QUIZ SECTION
Not Always a Malignant Tumour: A Quiz
Bárbara VIEIRA GRANJA1, Pedro AMOROSO CANÃO2 and Alberto MOTA1,3,4
1Department of Dermatology and Venereology, Centro Hospitalar Universitário de São João, Alameda Prof. Hernâni Monteiro, 4200–319 Porto, Portugal, 2Department of Pathology, Centro Hospitalar Universitário de São João, 3Department of Medicine, and 4RISE@CINTESIS, Faculty of Medicine, University of Porto, Porto, Portugal. E-mail: brlvg96@gmail.com
Citation: Acta Derm Venereol 2024; 104: adv34750. DOI: https://doi.org/10.2340/actadv.v104.34750.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Feb 9, 2024
A 34-year-old man with unremarkable medical history was admitted to the dermatology department due to an asymptomatic oral lesion that had evolved over a period of 8 week. Physical examination revealed a centrally ulcerated nodular lesion in the right lip commissure (Fig. 1a), with no other findings. Histological examination revealed a moderate lymphocytic infiltrate in the dermis with frequent plasma cells (Fig. 1b). No microorganisms were identified on Warthin–Starry stain. The lesion had spontaneous remission within 3 weeks. Twelve weeks later the patient returned due to asymptomatic white labial mucosal plaques (Fig. 1c), histopathological examination of which demonstrated a dense interstitial and perivascular plasma cell infiltrate in the lamina propria.
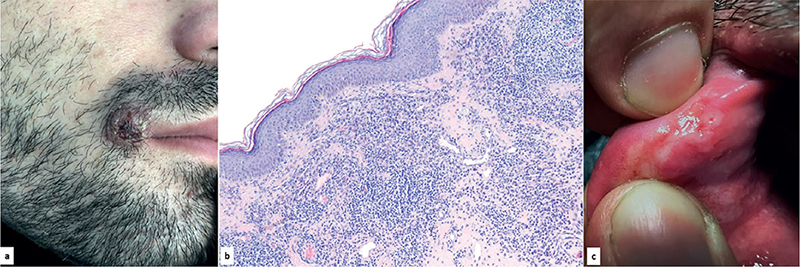
Fig. 1. a) Centrally ulcerated nodular lesion, asymptomatic, with firm and well-defined borders measuring 2 cm in the right lip commissure, with no other findings. (b) Interstitial lymphocytic infiltrate with plasma cells in the dermis (haematoxylin and eosin (HE), 100×). (c) Asymptomatic white plaques on the labial mucosal. Written permission is given by the patient to publish these photographs.
What is your diagnosis?
Differential diagnosis 1: Syphilis
Differential diagnosis 2: Keratoacanthoma
Differential diagnosis 3: Basal cell carcinoma
Differential diagnosis 4: Skin adnexal tumour
See next page for answer.
ANSWERS TO QUIZ
Not Always a Malignant Tumour: A Commentary
Diagnosis: Syphilis
Syphilis is a sexually-transmitted infectious disease caused by the anaerobic filamentous spirochete Treponema pallidum (1). Transmission is mainly through direct contact with syphilitic lesions, most often during vaginal, anal, or oral sex (1, 2).
Patients with undiagnosed syphilis may present with only oral lesions (2). Approximately 4–12% of patients with primary syphilis present with oral chancres, commonly on the lip, tongue, buccal mucosa, palate, gingiva or tonsillar pillar (2). Chancres remit spontaneously in 3–8 weeks (1). In secondary syphilis, oral manifestations are variable and the most well-recognized lesions are multiple mucous patches that are slightly raised and covered by greyish-white pseudomembranes and surrounded by erythema (1).
In line with its nickname of “The Great Imitator”, oral manifestations of syphilis may mimic a variety of infectious, neoplastic or immune-mediated processes (2, 3). In a recent case series, 92.5% of cases were diagnosed in the secondary stage and only 7.5% within the primary stage (4). The histopathological appearance may also lead to a plethora of diagnoses (2). Although no single microscopic feature is specific, the diagnosis should be considered towards an unusual epithelial hyperplasia, granulomatous or plasmacytic predominant chronic inflammation (5). The infiltrate characteristically surrounds blood vessels and nerves (2).
The first clinical presentation of this patient with a solitary ulcerated nodule of the lip commissure (Fig. 1a), which mimicked a neoplastic lesion. Even though he denied unprotected sexual contacts, the clinical and histopathological findings were suggestive of syphilis, and serological screening with a Venereal Disease Research Laboratory (VDRL) test showed a reactive title (1:32). PCR tests for Treponema pallidum were positive, both in skin biopsy specimens from the right labial commissure lesion and in mucosal plaques. After administration of a single dose of penicillin G benzathine (2.4 million units intramuscularly) there was complete remission of the lesions.
In conclusion, the large spectrum of possible appearances of oral manifestations of syphilis can create a diagnostic challenge to the clinician and pathologist, leading to delay in diagnosis or misdiagnosis. Therefore, early recognition is imperative for prompt diagnosis, treatment and prevention of disease transmission.
REFERENCES
- Ficarra G, Carlos R. Syphilis: the renaissance of an old disease with oral implications. Head Neck Pathol 2009; 3: 195–206.
- Smith MH, Vargo RJ, Bilodeau EA, Anderson KM, Trzcinska A, Canterbury CR, et al. Oral manifestations of syphilis: a review of the clinical and histopathologic characteristics of a reemerging entity with report of 19 new cases. Head Neck Pathol 2021; 15: 787–795.
- Leuci S, Martina S, Adamo D, Ruoppo E, Santarelli A, Sorrentino R, et al. Oral syphilis: a retrospective analysis of 12 cases and a review of the literature. Oral Dis 2013; 19: 738–746.
- Schuch LF, da Silva KD, de Arruda JAA, Etges A, Gomes APN, Mesquita RA, et al. Forty cases of acquired oral syphilis and a review of the literature. Int J Oral Maxillofac Surg 2019; 48: 635–643.
- Barrett AW, Villarroel Dorrego M, Hodgson TA, Porter SR, Hopper C, Argiriadou AS, et al. The histopathology of syphilis of the oral mucosa. J Oral Pathol Med 2004; 33: 286–291.