ORIGINAL REPORT
Referral Pathways for Children with Atopic Diseases in Denmark
Gitte FÆRK1–3, Malin Glindvad AHLSTRÖM3, Viktoria Helt-Eggers LURA1, Susanne REVENTLOW2, Jeanne Duus JOHANSEN3, Jacob P. THYSSEN5, Kirsten Skamstrup HANSEN1,4 and Lone SKOV1,6
1Department of Dermatology and Allergy, Copenhagen University Hospital – Herlev and Gentofte, 2The Research Unit for General Practice and Section of General Practice, Department of Public Health, University of Copenhagen, Copenhagen, 3National Allergy Research Center, Copenhagen University Hospital – Herlev and Gentofte, 4Department of Pediatrics, Copenhagen University Hospital – Herlev and Gentofte, 5Department of Dermatology and Venereology, Copenhagen University Hospital – Bispebjerg, and 6Department of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark
Atopic diseases such as atopic dermatitis, food allergy, allergic rhinoconjunctivitis, and/or asthma are common. In Denmark, however, there are multiple referral pathways for these diseases in the healthcare system and they are poorly understood. To describe how children with atopic diseases navigate their way through the Danish healthcare system, a questionnaire was distributed to children aged ≤ 17 years, who were being treated for atopic diseases between August 2020 and June 2021, either by a practising specialist or a hospital department, in the Capital Region of Denmark. A total of 279 children completed the questionnaire and most were referred to a specialist or to a hospital by their general practitioner. No “common track” to hospital existed for patients with ≥ 3 atopic diseases. These patients were more often referred to a hospital compared with children with 2 atopic diseases or fewer (odds ratio [OR] 3.79; 95% CI 2.07–7.24). The primary determinants for hospital treatment were food allergy (OR 4.69; 95% CI 2.07–10.61) and asthma (OR 2.58; 95% CI 1.18–5.63). In conclusion, children with multiple atopic diseases were more likely to be referred to hospital departments than to practising specialists, mainly due to food allergies.
SIGNIFICANCE
Atopic dermatitis, hay fever, food allergies, and asthma are common diseases, but little is known about how children with 1 or more of these diseases navigate through the healthcare system in Denmark. In this questionnaire study that included 279 children with atopic diseases, we mapped their pathway through the Danish healthcare system. Children with 3 or more atopic diseases were more likely to be referred to hospitals than to practising specialists. Food allergies and, to a lesser extent, asthma were the main reasons for referral.
Key words: allergic rhinitis; asthma; atopic dermatitis; disease management; food hypersensitivity; referral.
Citation: Acta Derm Venereol 2024; 104: adv34961. DOI https://doi.org/10.2340/actadv.v104.34961.
Copyright: 2014 © The Author(s). Published by MJS Publishing, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/).
Submitted: Dec 15, 2023; Accepted: Apr 18, 2024; Published: Jun 3, 2024
Corr: Gitte Færk, Center for Almen Medicin, Øster Farimagsgade 5, Opgang Q, stuen, DK-1353 København K, Denmark. E-mail: gitte.faerk@sund.ku.dk
Competing interests and funding: The authors GF, MA, VL, SR, and KH declared no potential conflicts of interest concerning the research, authorship, and publication of this article. LS has received research funding from Novartis, Bristol-Myers Squibb, AbbVie, Janssen Pharmaceuticals, Sanofi, Almirall, the LEO Foundation and the Kgl Hofbundtmager Aage Bang Foundation, and honoraria as consultant and/or speaker from AbbVie, Almirall, Leo Pharma, Pfizer, Eli Lilly, Novartis, Sanofi, UCB, Bristol-Myers Squibb, Boehringer Ingelheim, and Janssen Pharmaceuticals. JT is an adviser for AbbVie, Almirall, Arena Pharmaceuticals, Coloplast, OM Pharma, Aslan Pharmaceuticals, Union Therapeutics, Eli Lilly & Co, LEO Pharma, Pfizer, Regeneron, and Sanofi-Genzyme, a speaker for AbbVie, Almirall, Eli Lilly & Co, LEO Pharma, Pfizer, Regeneron, and Sanofi-Genzyme, and has received research grants from Pfizer, Regeneron, and Sanofi-Genzyme.
