms among healthcare workers, cleaners, and day-care workers. A total of 602 participants (40%) responded to an electronic questionnaire, including questions on previous and current occupational exposure and skin problems. Increased frequency of hand washing, use of hand disinfectants, use of disposable gloves and moisturizers were all associated with an increased symptom score on the hands, wrists, forearms. Participants who increased their use of masks or respirators had a higher risk of facial skin symptoms, compared with those with non-increased occupational exposure. In conclusion, a change of behaviour among healthcare workers, cleaners and day-care workers during the first year of the COVID-19 pandemic, with an increase in occupational exposures and use of moisturizers, was associated with higher occurrence of facial skin symptoms and symptoms on the hands, wrists and forearms.
Key words: COVID-19; facial skin symptoms; hand eczema; health personnel; occupational exposure.
Accepted Nov 17, 2022; Published Jan 5, 2023
Acta Derm Venereol 2023; 103: adv00840.
DOI: 10.2340/actadv.v103.3420
Corr: Hilde Kristin Vindenes, Department of Occupational Medicine, Haukeland University Hospital, Bergen, Norway. E-mail: hilde.kristin.vindenes@helse-bergen.no
SIGNIFICANCE
This study shows that, during the first year of the COVID-19 pandemic, a change in behaviour with an increase in occupational exposure to hand wash, hand disinfectants and disposable gloves and use of moisturizers, was associated with increased symptoms on the hands, wrists and forearms among healthcare workers, cleaners and day-care workers. Furthermore, increased use of masks or respirators was associated with a higher risk of facial skin symptoms.
INTRODUCTION
Due to frequent exposure to wet work, irritants and allergens, healthcare workers (HCWs) have an increased risk of developing work-related skin disease. In a Norwegian population-based study from the HUNT3 survey (2006–2008), 28.5% of women with hand eczema (HE) worked in health and social work at the time of HE onset (1). Wet work is one of the strongest risk factors for HE and is defined as having wet hands for ≥ 2 h, washing hands ≥ 20 times or wearing occlusive gloves for ≥ 2 h per working day (2). However, studies have shown that even wet work ≤ 30 min may increase the risk of HE (3). Using lipid-soluble hand disinfectants and detergents may cause adverse skin reactions including skin dryness and irritant and allergic contact dermatitis (2, 4). In individuals with atopic dermatitis (AD), the skin barrier is already impaired; hence, such exposures may induce exacerbation of the underlying condition as well as an increased risk of developing contact dermatitis (5).
The COVID-19 pandemic focused attention on measures that are important to prevent the spread of infection. Intensified hand hygiene measures and the use of personal protective equipment (PPE) are among the actions that were implemented (6, 7).
Previous COVID-19 studies have emphasized that the intensified use of hand hygiene procedures has increased the risk of HE. The excessive use of tight-fitting PPE during the pandemic also seems to have increased the risk of occupational skin diseases, such as skin damage, exacerbation of pre-existing disease (e.g. acne and rosacea) as well as irritant and allergic contact dermatitis (8, 9). Some studies have also described an association between frequent hand hygiene procedures and HE among children in day-care centres and schools (10, 11).
The aim of the current study was to assess to what extent changes in hand hygiene procedures and the use of PPE and moisturizers among HCWs, cleaners, and day-care workers, from before to during the COVID-19 pandemic, were associated with changes in the occurrance of skin symptoms.
MATERIALS AND METHODS
Population and study design
In February 2021, approximately 1 year after the COVID-19 pandemic began, an electronic questionnaire was sent by e-mail to 1,059 HCWs, cleaners and day-care workers at Haukeland University Hospital in Bergen, Norway and to 447 HCWs employed in primary healthcare in the municipality of Bergen and 3 surrounding municipalities. The workers were selected as they were expected to have intensified their hand hygiene measures during the pandemic. Participants from the hospital included workers from the emergency room, COVID-19 wards, intermediate wards, infection wards, the intensive care unit, the COVID-19 test team, cleaning and personnel in the hospital’s day-care centres. Participants from the municipalities included HCWs from emergency primary healthcare centres, COVID-19 test teams and HCWs predominantly working in health centres (defined as “others”). The following occupations were included in the study: nurses and auxiliary nurses, physicians, cleaners, day-care workers, students, and administrators. All workers from the mentioned workplaces were invited to participate in the study.
