ORIGINAL REPORT
Chronic Itch Affects Patients’ Ability to Experience Pleasure: Anhedonia in Itchy Disorders
Aleksandra STEFANIAK1,3, Magdalena BEREK-ZAMORSKA2, Claudia ZEIDLER3, Sonja STÄNDER3 and Jacek C. SZEPIETOWSKI1
1Department of Dermatology, Venereology and Allergology, Wrocław Medical University, Wrocław, Poland, 2Faculty of Social Sciences, Institute of Psychology, University of Silesia, Katowice, Poland, 3Center for Chronic Pruritus, Department of Dermatology, University Hospital of Münster, Münster, Germany
Abstract
Anhedonia, the reduced ability to experience pleasure, is a prevalent symptom in various psychiatric disorders, but has not been investigated in dermatological conditions, particularly those characterized by chronic itch. This study aimed to examine the prevalence and clinical correlates of anhedonia in patients with chronic itch. A cross-sectional study was conducted in 137 patients with chronic itch, classified according to the International Forum for the Study of Itch (IFSI) classification. Anhedonia was assessed using the Snaith–Hamilton Pleasure Scale (SHAPS) and Anticipatory and Consummatory Interpersonal Pleasure Scale (ACIPS). Itch severity, quality of life, and psychological distress were assessed using the Visual Analogue Scale (VAS), Verbal Rating Scale (VRS), ItchyQoL, and Hospital Anxiety and Depression Scale (HADS), respectively. The mean SHAPS score was 1.0 ± 1.7 points, and the mean ACIPS total score was 76.9 ± 16.2 points. In the study sample, 13.1% of patients were identified as anhedonic, with a higher prevalence observed in those with severe and very severe itch. Anhedonia was significantly correlated with itch severity (R = 0.2, p=0.02 for 24 h VASmean and SHAPS; R = 0.2, p = 0.01 for 24 h VASmax and SHAPS), anxiety symptoms (R = 0.3, p < 0.001 for SHAPS and HADS-anxiety), depression symptoms (R = 0.4, p < 0.001 for SHAPS and HADS-depression), and impairment in quality of life (R = 0.2, p = 0.014 for SHAPS and ItchyQoL). Anhedonia is a significant and prevalent aspect of psychological distress in patients with chronic itch. Addressing this symptom may not only improve patients’ overall mental health but also enhance the effectiveness of treatments for chronic itch. Future research is needed to elucidate further the mechanisms underlying the relationship between anhedonia and chronic itch and to develop targeted interventions for this population.
Key words: anhedonia; itch; psychodermatology; pruritus.
SIGNIFICANCE
This study explores the relationship between chronic itch and anhedonia – the reduced ability to experience pleasure – in patients with various itchy disorders. We found that the severity of itch, rather than its duration, was significantly associated with anhedonia. This suggests that effective management of itch severity could improve patients’ psychological well-being. Our findings also highlight the importance of considering anhedonia in the clinical assessment and treatment of patients with chronic itch. This research contributes to our understanding of the psychological impact of chronic itch and provides a basis for developing interventions to improve patients’ quality of life.
Citation: Acta Derm Venereol 2024; 104: adv35420. DOI https://doi.org/10.2340/actadv.v104.35420.
Copyright: © 2024 The Author(s). Published by MJS Publishing, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/).