The project was funded by (in alphabetical order): CAG (Clinical Academic Group), Fonden for faglig udvikling i speciallægepraksis, Lilly og Herbert Hansens Fond, Region Hovedstadens forskningsfond, and Tværspuljen. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
INTRODUCTION
Atopic diseases such as atopic dermatitis (AD), food allergy, asthma, and allergic rhinoconjunctivitis (ARC) are common diseases among children worldwide (1–3). Whereas AD and food allergy often develop during the first year of life (4), asthma and ARC usually occur later in childhood, with disease severities differing – from mild and transient, to severe and potentially fatal. The mechanisms underlying the development of 1 or several atopic diseases and the associated severity are poorly understood. Seven and 8 different disease trajectories for AD, asthma, and ARC have recently been described (5, 6). Early differentiation of patients with high vs low risk of persistent and severe atopic diseases is desirable to prevent disease progression and to offer the most appropriate level of care.
The Danish healthcare system is tax-supported and this ensures that all citizens have equal, cost-free access to healthcare services, including general practice, practising specialists, and hospital treatment (7). Some citizens may also have private health insurance cover and may be treated in private care, thus avoiding waiting lists. This option, however, may exclude some children, depending on their age and disease manifestations, as there is no private care for children with severe or complex atopic diseases.
In Denmark, children with atopic diseases are usually seen and treated initially in general practice, but may then be referred to practising specialists or hospital departments, e.g. paediatrics, dermatology, otorhinolaryngology, and allergology depending on the severity and complexity of their disease (8). According to paediatric specialty standards, children with complex or severe atopic diseases should be referred to a hospital department with a high level of specialization. To date, however, no disease management programme exists for patients with multiple atopic diseases, and the referral pathways in the Danish healthcare system are poorly understood (8). The management of these patients requires different levels of knowledge and support, depending on the number and severity of atopic diseases, family resources, and needs (9).
From 2006 to 2015, the number of patients with atopic diseases treated in a hospital setting in Denmark increased by 177% (8). A UK national survey reported that the number of paediatric allergy appointments for newly referred patients has increased sevenfold from 2006 to handle rising demand (10). A South Korean study also found increased prevalence of ARC and asthma in hospital settings, but not AD (11). To ensure optimal quality of care and effective use of healthcare services for individuals with atopic diseases, an efficient referral pathway to the appropriate level of care is warranted.
The aim of the present study was to describe the current referral pathways in the Danish healthcare system for children with AD, food allergy, ARC, and/or asthma.
MATERIALS AND METHODS
The study included children and adolescents (0–17 years) who had consulted a hospital department (paediatric, dermatology, or allergy) or a practising specialist (2 paediatricians, 1 dermatologist, and 1 otorhinolaryngologist) in the Capital Region of Denmark between August 2020 and June 2021. Patients diagnosed with AD, food allergy, ARC, and/or asthma by a physician from 1 of the hospital departments or practising specialists were invited to answer a questionnaire.
For patients aged < 15 years, one parent/caregiver answered the questionnaire; while patients aged 15 to 17 years were encouraged to answer the questionnaire together with their parent/caregiver.
The Ethics Committee of the Capital Region of Denmark (H-19041695) and the Data Protection Agency (P-2020-659) approved the study.
The questionnaire covered baseline characteristics, referral pathways, and details of the 4 atopic diseases including symptoms and severity. In the analysis, parent/patient-reported diseases confirmed by a physician were used. Answers were multiple choice and/or blank space for comments.
All data were manually entered into REDCap (Research Electronic Data Capture; https://www.project-redcap.org/) by two investigators (GF and VL) (12, 13).
Statistical analysis
A χ2 test was used to compare groups, but when expected values were below 5, Fisher’s exact test was used instead. Normal distribution was assessed for the data. For non-parametric values (e.g. Visual Analog Scale [VAS] scores for severity), a Mann–Whitney U test was applied. We used logistic regression to calculate the odds ratio (OR) of being referred to a hospital, with AD, food allergy, asthma, and ARC as the independent variables.