The employees were sent 2 e-mails and 1 text message with reminders regarding participation. A total of 602 participants (40%) responded anonymously to the questionnaire, which contained 58 questions (Appendix S1). However, not all participants completed every question; thus the response rate varies for each question. The questionnaire included questions on previous and current skin problems, such as HE, facial skin symptoms, and symptoms on hands, wrists, and forearms. HE was defined based on the question; “have you ever had hand eczema”, and point prevalence was based on answering affirmative to the question; “I have hand eczema now”. HE within the last 12 months was based on the question “When did you last have eczema on your hands?” Symptoms on hands, wrists, and forearms included 12 symptom categories: “redness”, “dry skin with scaling/flacking”, “fissures or cracks”, “weeping or crusts”, “tiny water blister”, “papules”, “urticaria”, “itching”, “burning, prickling or stinging”, “tenderness”, “aching or pain” and “other”. AD was assessed by a self-reported history of childhood eczema (12). Furthermore, the questionnaire contained different questions such as questions on symptoms from the upper and lower airways, physical activity, body mass index (BMI), occupational hand hygiene procedures and use of PPE and moisturizers (exposure data) (Appendix S1). Different occupational exposures (hand wash, hand desinfectants, use of disposable gloves, use of masks or respirators (filtering masks) and use of moisturizers and the outcomes (the number of symptoms on hands, wrist and forearms and the presence of facial skin symptoms (yes/no)) were reported in the questionnaire, both for before and during the pandemic. The occupational exposure variables included hand washing (number of times per work day, categorized as 0–5, 6–10, 11–20, > 20 times), use of hand desinfectants (number of times per work day, categorized as 0–5, 6–10, 11–20, 21–50, > 50 times), use of disposable gloves at work (never/seldom, 1–2 days/week, almost daily, 1–10 times daily, > 10 times daily) and use of masks or respirators at work (never/seldom, 1–2 days/week, almost daily, 1–10 times daily, >10 times daily). Use of moisturizers before and during the pandemic was also reported (never, less than 1 day/week, 1–3 days/week, 4–7 days/week, > 1 time daily). The participants were informed about the possibility of being referred for an outpatient examination if they had experienced skin symptoms. The questions were derived from the validated Nordic occupational skin questionnaire (NOSQ) (13), from the RHINESSA study (www.rhinessa.net) and from a Swedish study on HCWs conducted during the COVID-19 pandemic (9). The questionnaire was prepared by the National Centre for Emergency Primary Health Care using software developed by Qualtrics (Qualtrics, Provo, UT, USA). The study is approved by the Regional Committee for Medical and Health Research Ethics (west) (REC 191415).
Statistical analysis
Symptom scores were based on questions associated with HE collected from NOSQ (13) and were calculated as the number of symptoms on the hands, wrists and forearms. The score was based on the 12 reported symptom categories, and all symptoms were weighted equally. A change in symptom score from before to during the pandemic was made by subtracting the score of symptoms during the pandemic from the score of symptoms before the pandemic.
Levels of the occupational exposure variables before and during the pandemic were each compared separately using marginal homogeneity tests. The marginal homogeneity test was also applied to evaluate the use of moisturizers before and during the pandemic. McNemar’s test was used to compare reported occurrences of each symptom on the hands, wrists, and forearms before and during the pandemic.
Possible associations between demographic variables (sex, age, AD, rhinitis, asthma, smoking habits, level of physical activity, BMI, weekly work hours, years of work in occupation, workplace, and daily work with patients with suspected or confirmed COVID-19 infection (yes/no)) and a change in the presence of facial skin symptoms were analysed with negative binomial generalized estimating equations (GEE) models. Similarly, a possible impact on the change in symptom score was analysed with linear GEE models. Possible effect modifications on outcomes from demographic variables or from change in use of masks or respirators were assessed by including an appropriate interaction term in the models.
When assessing associations between demographic variables and a change in level of occupational exposures, the exposures were dichotomized (increased or equal/reduced exposure) and analysed with negative binomial regression. Thus, the recoded exposure variables constituted the outcome part of the regression models. The possible impact of a change in occupational exposure on a change in symptom score on the hands, wrists and forearms was analysed with linear regression with difference in symptom score as the outcome. Estimates were also adjusted for possible confounding from sex, age, AD and weekly work hours. Direct acyclic graphs (DAGs) were used to identify variables to adjust for in the model. GEE models with robust estimation of standard errors were used to account for the correlation of individual measurements over time. Furthermore, the possible impact of a change in occupational exposures on a change in facial skin symptoms were analysed with negative binomial GEE models. All statistical analyses were performed with STATA SE17.0 (StataCorp LLC) and p-values less than 0.05 were considered statistically significant with no adjustment for multiple comparisons.
RESULTS
The majority of participants were female (79.4%) (Table I). The mean age was 39 years (data not shown). The mean number of working years in the given occupation was 12.1 years. A total of 262 participants (43.5%) worked with patients with suspected or confirmed COVID-19 infection (Table I). The most common occupation was nurse/auxiliary nurse (47.2%). The proportion of nurses/auxiliary nurses among female participants (50.0%) was higher than among male participants (36.3%) (data not shown). In total, 17.2% of the participants in the study reported a history of AD (Table I). The prevalence of AD was 44.1% among participants with self-reported HE during the last 12 months (data not shown).