Submitted: Jan 3, 2024; Accepted: Aug 5, 2024; Published: Aug 23, 2024
Corr: Prof. dr. Jacek C. Szepietowski, Department of Dermatology, Venereology and Allergology, Wrocław Medical University, Chałubińskiego 1, 50-368 Wrocław, Poland. E-mail: jacek.szepietowski@umed.wroc.pl
Competing interests and funding: MBZ declares no conflict of interest. AAS has received a speaker honorarium from Janssen. CZ has received speaker honoraria from Almirall, Beiersdorf, Galderma, Sanofi, Novartis, and Abbvie and support from Almirall, Beiersdorf, Galderma, and Sanofi. SS has received consultant fees from AbbVie, Almirall, Beiersdorf, Clexio, Escient, Galderma, Grünenthal, Incyte, IntegrityCE, Kiniksa, Klinge Pharma, Lilly, P.G. Unna Academy, Pfizer, Sanofi, TouchIME, Vifor, and WebMD, honoraria from AbbVie, BMS, FomF, Galderma, LeoPharma, L’Oreal, MEDahead, Moroscience, Novartis, Sanofi, P. G. Unna Academy, Pfizer, UCB, and Vifor, and support from Lilly, Novartis, P.G. Unna Academy, Sanofi, Vifor, and has participated in a data safety monitoring board from AbbVie, Almirall, Galderma, Lilly, Pfizer, Sanofi, and Vifor. JCS has received consulting fees from AbbVie, LEO Pharma, Novartis, Pierre Fabre, Sanofi Genzyme, Trevi, and UCB, speaker honoraria from AbbVie, Almirall, Eli Lilly, Novartis, Leo Pharma, UCB, Sanofi-Genzyme, Pfizer, and Pierre-Fabre, financial support from Sanofi-Genzyme and Novartis, and served as an investigator for AbbVie, Amgen, Bristol Myers Squibb, Galapagos, Galderma, Incyte, InflaRX, Janssen, Kliniksa, Kymab Limited, Menlo Therapeutics, Merck, Novartis, Pfizer, Regereron Pharmaceuticals, Inc., Trevi Therapeutics, and UCB Pharma, and is also President of the Polish Dermatological Society.
INTRODUCTION
Anhedonia can be understood as a lack of satisfaction with life, a lack of willingness to engage in life experiences or a lack of energy to live, or a loss or reduction in the ability to meet one’s primary and higher-order needs (1). This symptom may be generalized to all pleasant life experiences or involve reactions to stimuli of a specific type, for example, sensory stimuli or social contacts. Anhedonia is one of the main symptoms of depression, schizophrenia, post-traumatic stress disorder, anxiety disorders, addiction, Parkinson’s disease, suicidal tendencies, and eating disorders (2, 3). Moreover, anhedonia can occur as a separate disorder, manifested by an inability or difficulty to feel pleasure, without the other symptoms characteristic of depressive disorders (4).
Itch is defined as an unpleasant sensation that leads to the desire to scratch (5). It is a prevalent and upsetting symptom that can arise in dermatological conditions as well as chronic systemic disorders (5–10), placing a heavy burden on patients and lowering their quality of life (QoL) (11, 12). The International Forum for the Study of Itch (IFSI) classification is used by most researchers to categorize itch. Prior research (9, 10, 13) has emphasized the significance of the connection between mental health, QoL, and numerous itch illnesses. It has been widely established that there is a connection between common psychosocial and psychological components and dermatological conditions (14).
The objectives of this study were to examine the relationship between the ability of patients with chronic itch to experience pleasure as well as the relationship between social and sensory anhedonia and chronic itch.
MATERIAL AND METHODS
This prospective cross-sectional study was performed between June 2021 and December 2021. The project was approved by the local Ethical Committee (2007-413-f-S). We approached 150 consecutive adult patients who were treated due to chronic itch in the Competence Center Chronic Pruritus Universitätsklinikum Münster and 137 agreed to participate in the study (response rate: 91.3%). Demographics for the whole population are given in Table I. Exclusion criteria for this analysis included mental status changes making the patient unable to make a detailed assessment of itch.
After inclusion, detailed information on clinical history, utilized therapies, and physical findings were recorded. All patients were classified according to International Forum for the Study of Itch (IFSI) classification (15).