P-values were considered as statistically significant if they were below 0.05. A 95% confidence interval was used for ORs.
Data management and statistical analyses were performed using R version 4.2.0 (R Core Team, 2022; R Foundation for Statistical Computing, Vienna, Austria), and SAS® Enterprise Guide®, version 7.15 (SAS Institute, Cary, NC, USA).
RESULTS
In total, 301 children and adolescents were included in the study and the completed questionnaire was returned by 279 (completion rate: 92.7%). In the subsequent analysis, only patients who completed the questionnaires were included. Of the 279 patients, 166 came from hospital departments and 113 from practising specialists. Patient characteristics are listed in Table I. Overall, median age was 10 years (CI 9–10). Approximately 80% of all patients had a family history of atopic diseases, mainly ARC (more than 60%). The socioeconomic differences (parent education, household income, parents living together) between patients from different inclusion sites were minor (Table SI).
Patients from the Department of Dermatology and the practising dermatologist differed slightly from the rest. They were younger compared with patients from other specialties (median 4 years [Department of Dermatology] and 0 years [practising dermatologist] vs ≥ 10 years [other specialties]). Dermatologic patients more commonly had a first-degree relative with AD compared with patients from other specialties (57% vs ≤ 32%) (see Table SI). Among patients with AD, there was no significant difference in the self-reported severity of AD within the last 6 months between those treated by practising specialists and those treated at hospital departments (p = 0.12). However, a significantly higher proportion of patients from hospital departments had required urgent visits to a physician within the previous 12 months due to AD (Table II).
| Factor | Practising specialist % (n/N of total) | Hospital % (n/N of total) | p-valuesb |
| Distribution of diseasesa | |||
| AD | 32% (36/111) | 56% (92/163) | 9 x 10–5 |
| Food allergy | 21% (23/111) | 52% (85/164) | 2 x 10–7 |
| ARC | 69% (77/111) | 62% (99/159) | 0.23 |
| Asthma | 37% (40/109) | 51% (84/165) | 0.02 |
| Number of diseases | |||
| 1 disease | 42% (45/107) | 24% (38/157) | 0.002 |
| 2 diseases | 35% (37/107) | 29% (46/157) | 0.36 |
| 3 diseases | 13% (14/107) | 27% (42/157) | 0.008 |
| 4 diseases | 2% (2/107) | 15% (24/157) | 0.0003 |
| Severity last 6 months, VAS 0–100 (0 is no symptoms and 100 is severe symptoms), mean (SD) | |||
| AD | 36 (31) | 44 (28) | 0.12 |
| Food allergy | 44 (30) | 41 (33) | 0.65 |
| ARC | 41 (26) | 43 (25) | 0.64 |
| Asthma | 29 (22) | 27 (24) | 0.38 |
| Any days missed from day care and school in the previous 12 months due to the diseases, yes | 26% (29/112) | 39% (65/165) | 0.02 |
| 1 to 2 days | 9% (10/112) | 12% (20/165) | 0.40 |
| < 1 week | 10% (11/112) | 17% (28/165) | 0.09 |
| 1 week–1 month | 4% (5/112) | 6% (10/165) | 0.76 |
| > 1 month | 1% (1/112) | 3% (5/165) | 0.41 |
| Unknown | 2% (2/112) | 1% (2/165) | 1 |
| Urgent visits to a physician in the previous 12 months due to the diseases, yes | 13% (15/113) | 29% (48/166) | 0.002 |
| AD | 3% (3/113) | 10% (17/166) | 0.02 |
| Food allergy | 2% (2/113) | 8% (13/166) | 0.03 |
| ARC | 3% (3/113) | 2% (4/166) | 1 |
| Asthma | 4% (5/113) | 9% (15/166) | 0.14 |
| Other allergic symptoms | 2% (2/113) | 2% (4/166) | 1 |
| Affecting the family in general, scale 0–100 (0 is not affected and 100 is very affected), mean (SD) | 27 (25) | 34 (32) | 0.33 |
| aParent/patient-reported physician-based diseases. bP-values were obtained using the χ2 test, Fisher’s exact test, Welch, and Student’s t-test. | |||
| Data are summarized as percentage (number of total) or mean (SD). | |||
| AD: atopic dermatitis; ARC: allergic rhinoconjunctivitis; n: number; SD: standard deviation; VAS: visual analogue scale. Significant p-values (p ≤ 0.05) are shown in bold. | |||
Hospital vs practising specialists
The children were divided into 2 groups depending on their site of inclusion: hospital department or a practising specialist. Hospital patients more often had AD (p = 9 x 10–5), food allergy (p = 2 x 10–7) and/or asthma (p = 0.02) than patients from practising specialists; no differences were found in the number of patients with ARC (see Table II). Hospital patients were more likely to have 3 (27% vs 13%, p = 0.008) or all 4 of the atopic diseases (15% vs 2%, p = 0.0003) compared with patients from practising specialists, who often had only 1 of the diseases (42% vs 24%, p = 0.002).