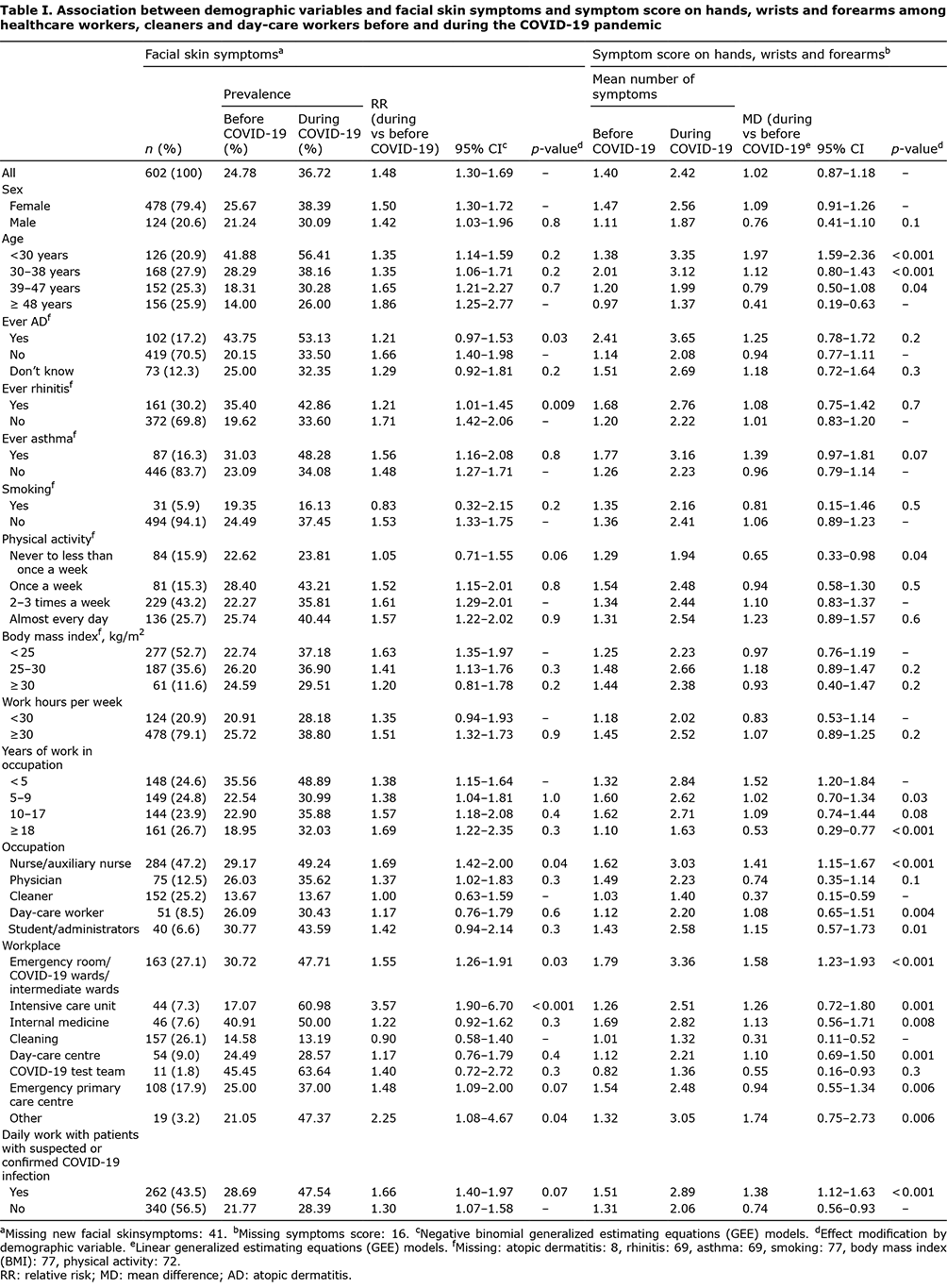
Hand eczema and symptoms on hands, wrists and forearms
In total, 20.1% of the participants reported HE during the preceding 12 months, while the point prevalence (current eczema) was 10.2% (data not shown). Among cleaners, 13.9% reported HE during the last 12 months, while the prevalence among day-care workers and HCWs were 11.8% and 23.7%, respectively.
The participants reported a significant change in hand washing, the use of hand desinfectants, disposable gloves, and masks or respirators (Fig. 1). An increase in hand washing frequency (> 20 times daily) from 14.1% to 23.2% was found. The percentage of participants using hand disinfectants > 50 times daily at work increased from 15.0% to 32.9%. For participants using disposable gloves > 10 times daily, there was a change from 27.5% to 60.7%. The percentage of participants using masks or respirators >10 times daily increased from 2.4% to 48.8%. The risk of increase in hand washing frequency, the use of hand disinfectants, use of disposable gloves and masks or respirators during the pandemic was significantly higher in the younger age groups compared with the oldest age group (Table SI). Nurses/auxiliary nurses, physicians, day-care workers and students/administrators had a significantly higher risk of increase in the use of hand disinfectants and use of disposable gloves (except gloves for day-care workers) compared with cleaners.

