QUIZ SECTION
Annular Pigmented Macules on the Upper Trunk: A Quiz
Federica D’AGOSTINO1,2, Giulia GASPARINI1,2, Silvia Francesca RIVA1,2, Antonio GUADAGNO1,2 and Aurora PARODI1,2
1Department of Health Sciences (DISSAL), Section of Dermatology, University of Genoa, Via Pastore 1, IT-16132 Genoa, Italy, 2Department of Dermatology, Ospedale Policlinico San Martino IRCCS, Genoa, Italy. E-mail: drfedericadagostino@gmail.com
Citation: Acta Derm Venereol 2024; 104: adv35278. DOI https://doi.org/10.2340/actadv.v104.35278.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Mar 12, 2024
A 76-year-old Caucasian woman presented at the dermatology clinic with itchy pigmented skin lesions on the upper dorsal region, which had been present for the past year. Her significant medical comorbidities include hypertension and dyslipidaemia treated with olmesartan, nebivolol, atorvastatin and ezetimibe. She had a history of breast cancer successfully treated with surgery and radiotherapy 5 years prior.
Physical examination revealed chronic sun-damaged skin and multiple, brown annular macules, 5 mm in size, with a well-demarcated hyperchromic border and central sparing over the upper back area.
On dermoscopy, the lesions exhibited a hyperchromic border with grey dots limited on the periphery and central clearing (Fig. 1).
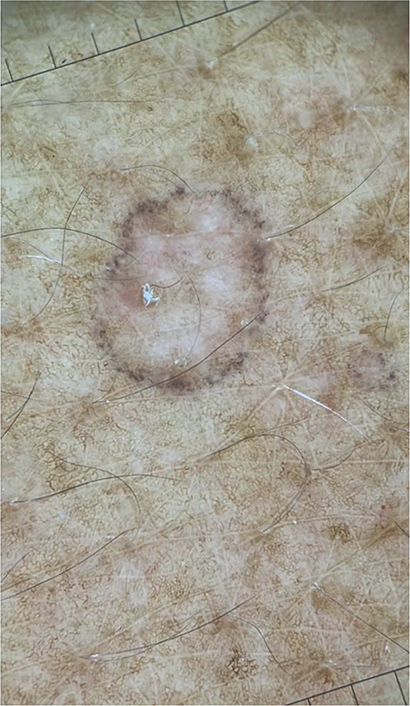
Fig. 1. Dermoscopy. The lesions on the upper back area exhibited a hyperchromic border with grey dots limited on the periphery and central clearing. Original magnification × 10.
A skin biopsy from a dorsal lesion was performed. Histopathology showed a cornoid lamella composed of thin column of parakeratotic cells, agranulosis and vacuolated cells in the spinous layer of the epidermis, and a slight perivascular chronic inflammatory infiltrate, scattered melanophages, mild solar elastosis in the papillary dermis (Fig. 2).
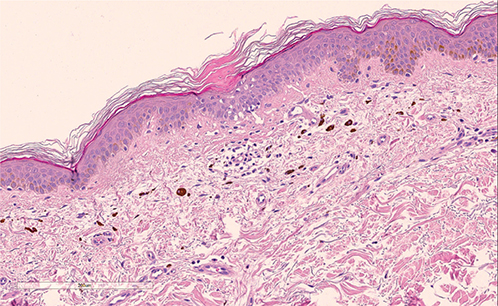
Fig. 2. Histopathology: haematoxylin and eosin; original magnification 40×. The epidermis shows a cornoid lamella composed of thin column of parakeratotic cells, agranulosis and vacuolated cells in the spinous layer. Within the papillary dermis, a slight perivascular chronic inflammatory infiltrate is seen. Scattered melanophages are present.
What is your diagnosis?
Differential diagnosis 1: Pigmented disseminated superficial actinic porokeratosis
Differential diagnosis 2: Lichenoid keratosis
Differential diagnosis 3: Lichen planus pigmentosus
Differential diagnosis 4: Lichenoid drug reaction
See next page for answer.