There was no difference in the self-reported severity of the atopic diseases, how they affected the families’ daily lives, and their quality of life (see Table II). However, 39% of patients from hospital departments had missed days from day care compared with 26% from practising specialists (p = 0.02), although no differences were found in the number of days missed. Besides planned visits to their physician, patients from hospital departments were more likely to require urgent visits (29% vs 13%, p = 0.002), because their AD flared up (10% vs 3%, p = 0.02) or their food allergy worsened (8% vs 2%, p = 0.03).
Referral pathways
Generally, about 80% of patients had previously consulted their GP regarding atopic disease and around 75% had either seen a practising specialist in the past or were seeing one at the time of study inclusion. Patients were divided into 2 groups depending on their number of atopic diseases: 164 had 1 or 2 diseases, and 81 had 3 or 4 diseases. In the group with ≥ 3 diseases, 80% received treatment at a hospital department, compared with 51% in the group with ≤ 2 diseases (OR 3.87, CI 2.07–7.24) (Table III). Patients from both groups followed the general referral pattern from their GP to a practising specialist or to a hospital department. No “common track” directly from general practitioner to hospital existed for patients with ≥ 3 atopic diseases (Table III) (Fig. 1). More than half of all patients had visited their GP only once or twice before their referral to a practising specialist or hospital department, and this typically occurred within 6 months of their first visit. Five percent of patients with 1 or 2 diseases, and 12% of patients with 3 or 4 diseases had consulted a private hospital or a private specialist, covered by either family resources or a private health insurance company.
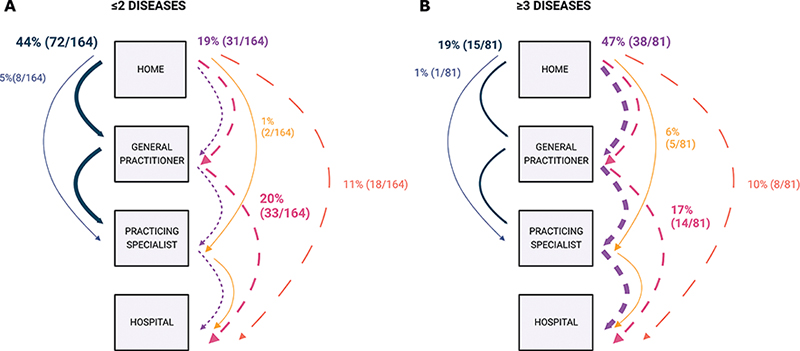
Fig. 1. Referral pathways for children 0 to 17 years with atopic dermatitis, food allergy, allergic rhinoconjunctivitis, and/or asthma stratified by number of diseases. (A) Children with ≤ 2 atopic diseases and (B) children with ≥ 3 atopic diseases. Each arrow shows the referral pathway for a group of patients. The width of the arrow illustrates the proportion of patients in each group, also shown as percentage and numbers in parentheses. On the left side in each figure are referral pathways ending at a practising specialist and on the right side referral pathways ending at a hospital. The figure was created with BioRender.com.
Even though patients with more than 3 atopic diseases were referred to hospital, further analysis showed that food allergy (OR 4.69, 2.07–10.61) was the primary determinant for the referral. Asthma (OR 2.58, 1.18–5.63) also played a role, but AD (OR 2.31, 0.97–5.52), ARC (OR 0.54, 0.25–1.17), or the fact of having ≥ 3 atopic diseases (OR 1.17, 0.34–4.04) had no influence.
