QUIZ SECTION
An Indolent Forearm Plaque: A Quiz
Claire SOURSOU1, Maxime BATTISTELLA2, Edouard BEGON1 and Clémence MAUPPIN1
1Department of Dermatology, René Dubos Hospital, 6 avenue de l’Ile de France, Pontoise, and 2Department of Pathology, Saint Louis Hospital, APHP, Paris, France. E-mail: claire.soursou@aphp.fr
Citation: Acta Derm Venereol 2024; 104: adv34883. DOI https://doi.org/10.2340/actadv.v104.34883.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Apr 3, 2024
An 88-year-old Caucasian man presented to the dermatology department for evaluation of an erythematous scaly plaque on the right forearm. He had a past medical history of arterial hypertension and heart failure. The patient reported that the lesion had developed 30 years previously and had been stable and asymptomatic since then. The plaque had been treated with various topical treatments without improvement.
Physical examination revealed an erythematous scaly plaque on the right forearm and hand, atrophic in some places, with a well-defined border. There were no enlarged lymph nodes and no other lesions on the rest of the skin (Fig. 1).

Fig. 1. Physical examination revealed an erythematous scaly plaque on the right forearm and hand, atrophic in some places, with a well-defined border.
What is your diagnosis?
Differential diagnosis 1: Pagetoid reticulosis
Differential diagnosis 2: Discoid lupus erythematosus
Differential diagnosis 3: Psoriasis
Differential diagnosis 4: Dermatophytosis
See next page for answer.
ANSWERS TO QUIZ
An Indolent Forearm Plaque: A Commentary
Diagnosis: Pagetoid reticulosis
Skin biopsy revealed the presence of an atypical, small-to-medium sized strongly epidermotropic atypical lymphoid population, with some keratinocyte necrosis and hyperkeratotic changes on the surface. Atypical lymphocytes also showed focal folliculotropism. The dermis was the site of a moderately abundant perivascular lymphoid infiltrate with no atypia (Fig. 2). The immunohistochemical profile of the epidermotropic cells was CD2+, CD5+, weak CD8+, CD4–, CD3–, CD7–, PD1–, perforin–, CD56–, granzyme B–, TCRdelta–, CD30–. A search for a cutaneous T clone was unsuccessful.
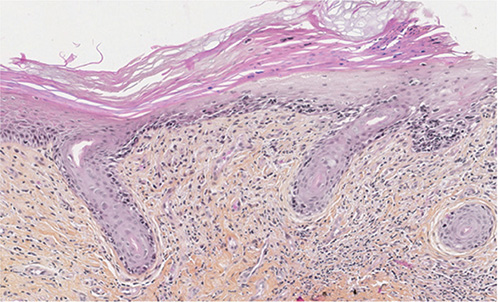
Fig. 2. Skin biopsy revealed the presence of an atypical, small to medium sized epidermotropic lymphocytic population, keratinocyte necrosis and hyperkeratotic changes on the surface.
Based on these findings, we diagnosed pagetoid reticulosis. The patient was initially treated with 1 application of clobetasol propionate 0.05% cream daily for 1 month, then gradually tapered off over 2 months. After 1 month of treatment, the skin lesion had improved, becoming less scaly and less erosive (Fig. 3). The patient was also offered radiotherapy. He declined it because of the good response to topical corticosteroids and because he was debilitated by several hospitalizations for cardiac decompensation.

Fig. 3. Under topical corticosteroids, the skin lesion improved, becoming less scaly and less erosive.