Clinical parameters such as bodyweight, height, and BMI were checked. Itch assessment was performed in all patients: the Visual Analogue Scale (VAS) and Verbal Rating Scale (VRS) (16, 17). Patients were asked to assess the maximal and average itch experienced during the last 4 weeks and last 24 h. Based on VASmax in the last 24 h patients were divided into 4 groups based on itch intensity (0– 3 points represents mild itch, 4–6 points moderate itch, 7–8 points severe itch, and ≥ 9 points severe itch) (18).
ItchyQol (19–21) and the Hospital Anxiety and Depression Scale (HADS) (22) were applied to assess connections between itch with psychosocial status and life quality impairment. The first primary questionnaire devoted to itchy conditions, ItchyQoL, concentrates not only on the impact of itch on daily activities, but also on the symptoms’ characteristics and the perceived level of psychological burden. It assesses the itch’s 3 aspects: symptoms, functioning, and emotions. (21). ItchyQoL is also suitable for use in patients with itch without primary skin lesions. The ItchyQoL assessment consists of 22 questions, each of which is scored on a 5-point scale from 1 (never) to 5 (all the time). The sum of these scores determines the ItchyQoL score (22–110 points). The overall ItchyQoL score reflects the degree of itch-specific QoL impairment, and ranges from 0 to 30 points (very mild) to 31 to 50 points (mild), 51 to 80 points (moderate), and 81 to 110 points (severe impairment) (19). The subscales (symptoms, functioning, and emotions) are calculated as the mean scores pertaining to that category (range 1–5 points) (23). The 14-item HADS (23) is a self-evaluation rating scale that is used to assess depression and anxiety. It has 7 items for evaluating anxiety and 7 for assessing depression, each scoring 0 to 3 points. Scores between 0 and 7 points are regarded as normal cases, 8 to 10 points as borderline cases, and 11 to 21 points as abnormal cases needing additional testing or treatment.
The main parameter – anhedonia – was assessed according to the Snaith–Hamilton Pleasure Scale (SHAPS) (23) and Anticipatory and Consummatory Interpersonal Pleasure Scale (ACIPS) (24).
SHAPS is a self-reported tool for measuring hedonic capacity/hedonic tone, focusing on the consummatory aspect of pleasure, i.e., getting satisfaction from experiencing pleasurable sensations. One of the questionnaire’s assumptions is to describe the feeling of pleasure as a state that can change. This property is very useful in examining patients and the sense of pleasure during disease progression/treatment. It consists of 14 statements that the respondent evaluates on a 4-point scale (definitely agree, agree, disagree, and strongly disagree). The scoring model was based on the general health questionnaire, so both “disagree” responses score 0 and both “agree” responses score 1 point. SHAPS score is the sum of the 14 items, so the score range is 0–14 points. Hedonic capacity is the ability to feel pleasure; hence the higher scores obtained on the scale are understood as the intensification of difficulties related to experiencing pleasure, i.e., anhedonia. Respondents who scored >2 points are suggested to have a lowered hedonistic tone – anhedonia (23). The original version of the scale is characterized by satisfactory reliability and validity of the scale (23), as is the German (2) adaptation of the scale that was used in the study.
ACIPS (24) is a tool that measures the level of ability to experience interpersonal and social pleasure. The questionnaire is a self-report tool and consists of 17 statements regarding social interactions with others and regarding making and maintaining relationships. Seven of them concern anticipatory anhedonia (related to the pleasure-seeking motivation, and prediction of it), and 10 consummatory anhedonia, which is related to the satisfaction derived from a pleasant experience. Additionally, the scale may also be used to measure intimate social interactions (ACPIS-ISI), group social interactions – casual socialization (ACIPS-GSI), and social bonding and making connections (ACIPS-SBMC) (24). The 3 factors we observed correspond to 3 different levels of social connectedness, ranging from relatively intimate to more casual (25). The answers given by the respondents are scored on a 6-point Likert scale, where 1 means “very false for me” and 6 “very true for me”, with lower scores indicating a greater likelihood of anhedonia related to interpersonal relations and participation in social life. Official translation by Kirst into German (“Skala der erwarteten und der vollendeten zwischenmenschlichen Freude”) was utilized in the study (26).