DISCUSSION
This study provides new insight into the referral pathways in Denmark for children with atopic diseases. Children with 1 or 2 atopic disease(s) were often treated by practising specialists, while those with 3 or more atopic diseases were almost 4 times more likely to be referred to a hospital department. Subsequent analysis showed that food allergy and, to a lesser extent, asthma were the primary determinants for referral to a hospital department, rather than the number of diseases. We found no common track to hospital for patients with ≥ 3 diseases, and the general referral pattern was from the GP to a practising specialist and to a hospital department.
Previous referral pathway studies have been register-based in the main and often dealing with a single atopic disease (7, 14, 15). According to a study that included 2 atopic diseases, children with both AD and asthma visited hospital emergency departments and outpatient clinics more frequently than those with asthma alone (16). This is in line with our findings: that children with multiple atopic diseases were more frequently referred to a hospital department and a higher percentage needed urgent care. However, a corresponding study showed that adults with both AD and asthma, compared with adults with only 1 of these diseases, more frequently consulted their GP or a practising specialist rather than hospital departments (outpatient clinics) (17), indicating that the referral pathways for atopic diseases change from childhood to adulthood. Interestingly, when ARC was included in the study, adults with both AD and asthma more often had ARC consultations in a hospital than adults with only 1 of the diseases (17). This result supports our finding concerning multiple atopic diseases and hospital referrals.
We found that food allergy was a main determinant for referral to a hospital department and it might suggest that children with food allergy are primarily receiving medical investigation at hospital departments. This is consistent with Danish national guidelines that hospital-based allergy centres perform the diagnostic tests such as oral food challenges, and provide care for patients with food allergy and anaphylactic reactions (8). Both international and national recommendations from other countries are consistent with these guidelines (18, 19).
Another, albeit less significant, determinant that affected hospital referral was asthma. Previous research has emphasized the importance of receiving specialized care for severe asthma (20, 21), partly due to access to a greater variety of asthma treatments including biological treatment (21, 22).
We did not find a common track to hospital for children with multiple atopic diseases and many had seen both their GP and a practising specialist before a hospital referral. This may be due to the time-varying onset of the diseases (5, 6), as only 1 or 2 diseases had evolved at the time point for referral from their GP. However, there is ongoing work to categorize atopic diseases into various subtypes based on genetic factors and clinical characteristics (23, 24). One study showed that persistent AD might be predicted by a child’s prior usage of especially potent AD medication (25). If these findings could be used to accurately predict how the diseases will develop, they could help to determine where patients should be referred to get the best care at the right time.
Disease management programmes include stratification of patients, adopting a patient-centred approach and ensuring coherence in healthcare services (26). Clinical practice guidelines are part of these disease management programmes, yet a study revealed that within the scope of applied clinical practice standards in General Practice, fragmented healthcare was a concern for patients with multiple diseases (27). Further, it was difficult to integrate these patients’ individual needs and preferences into the stratification, which, in any case, is not always accurate as the most vulnerable patients with fewer resources are often dismissed rapidly in the secondary and tertiary healthcare sectors because of, e.g., missed appointments or low adherence to treatment (27). The limited options to personalize guidelines are the main reasons for non-adherence, according to the Allergic Rhinitis and Its Impact on Asthma (ARIA) collaboration (28); but a personalized, integrated patient care approach has been suggested as a solution (28, 29).
Strengths and limitations
We included patients from practising specialists as well as from hospitals. To reduce selection and non-response bias, all eligible patients at, e.g., a hospital department on a given day were invited to participate, and they were encouraged to fill out the questionnaire while they were at the department. The completion rate in our study was 92.7%.
A potential limitation is recall bias, for example in the questions concerning previous experiences of referral pathways in the healthcare system. The patients in this study were children and adolescents, which meant that the onset of their disease(s) and referral pathways were within recent years, thus reducing the risk of recall bias. The primary and secondary healthcare sectors in Denmark use different electronic medical record systems that do not automatically share information. This made it difficult to confirm patients’ responses concerning their referral pathways and we therefore had to rely on parent/patient-reported data.