The proportion of subjects reporting use of moisturizers more than once daily increased from 23.7% to 44.3% from before to during the pandemic (Fig. 1), and with a significantly higher chance of increase for participants younger than 39 years compared with the oldest age group (Table SI).
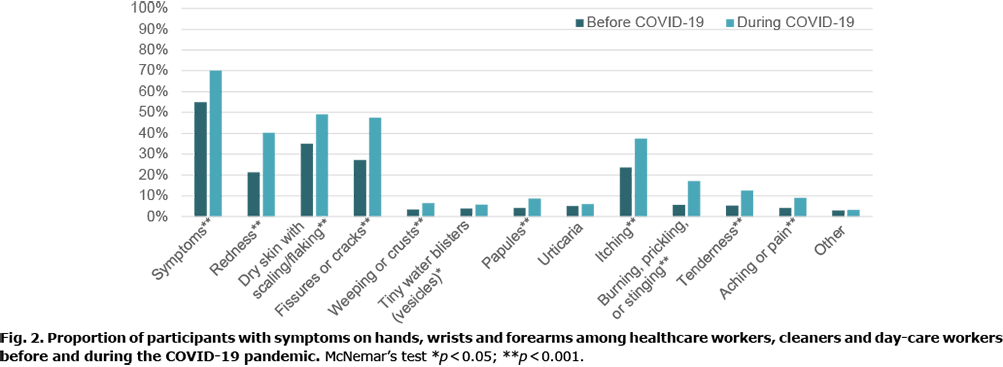
There was a significant increase in all symptoms on hands, wrists, and forearms from before to during the pandemic, except urticaria (Fig. 2). Redness, dry skin with scaling/flaking, fissures or cracks and itching increased the most. Among all the participants, 42.0% had an increase in symptom score from before to during the pandemic, 49.0% did not have any change, and 9.0% reported a reduced symptom score (data not shown). The mean number of symptoms increased from 1.4 to 2.4 from before to during the pandemic (Table I).
Young age was significantly associated with an increased symptom score on the hands, wrists, and forearms compared with the oldest age group. Those who had been working for 18 years or more were less likely to report a change in the symptom score on the hands, wrists and forearms.
The symptom score increased for all occupations. Nurses/auxiliary nurses, day-care workers and students/administrators had a significantly higher increased symptom score on the hands, wrists, and forearms compared with cleaners. A significant increase in symptom score was seen for all workplaces. Except for the COVID-19 test team, all workplaces had a significantly higher increase in symptom score compared with cleaning. HCWs who worked daily with patients with suspected or confirmed COVID-19 infection also had a significantly increased symptom score compared with HCWs not working with these patients.
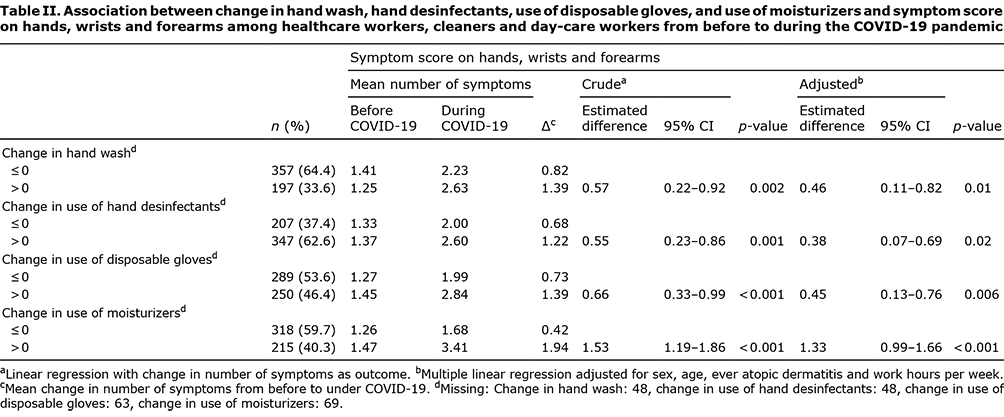
Increased frequency of hand washing, the use of hand disinfectants, use of disposable gloves and use of moisturizers during the pandemic were all significantly associated with an increased symptom score (both crude and adjusted) (Table II).
