QUIZ SECTION
A Middle-aged Man with Diffuse Red Papule: A Quiz
Lingling ZHANG, Yangyang MA, and Wenting HU*
Department of Dermatology, Hangzhou Third People’s Hospital, 38 Xihu Ave, Hangzhou 310009, PR China. E-mail: sendnote@126.com
Citation: Acta Derm Venereol 2024; 104: adv35386. DOI https://doi.org/10.2340/actadv.v104.35386.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Apr 2, 2024
A 47-year-old male presented with a 2-month history of diffuse, asymptomatic skin eruption involving the face, upper and lower extremities, abdomen, chest, and back. An extensive laboratory workup including complete blood cell count, comprehensive metabolic profile, ANA spectrum, erythrocyte sedimentation rate, serum protein electrophoresis, lipid profile, and angiotensin-converting enzyme level did not reveal any abnormalities. In addition, an age-related malignancy screen including a physical examination, colonoscopy, computed tomography scan of chest and abdomen, chest radiograph, and prostate-specific antigen level were then conducted, which were all within normal limits, and there was no lymphadenopathy or splenomegaly.
On presentation, the patient had hundreds of soft red papules, ranging in size from 0.5 to 1 cm, without scale crust, symmetrically scattered over the face, trunk, neck, and proximal upper extremities (Fig. 1a, b). The mucous membranes and cutaneous appendages were not involved. Biopsy of skin from the back demonstrated diffuse histiocytic infiltration in the dermis, with a few lymphocytes and neutrophils, and no foam cells or Touton giant cells (Fig. 1c). Immunohistochemically, cells expressed CD68 (Fig. 1d) and lysozyme, but were negative for S-100 protein.
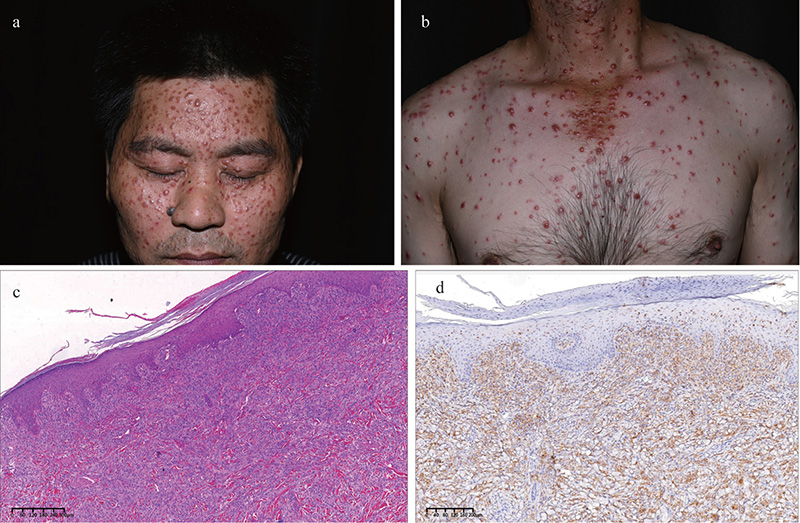
Fig. 1. (a, b) Dense red papules are visible on the patient’s face and trunk, (c) shows the hema-toxylin-eosin stain, and (d) displays a CD68 stain.
What is your diagnosis?
1. Rosai-Dorfman disease
2. Langerhans cell histiocytosis
3. Generalized eruptive histiocytoma
See next page for answer.
ANSWERS TO QUIZ
A Middle-aged Man with Diffuse Red Papule: A Commentary
Diagnosis: Generalized eruptive histiocytoma
Generalized eruptive histiocytoma (GEH), also called non-Langerhans cell histiocytosis, was first reported by Winkelmann and Muller in 1963 (1). Its clinical features include systemic, asymptomatic, multiple red or reddish-brown papules. It usually occurs in the face, trunk, and the proximal limbs, and will not induce systemic damage generally. Moreover, its histopathological findings are monomorphic tissue and cell infiltration within the dermis, cytoplasmic acidophily, clear nuclear membrane and nucleolus, with no foam cells or Touton giant cells. In immunohistochemistry analysis, the tissue-like cells are positive for CD36, but negative for S-100 and CD1a. No Birbeck granule is observed under the electron microscope.
GEH may be an early undifferentiated stage of a different histiocytosis, which can evolve into multiple juvenile type or adult type xanthogranuloma, disseminated xanthoma, progressive nodular histiocytosis, or multicentre reticular histiocytosis (2). Therefore, long-term follow-up is required for GEH. Most GEH cases are self-limiting, and the rash can spontaneously resolve within months to years, with no trace or only hyperpigmentation after resolution, and generally does not require treatment. Nonetheless, some patients may actively seek treatment due to mental stress. Corticosteroids, PUVA, and isotretinoin have been reported to be effective (3–5), but mainly in case reports. Therefore, whether treatment should be applied must be decided cautiously after sufficient physician–patient communication and benefit–risk balance.
REFERENCES
- Winkelmann RK, Muller SA. Generalized eruptive histiocytoma: a benign papular histiocytic reticulosis. Arch Dermatol 1963; 88: 586–596.
- Gianotti R, Alessi E, Caputo R. Benign cephalic histiocytosis: a distinct entity or a part of a wide spectrum of histiocytic proliferative disorders of children? A histopathological study. Am J Dermatopathol 1993; 15: 315–319.
- Takahashi S, Muto J, Takama H, Yanagishita T, Takeo T, Ohshima Y, Yuichiro O, et al. Generalized eruptive histiocytoma: pediatric case report and review of the published work. J Dermatol 2019; 46: e407–e408.
- Lan Ma H, Metze D, Luger TA, Steinhoff M. Successful treatment of generalized eruptive histiocytoma with PUVA. J Dtsch Dermatol Ges 2007; 5: 131–134.
- Kwinter J, DeKoven J. Generalized eruptive histiocytoma treated with isotretinoin. J Cutan Med Surg 2009; 13: 146–150.