Family history of atopic diseases was reported in the questionnaire, but we did not have data on family members’ encounters with the healthcare system. Prior experience may influence expectations regarding referral to and navigation of the healthcare system.
Severity of the diseases was not clinically assessed, since we did not have validated patient/parent-reported measurements for all 4 diseases. We therefore chose to use VAS to assess severity, both for the specific day that patients completed the questionnaire, and for the previous 6 months, to ensure comparability and consistency across all 4 diseases. Furthermore, ARIA guidelines for ARC recommend the use of VAS to assess severity (28).
Conclusion
This study shows that children with multiple atopic diseases were more likely to be referred to hospital departments than to practising specialists, specifically for food allergies. Further research in the form of qualitative, in-depth interviews with the parents of children with atopic diseases could obtain more insight into their needs, experiences, and preferences.
ACKNOWLEDGEMENTS
IRB approval status: Approved by the Ethics Committee of the Capital Region of Denmark (H-19041695).
REFERENCES
- Pawankar R, Canonica GW, Holgate ST, Lockey RF, Blaiss MS. Chapter 2 The burden of allergic diseases. In: World Allergy Organization (WAO) White Book on Allergy. Update 2013: 2013: p. 27–72.
- Henriksen L, Simonsen J, Haerskjold A, Linder M, Kieler H, Thomsen SF, et al. Incidence rates of atopic dermatitis, asthma, and allergic rhinoconjunctivitis in Danish and Swedish children. J Allergy Clin Immunol 2015; 136: 360–366.e362.
- Asher MI, Montefort S, Bjorksten B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet 2006; 368: 733–743.
- Weidinger S, Novak N. Atopic dermatitis. Lancet 2016; 387: 1109–1122.
- Belgrave DC, Granell R, Simpson A, Guiver J, Bishop C, Buchan I, et al. Developmental profiles of eczema, wheeze, and rhinitis: two population-based birth cohort studies. PLoS Med 2014; 11: e1001748.
- Kilanowski A, Thiering E, Wang G, Kumar A, Kress S, Flexeder C, et al. Allergic disease trajectories up to adolescence: characteristics, early-life, and genetic determinants. Allergy 2023; 78: 836–850.
- Egeberg A, Thyssen JP, Wu JJ, Pierce E, Terres JAR. Treatment patterns in Danish patients with atopic dermatitis before and after hospital referral. Dermatol Ther (Heidelb) 2021; 11: 499–512.
- Sundhedsstyrelsen [Danish National Health Authority]. Status på allergi-området. Rapportering til Sundheds- og Ældreministeriet [Overview of the allergy area. Reporting to the Health and Senior Citizen Ministry]; 2017: p. 1-92.
- Vestergaard C, Thyssen JP, Barbarot S, Paul C, Ring J, Wollenberg A. Quality of care in atopic dermatitis: a position statement by the European Task Force on Atopic Dermatitis (ETFAD). J Eur Acad Dermatol Venereol 2020; 34: e136–e138.
- Wells R, McKay C, Makwana N, Vyas D, Vaughan S, Christopher A, et al. National survey of United Kingdom paediatric allergy services. Clin Exp Allergy 2022; 52: 1276–1290.
- Yoo B, Park Y, Park K, Kim H. A 9-year trend in the prevalence of allergic disease based on national health insurance data. J Prev Med Public Health 2015; 48: 301–309.
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019; 95: 103208.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377–381.
- von Kobyletzki L, Ballardini N, Henrohn D, Neary MP, Ortsater G, Geale K, et al. Care pathways in atopic dermatitis: a retrospective population-based cohort study. J Eur Acad Dermatol Venereol 2022; 36: 1456–1466.
- Johansson EK, Brenneche A, Trangbaek D, Stelmaszuk MN, Freilich J, Anderson CD. Treatment patterns among patients with atopic dermatitis in secondary care: a national, observational, non-interventional, retrospective study in Sweden. Acta Derm Venereol 2022; 102: adv00774.