Facial skin symptoms
Prevalence of facial skin symptoms increased significantly from before (24.8%) to during (36.7%) the pandemic, with no significant sex difference (Table I). Participants working in the emergency room/COVID-19 wards/intermediate wards, intensive care unit and “other” had a significantly higher risk of facial skin symptoms compared with cleaners. Furthermore, the risk of facial skin symptoms was significantly higher for nurses and auxiliary nurses compared with cleaners. The risk of facial skin symptoms during the pandemic increased relatively more in the group without the atopy markers, AD and rhinitis, compared with atopic participants.
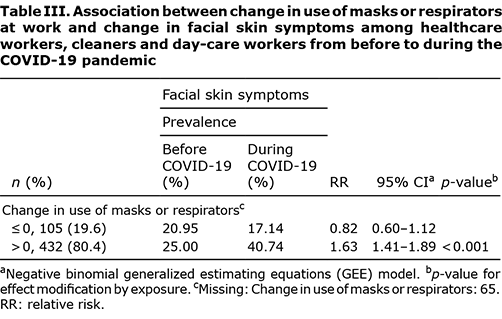
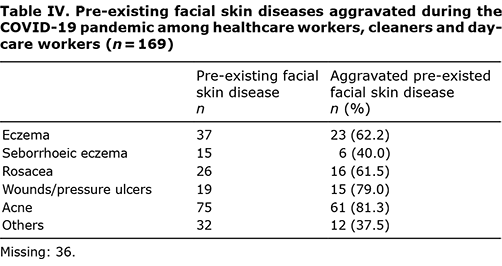
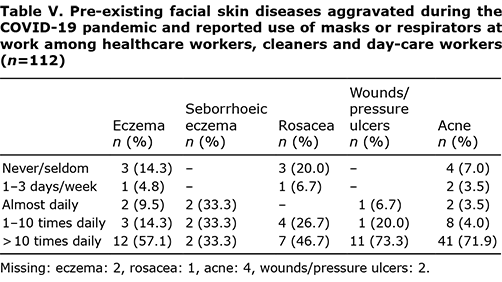
Those who had increased their frequency of use of masks or respirators had a significantly higher risk of more facial skin symptoms (Table III). For participants with facial skin disease before COVID-19, 72.5% reported aggravation of the disease during the first year of the pandemic (data not shown). Acne was the most frequently reported pre-existing facial skin disease being aggravated (81.3%), followed by wounds/pressure ulcers (79.0%), eczema (62.2%) and rosacea (61.5%) (Table IV). The majority of those with aggravated eczema, wounds/pressure ulcers and acne reported use of masks or respirators more than 10 times daily at work (Table V).
DISCUSSION
Increased frequency of hand hygiene procedures and the use of PPE at work were observed during the first year of the COVID-19 pandemic. During the same period, the occurrence of skin symptoms on the hands, wrists, and forearms, as well as facial skin symptoms increased.
Previous studies have reported that the major determinants for the development of irritant contact dermatitis are duration and frequency of wet work (2). We propose that the increase in hand and facial skin symptoms within the first year of the COVID-19 pandemic is caused by intensified infection prevention. Previous COVID-19 studies have reported on the prevalence of hand and facial skin symptoms during the pandemic; however, the current study also provides self-reported change in occupational exposure and changes in symptoms during this time.
In the current study, 20.1% of the participants (comprising HCWs, cleaners and day-care workers) reported HE during the pandemic. Traditionally, cleaners and HCWs have high exposure to wet work and the prevalence of HE is high relative to other occupations (1, 14). However, the literature regarding HE among day-care workers is scarce. In the current study, 13.8% of cleaners reported HE during the pandemic, while the prevalence among day-care workers was 11.8%.
Several studies have reported skin symptoms among HCWs during the pandemic, and considerable differences are reported in the occurrence of HE. Swedish HCWs had a 1-year prevalence of 29% during the pandemic (9) compared with 21% in 2014 (15). A lower prevalence of HE among HCWs during the pandemic was reported from Denmark (14.7%) (16). Furthermore, a Danish cohort study reported a decrease in the 1-year prevalence of HE during the pandemic, from 16.0% to 13.0% (17). Some studies on HCWs working with COVID-19 patients report a considerably higher prevalence of HE (50.5%) (18) and skin damage on hands (70.4%) (8). In a study by Guertler et al. (19) self-reported HE and symptoms on the hands among HCWs were examined. The prevalence of HE was 14.0%, while the prevalence of symptoms associated with acute hand dermatitis was substantially higher (90.4%). The study participants reported dryness, erythema and itching to be the most common symptoms. In the current study, redness, dry skin with scaling/flaking, fissure or cracks, and itching were the symptoms that increased the most during the pandemic. The difference in prevalence may be due to differences in infection rates/workload between countries, difference in groups of employment included or the use of different definitions of HE.