ANSWERS TO QUIZ
Annular Pigmented Macules on the Upper Trunk: A Commentary
Diagnosis: Pigmented disseminated superficial actinic porokeratosis
Porokeratosis is a benign neoplastic disorder of keratinization characterized by a clonal proliferation of epidermal keratinocytes. The pathway that leads to the abnormal proliferation of keratinocytes is unknown. A variety of causal factors have been proposed, including genetic susceptibility, ultraviolet radiation, viral infections and immunosuppression (1, 2).
Multiple clinical variants of porokeratosis have been described.
Disseminated superficial actinic porokeratosis (DSAP) is the most common type of porokeratosis. DSAP typically occurs in the third or fourth decade of life, with an estimated female to male ratio of 1.8:1 (3). Patients frequently report a history of chronic sun exposure, supporting the role of ultraviolet radiation as one of the main aetiopathogenetic factors.
In recent years, a rare distinct variant of DSAP has been described, which is represented by pigmented disseminated superficial actinic porokeratosis (4–6).
DSAP is clinically characterized by skin-coloured, annular atrophic macules/plaques, 5–10 mm in size, surrounded by a peripheral hyperkeratotic ridge-like border. The distribution of lesions usually involves sun-exposed sites, such as the extensor surfaces of the arms, legs, back and shoulders, with sparing of the palms and soles, whereas facial lesions occur in approximately 15% of patients (4, 5).
Dermoscopic examination of DSAP reveals a peripheral annular keratin rim with double edge “train tracks”, an atrophic scar-like central area and no obvious melanocytic features (1).
While the pigmented variant of DSAP the “train tracks” border shows with multiple fine grey-black dots (4, 5)
Histopathology of DSAP shows the presence of cornoid lamellae consistent with hyperkeratotic and parakeratotic columns associated with underlying loss of granular layer, in the epidermis, and solar elastosis, melanocyte hyperplasia, pigment incontinence within the superficial dermis below the cornoid lamellae.
Notably, the unusual finding, which support the diagnosis of a pigmented DSAP, as in the current case, was the presence of prominent melanocyte hyperplasia and pigment incontinence (4–6).
Differential diagnosis of DSAP includes other hyperplastic and neoplastic lesions, such as solar lentigo, actinic keratoses, lichenoid keratoses, melanoma, and inflammatory skin disorders such as guttate psoriasis, pityriasis rosea and lichen planus. Particularly, in pigment DSAP differential diagnosis focuses on lichen planus pigmentosus and lichenoid keratoses.
Treatment options for porokeratosis include cryotherapy, 5-fluorouracil, topical retinoids, topical tacrolimus and photodynamic therapy (5).
Due to the possibility of malignant transformation within porokeratosis to squamous cell carcinoma and Bowen’s disease, clinical surveillance with annual skin examinations and sun protection are key elements of the management of porokeratosis (4, 6).
Nevertheless, further observational studies are needed to increase recognition of this particular variant.
REFERENCES
- Zaar O, Polesie S, Navarrete-Dechent C, Errichetti E, Akay BN, Jaimes J, et al. Dermoscopy of porokeratosis: results from a multicentre study of the International Dermoscopy Society. J Eur Acad Dermatol Venereol 2021; 35: 2091–2096.
- Vargas-Mora P, Morgado-Carrasco D, Fustà-Novell X. Porokeratosis: A review of its pathophysiology, clinical manifestations, diagnosis, and treatment. Actas Dermosifiliogr (Engl Ed) 2020; 111: 545–560.
- Sertznig P, von Felbert V, Megahed M. Porokeratosis: present concepts. J Eur Acad Dermatol Venereol 2012; 26: 404–412.
- Tan TS, Tallon B. Pigmented porokeratosis. A further variant? Am J Dermatopathol 2016; 38: 218–221.
- Sotoodian B, Mahmood MN, Salopek TG. Clinical and dermoscopic features of pigmented disseminated superficial actinic porokeratosis: case report and literature review. J Cutan Med Surg 2018; 22: 229–231.
- Reyna-Rodríguez IL, García-Lozano JA, Ocampo-Candiani J. Pigmented disseminated superficial actinic porokeratosis in dark-skinned patients: Clinical, dermoscopic, and histopathologic features. J Cosmet Dermatol 2021; 20: 3054–3056.