Pagetoid reticulosis, also known as Woringer–Kolopp disease, is a rare form of cutaneous T-cell lymphoma that presents as a single, slow-growing, hyperkeratotic or scaly plaque usually on the extremities (1). It is classified by the European Organisation for Research and Treatment of Cancer System as a variant of mycosis fungoides (2). No gender predilection has been demonstrated. The indolent course of the disease and its rarity make it difficult to diagnose. Clinical differential diagnoses include psoriasis, dermatophytosis, eczematous dermatitis, and Bowen’s disease. Histological examination reveals an epidermis infiltrated by atypical T lymphocytes demonstrating striking epidermotropism (3). The term pagetoid reticulosis was introduced by Braun-Falco et al. (4) in 1973 because of the similarity of the epidermotropic atypical lymphocytes to the intraepidermal adenocarcinomatous cells found in Paget’s disease of the breast. Other epidermal changes include spongiosis, acanthosis, and hyperkeratosis. The dermis contains an inflammatory infiltrate of mature lymphocytes, histiocytes, and plasma cells.
While the clinical and histopathological results are relatively constant, the immunophenotypic profile is more heterogeneous: T cells are most often CD4–/CD8+, but cases with CD4+/CD8–, CD4–/CD8–, or CD4+/CD8+ phenotype have also been documented. The disease is inconsistently CD30+ (1). No additional imaging or testing is recommended, as no cases of distant or lymph node metastasis have been described in the localized form of pagetoid reticulosis (1). Radiotherapy or wide excision should be considered initially, as the cure rate is excellent and the recurrence rate is very low (1, 5). Combined therapies and other modalities such as topical corticosteroids (1), photodynamic therapy (6), local chemotherapy (topical alkylating agents, interferon alpha-2b (7), imiquimod (8)), or alitretinoin (9) may be used. In a systematic review that included 143 patients, 92 patients had complete remission after treatment (most of them with radiotherapy, surgery, or topical corticosteroids) and 11 cases recurred with a median time to recurrence of 38.5 months. Annual follow-up is recommended (1). In fact, the majority of patients with pagetoid reticulosis have an excellent prognosis (1).
REFERENCES
- Osto M, Afify O, Musa A, Ahmed U, Rehman R, Mehregan D. Woringer–Kolopp disease (localized pagetoid reticulosis): a systematic review. Int J Dermatol 2023; 62: 312–321.
- Willemze R, Cerroni L, Kempf W, Berti E, Facchetti F, Swerdlow SH, et al. The 2018 update of the WHO-EORTC classification for primary cutaneous lymphomas. Blood 2019; 133: 1703–1714.
- Haghighi B, Smoller BR, LeBoit PE, Warnke RA, Sander CA, Kohler S. Pagetoid reticulosis (Woringer–Kolopp disease): an immunophenotypic, molecular, and clinicopathologic study. Mod Pathol 2000; 13: 502–510.
- Braun-Falco O, Marghescu S, Wolff HH. Pagetoide retikulose (Morbus Woringer–Kolopp). Hautarzt 1973; 24: 11–21.
- Latzka J, Assaf C, Bagot M, Cozzio A, Dummer R, Guenova E, et al. EORTC consensus recommendations for the treatment of mycosis fungoides/Sézary syndrome – Update 2023. Eur J Cancer 2023; 195: 113343.
- Mendes GW, Beckford A, Krejci N, Mahalingam M, Goldberg L, Gilchrest BA. Pagetoid reticulosis in a prepubescent boy successfully treated with photodynamic therapy. Clin Exp Dermatol 2012; 37: 759–761.
- Wang T, Liu YH, Zheng HY. Localized pagetoid reticulosis (Woringer–Kolopp disease): complete response to NB-UVB combined with IFN. Dermatol Ther 2014; 27: 227–229.
- Su O, Dizman D, Onsun N, Bahali AG, Biyik Ozkaya D, Tosuner Z, et al. Treatment of localized pagetoid reticulosis with imiquimod: a case report and review of the literature. J Eur Acad Dermatol Venereol 2016; 30: 324–326.
- Schmitz L, Bierhoff E, Dirschka T. Alitretinoin: eine effektive Therapie option der pagetoiden Retikulose. J German Soc Dermatol 2013; 11: 1194–119.