The majority of the participants in the current study were female, similar to previous studies among HCWs (3, 9, 20). In the current study, the prevalence of facial skin symptoms and symptoms on the hands, wrists and forearms increased more for women than for men, but did not reach statistical significance. Women are known to have a higher risk of HE than men. A sex difference has been explained by varying environmental exposures and not by a genuine difference in skin susceptibility. Women are more often represented in occupations involving wet work and traditionally have a higher total load of additional exposures at home, such as taking care of children and cleaning (2, 21).
In the current study, a history of AD was reported by 44.1% of the participants with HE during the pandemic. Ruff et al. reported that patients with AD had a 3–4-fold increased prevalence of HE compared with controls (22). In a Norwegian population-based study, 31% of the participants with HE reported having had AD (1). Interestingly, the reported increase in the symptom score on the hands, wrists and forearms in the present study did not seem to be affected by atopy, but may instead be explained by increased exposure.
An increase in hand hygiene measures was associated with an increase in symptom score. In the current study, the proportion of participants reporting hand wash frequency more than 20 times per day increased from 14.1% to 23.2%; furthermore, the reported use of hand disinfectants more than 50 times a day increased from 15.0% to 32.9%. Guidelines have been changed during the last decades, recommending HCWs to replace hand washing with hand desinfectants, using alcohol gel rubs when possible (4). This could explain why the observed difference in hand washing frequency is not larger, as the largest increase in hand hygiene procedures are seen for use of hand disinfectants.
The pandemic has resulted in increased attention on hand hygiene procedures and use of PPE. Change in all occupational exposures was significantly higher among the younger age groups and participants who had been employed for a shorter time in the occupation. This is in line with a Swedish study, reporting that water exposure at work decreases with increasing age (23). One of the suggested explanations was that senior workers were employed on more administrative assignments.
In the current study the symptom score on the hands, wrists, and forearms increased regardless of workplace or occupation, which is in line with findings by Guertler et al. (19). Due to the pandemic, hand hygiene measures have been implemented among all HCWs, independent of COVID-19 related work. The current study illustrates that this effect is seen for other groups, as day-care workers also report a significant increase in use of hand disinfectants and moisturizers. To our knowledge, no previous studies on occupational exposure among cleaners and day-care workers during the COVID-19 pandemic have been published.
The application of moisturizers is assumed to offer a protective effect against irritant exposure (24). Among the respondents in the current study, 24% used moisturizers more than once daily before the pandemic, compared with 44% during the pandemic. Erdem et al. (18) reported that the use of moisturizing cream in daily life was associated with a higher risk of HE and symptoms of HE. In the current study, young and female participants showed the largest increase in moisturizer use. Furthermore, the largest increase in use was observed for the participants with the highest increase in symptoms. This may illustrate that participants used moisturizer with a therapeutic intent after the development of symptoms of HE, as also reported by Visser (25), but may also signal a prophylactic strategy.
Since the start of the COVID-19 pandemic, several studies have reported on facial skin disease related to the use of masks or respirators (8, 9, 26, 27). The current study shows a significant increase in reported facial skin symptoms during the pandemic, compared with before. For participants with facial skin disease before the pandemic, 72.5% reported aggravation of the disease during the pandemic. Acne was the most common pre-existing disease reported to be aggravated. Participants with AD and rhinitis reported a higher prevalence of facial symptoms during the pandemic than non-atopic participants; however, the risk of increased symptoms was higher among non-atopic participants. Atopic participants had a higher occurrence of initial facial symptoms, and are more likely to perform more frequent skin care compared with non-atopics, as suggested by Niesert et al. (27).
More frequent use of masks or respirators significantly increased the risk of facial skin symptoms during the pandemic. Furthermore, our results suggests a dose- dependent association between use of masks or respirators and exacerbations of facial skin diseases, which is in line with other studies (9, 27).
Strengths and limitations
A strength of the current study is the detailed data on self-reported occupational exposure before and during the pandemic. However, as this is a cross-sectional study the prevalence and exposures before the pandemic are retrospectively self-reported and one might speculate whether these are overestimated, thus representing a recall bias. To limit the total number of questions, no questions regarding leisure exposure were included in the questionnaire. Non-occupational exposures contribute to the total daily exposure and, as the authorities recommended intensified hand hygiene procedures during the pandemic, an increase in non-occupational exposure cannot be ruled out.
Most questions were derived from the NOSQ; however, some alterations to questions were necessary to emphasize changes due to the pandemic and these questions have not been validated. However, these questions have been used in prior studies, such as the RHINESSA study and the Swedish study among HCWs during the COVID-19 pandemic (9). Lund et al. (28) showed that workers in professions with a high prevalence of wet work exposure overestimated the duration of wet work, and underestimated the frequency of hand washing. Further, for hand desinfectants they were least likely to overestimate frequency. Regarding wet work exposure, the current study used the validated questionnaire based on frequency and not on duration, thus one cannot rule out the possibility of underestimation.