- Ali Z, Ulrik CS, Egeberg A, Thyssen JP, Thomsen SF. Association of childhood atopic dermatitis with a higher risk of health care utilization and drug use for asthma: a nationwide cohort study. Dermatitis 2022; 33: 257–263.
- Ali Z, Egeberg A, Thyssen JP, Ulrik CS, Thomsen SF. Adults with concomitant atopic dermatitis and asthma have more frequent urgent healthcare utilization and less frequent scheduled follow-up visits than adults with atopic dermatitis or asthma only: a nationwide cohort study. J Eur Acad Dermatol Venereol 2022; 36: 2406–2413.
- Berni Canani R, Caffarelli C, Calvani M, Martelli A, Carucci L, Cozzolino T, et al. Diagnostic therapeutic care pathway for pediatric food allergies and intolerances in Italy: a joint position paper by the Italian Society for Pediatric Gastroenterology Hepatology and Nutrition (SIGENP) and the Italian Society for Pediatric Allergy and Immunology (SIAIP). Ital J Pediatr 2022; 48: 87.
- Muraro A, Werfel T, Hoffmann-Sommergruber K, Roberts G, Beyer K, Bindslev-Jensen C, et al. EAACI food allergy and anaphylaxis guidelines: diagnosis and management of food allergy. Allergy 2014; 69: 1008–1025.
- Denton E, Lee J, Tay T, Radhakrishna N, Hore-Lacy F, Mackay A, et al. Systematic assessment for difficult and severe asthma improves outcomes and halves oral corticosteroid burden independent of monoclonal biologic use. J Allergy Clin Immunol Pract 2020; 8: 1616–1624.
- Hansen S, von Bulow A, Sandin P, Ernstsson O, Janson C, Lehtimaki L, et al. Prevalence and management of severe asthma in the Nordic countries: findings from the NORDSTAR cohort. ERJ Open Res 2023; 9: 00687–2022.
- Agache I, Beltran J, Akdis C, Akdis M, Canelo-Aybar C, Canonica GW, et al. Efficacy and safety of treatment with biologicals (benralizumab, dupilumab, mepolizumab, omalizumab and reslizumab) for severe eosinophilic asthma. A systematic review for the EAACI Guidelines: recommendations on the use of biologicals in severe asthma. Allergy 2020; 75: 1023–1042.
- Paternoster L, Savenije OEM, Heron J, Evans DM, Vonk JM, Brunekreef B, et al. Identification of atopic dermatitis subgroups in children from 2 longitudinal birth cohorts. J Allergy Clin Immunol 2018; 141: 964–971.
- Conrad LA, Cabana MD, Rastogi D. Defining pediatric asthma: phenotypes to endotypes and beyond. Pediatr Res 2021; 90: 45–51.
- Thyssen JP, Corn G, Wohlfahrt J, Melbye M, Bager P. Retrospective markers of paediatric atopic dermatitis persistence after hospital diagnosis: a nationwide cohort study. Clin Exp Allergy 2019; 49: 1455–1463.
- Sundhedsstyrelsen [Danish National Health Authority]. 3 Indhold i forløbsprogrammer [3 Content in Disease Management Programs]. In: Forløbsprogrammer for kronisk sygdom - den generiske model [Disease Management Programs for chronic disease - the generic model]; 2012: p. 9–23.
- Kristensen MAT, Due TD, Holge-Hazelton B, Guassora AD, Waldorff FB. ‘More constricting than inspiring’: GPs find chronic care programmes of limited clinical utility. A qualitative study. BJGP Open 2018; 2: bjgpopen18X101591.
- Bousquet J, Schunemann HJ, Togias A, Bachert C, Erhola M, Hellings PW, et al. Next-generation Allergic Rhinitis and Its Impact on Asthma (ARIA) guidelines for allergic rhinitis based on Grading of Recommendations Assessment, Development and Evaluation (GRADE) and real-world evidence. J Allergy Clin Immunol 2020; 145: 70–80 e73.
- Maleki-Yazdi K, Zhao I, Chu D. Values and preferences of patients and caregivers regarding treatment of atopic dermatitis: a systematic review. Ann Allerg Asthma Im 2022; 129: S74–S75.