This study was not able to compare responders from non-responders as there was no background information (e.g. sex, age, occupation) concerning non-responders. Inclusion of respondents with skin symptoms may cause a selection bias, which might lead to an overestimation of the prevalence of skin symptoms. In questionnaire studies, 2 methods have been used to diagnose HE; self-reported HE or diagnosis based on various symptoms. Svensson et al. (29) defined the minimum criteria of HE diagnosed by the dermatologist to be erythema and papules/vesicles or erythema and scaling and fissures/lichenification. HE diagnosis based on combinations of reported skin symptoms had a lower sensitivity and specificity compared with HE diagnosis by the dermatologist, while the question “Do you have hand eczema?” had higher sensitivity and specificity.
Self-reported HE has been shown to underestimate the true prevalence of HE. Meding et al. (30) found that false-positive answers were usually caused by confusion with other skin diseases and the false-negative answers were obtained from individuals with mild HE in most cases. The current study aimed to investigate the change in symptoms. In line with Vissler et al. a score based on symptoms from the NOSQ was used in order not to miss an early state of HE/mild HE (25). Although it may be difficult for the lay individual to identify symptoms of HE, the current study population is mainly represented by HCWs, who are thought to have a higher ability to identify skin symptoms. Like Hamnerius et al. (9), we used diagnosis-based rather than symptom-based questions on exacerbations of pre-existing facial skin diseases, as the majority of the participants had some level of medical education, and thus would be expected to know the terms for common facial skin diseases.
Conclusion
This study shows that a change in behaviour among HCWs, cleaners and day-care workers during the first year of the COVID-19 pandemic, with an increase in occupational exposure (hand washing, hand disinfectants, disposable gloves and masks or respirators) and use of moisturizers was associated with increased symptoms on hands, wrists and forearms and a higher risk of facial skin symptoms compared with before the pandemic.
ACKNOWLEDGEMENTS
The authors would like to thank all the participants and institutions that participated in this study and everyone who contributed to the development of the project, especially Merete Allertsen, Liv Heiberg Okkenhaug, Trude Duelien Skorge, Ingrid Hjulstad Johansen and Sue Stannard.
This project was funded by the Western Norwegian Regional Health Authorities (grant number 912128) and by funding through the Alrek Health Cluster.
The authors have no conflicts of interest to declare.
REFERENCES
- Vindenes HK, Svanes C, Lygre SHL, Hollund BE, Langhammer A, Bertelsen RJ. Prevalence of, and work-related risk factors for, hand eczema in a Norwegian general population (The HUNT Study). Contact Dermatitis 2017; 77: 214–223.
- Behroozy A, Keegel TG. Wet-work exposure: a main risk factor for occupational hand dermatitis. Saf Health Work 2014; 5: 175–180.
- Lund T, Petersen SB, Flachs EM, Ebbehoj NE, Bonde JP, Agner T. Risk of work-related hand eczema in relation to wet work exposure. Scand J Work Environ Health 2020; 46: 437–445.
- World Health Organization (WHO) Guidelines Approved by the Guidelines Review Committee. WHO guidelines on hand hygiene in health care: first global patient safety challenge clean care is safer care. Geneva: World Health Organization; 2009.
- Visser MJ, Landeck L, Campbell LE, McLean WHI, Weidinger S, Calkoen F, et al. Impact of atopic dermatitis and loss-of-function mutations in the filaggrin gene on the development of occupational irritant contact dermatitis. Br J Dermatol 2013; 168: 326–332.
- World Health Organization, United Nations Children’s Fund. Water, sanitation, hygiene, and waste management for the COVID-19 virus: interim guidance, 19 March 2020. Geneva: World Health Organization, 2020.
- World Health O. Mask use in the context of COVID-19: interim guidance, 1 December 2020. Geneva: World Health Organization, 2020.
- Lan J, Song Z, Miao X, Li H, Li Y, Dong L, et al. Skin damage among healthcare workers managing coronavirus disease-2019. J Am Acad Dermatol 2020; 82: 1215–1216.
- Hamnerius N, Pontén A, Bergendorff O, Bruze M, Björk J, Svedman C. Skin exposures, hand eczema and facial skin disease in healthcare workers during the COVID-19 pandemic: a cross-sectional study. Acta Derm Venereol 2021; 101: adv00543.
- Simonsen AB, Ruge IF, Quaade AS, Johansen JD, Thyssen JP, Zachariae C. High incidence of hand eczema in Danish schoolchildren following intensive hand hygiene during the COVID-19 pandemic: a nationwide questionnaire study. Br J Dermatol 2020; 183: 975–976.
- Simonsen AB, Ruge IF, Quaade AS, Johansen JD, Thyssen JP, Zachariae C. Increased occurrence of hand eczema in young children following the Danish hand hygiene recommendations during the COVID-19 pandemic. Contact Dermatitis 2021; 84: 144–152.
- Stenberg B, Lindberg M, Meding B, Svensson A. Is the question ‘Have you had childhood eczema?’ useful for assessing childhood atopic eczema in adult population surveys? Contact Dermatitis 2006; 54: 334–337.
- Susitaival P, Flyvholm MA, Meding B, Kanerva L, Lindberg M, Svensson A, et al. Nordic Occupational Skin Questionnaire (NOSQ-2002): a new tool for surveying occupational skin diseases and exposure. Contact Dermatitis 2003; 49: 70–76.
- Lund T, Flachs EM, Sørensen JA, Ebbehøj NE, Bonde JP, Agner T. A job-exposure matrix addressing hand exposure to wet work. Int Arch Occup Environ Health 2019; 92: 959–966.
- Hamnerius N, Svedman C, Bergendorff O, Bjork J, Bruze M, Engfeldt M, et al. Hand eczema and occupational contact allergies in healthcare workers with a focus on rubber additives. Contact Dermatitis 2018; 79: 149–156.
- Yüksel YT, Ebbehøj NE, Agner T. An update on the prevalence and risk exposures associated with hand eczema in Danish hospital employees: a cross-sectional questionnaire-based study. Contact Dermatitis 2022; 86: 89–97.
- Yüksel YT, Nørreslet LB, Flachs EM, Ebbehøj NE, Agner T. Hand eczema, wet work exposure, and quality of life in health care workers in Denmark during the COVID-19 pandemic. JAAD Int 2022; 7: 86–94.
- Erdem Y, Altunay IK, Aksu Çerman A, Inal S, Ugurer E, Sivaz O, et al. The risk of hand eczema in healthcare workers during the COVID-19 pandemic: do we need specific attention or prevention strategies? Contact Dermatitis 2020; 83: 422–423.
- Guertler A, Moellhoff N, Schenck TL, Hagen CS, Kendziora B, Giunta RE, et al. Onset of occupational hand eczema among healthcare workers during the SARS-CoV-2 pandemic: comparing a single surgical site with a COVID-19 intensive care unit. Contact Dermatitis 2020; 83: 108–114.
- Hamnerius N, Svedman C, Bergendorff O, Bjork J, Bruze M, Ponten A. Wet work exposure and hand eczema among healthcare workers: a cross-sectional study. Br J Dermatol 2018; 178: 452–461.
- Mollerup A, Veien NK, Johansen JD. An analysis of gender differences in patients with hand eczema – everyday exposures, severity, and consequences. Contact Dermatitis 2014; 71: 21–30.
- Ruff SMD, Engebretsen KA, Zachariae C, Johansen JD, Silverberg JI, Egeberg A, et al. The association between atopic dermatitis and hand eczema: a systematic review and meta-analysis. Br J Dermatol 2018; 178: 879–888.
- Meding B, Lindahl G, Alderling M, Wrangsjo K, Anveden Berglind I. Is skin exposure to water mainly occupational or nonoccupational? A population-based study. Br J Dermatol 2013; 168: 1281–1286.
- Williams C, Wilkinson SM, McShane P, Lewis J, Pennington D, Pierce S, et al. A double-blind, randomized study to assess the effectiveness of different moisturizers in preventing dermatitis induced by hand washing to simulate healthcare use. Br J Dermatol 2010; 162: 1088–1092.
- Visser MJ, Verberk MM, van Dijk FJ, Bakker JG, Bos JD, Kezic S. Wet work and hand eczema in apprentice nurses; part I of a prospective cohort study. Contact Dermatitis 2014; 70: 44–55.
- Ho WYB, Tan LYC, Zhao X, Wang D, Lim JH. Epidemiology of occupational dermatoses associated with personal protective equipment use in the COVID-19 pandemic: risk factors and mitigation strategies for frontline healthcare workers. JAAD Int 2022; 8: 34–44.
- Niesert AC, Oppel EM, Nellessen T, Frey S, Clanner-Engelshofen BM, Wollenberg A, et al. “Face mask dermatitis” due to compulsory facial masks during the SARS-CoV-2 pandemic: data from 550 health care and non-health care workers in Germany. Eur J Dermatol 2021; 31: 199–204.
- Lund T, Flachs EM, Ebbehøj NE, Bonde JP, Agner T. Wet work exposure: comparison of observed and self-reported data. Int Arch Occup Environ Health 2019; 92: 317–326.
- Svensson A, Lindberg M, Meding B, Sundberg K, Stenberg B. Self-reported hand eczema: symptom-based reports do not increase the validity of diagnosis. Br J Dermatol 2002; 147: 281–284.
- Meding B, Barregård L. Validity of self-reports of hand eczema. Contact Dermatitis 2001; 45: 99–103.