Statistical analysis
Statistical analysis of the variables was performed using the Jamovi statistical program (version 2.3.21.0; https://www.jamovi.org/). Due to the distribution of variables that did not meet the criterion of normality, non-parametric tests were used in statistical analysis. The analysis of correlations between the variables was carried out using Spearman’s coefficient. The significance of differences between groups was determined using the Mann–Whitney U test (independent samples t-test), and Kruskal–Willis statistics (non-parametric one-way ANOVA) were used for group comparisons. Results with p-values less than 0.05 were considered statistically significant.
RESULTS
Patient population
A total of 137 patients with itch on diseased skin (IFSI 1) (n = 42), non-diseased skin (IFSI 2) (n = 46), and with chronic scratch lesions (IFSI 3) (n = 49) were included in the analysis. The most common itch origin was dermatological (47.5%), followed by neurological (24.1%), mixed (17.5%), systemic (5.1%), and psychological origin (0.7%). Furthermore, 5.1% of patients had an itch of unknown origin.
The mean duration of itch was 9.9 ± 5.7 (range: 5–76, median 5) years. The mean VASmean in the last 24 h was 4.9 ± 2.9 points (range: 2–10 points), and mean VASmax was 5.8 ± 2.8 points (range: 2–10 points), indicating moderate itch. During the last 4 weeks VASmax was 6.5 ± 2.5 points (range: 2–10 points). On the verbal scale VRSmean was 2.2 ± 0.9 points (range: 0–4 points, median 2 points) and VRSmax was 2.3 ± 1.0 points (range: 0–4 points, median 2 points). There were no significant differences between the IFSI groups in terms of itch intensity, nor due to the origin of itch (detailed data not shown). Among the participants, 26 patients (19%) reported experiencing mild itch, 50 patients (36.5%) reported moderate itch, 26 patients (19%) declared severe itch, and 35 patients (25.5%) reported very severe itch. With reference to HADS, the prevalence of anxiety and depression among patients was 17% (anxiety) and 13% (depression). The mean ItchyQoltotal score was calculated to be 67.1 ± 20.1 points (range: 22–11 points, median 66 points), denoting moderate impairment in QoL caused by itch (Table II).
| ItchyQol subscale | Mean ± SD (median) |
| Symptoms | 3.3 ± 0.9 (3) |
| Functioning | 3.1 ± 1 (3.3) |
| Emotions | 2.9 ± 1 (2.8) |
| Combined | 3.05 ± 0.9 (3) |
| ItchyQoL: Itch-specific Quality of Life questionnaire. | |
Anhedonia measurements
The SHAPS mean score was evaluated at 1.0 ± 1.7 points (with a range of 0–8 points and a median of 0 points). Based on the SHAPS score, altogether 18 patients (13.1%) were identified as anhedonic, with 11.9% in IFSI group I, 10.9% in group II, and 16.3% in IFSI III group (the differences between the groups are not statistically significant). When considering the severity of itch, it was observed that among patients with very severe itch, 23% were anhedonic. Among those with severe itch, 26.9% were anhedonic, whereas only 11.5% of patients with moderate itch and 6% with mild itch were identified as anhedonic (Fig. 1).
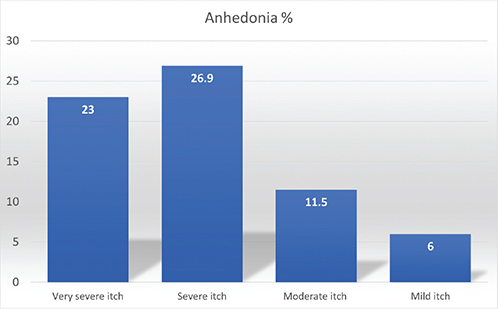
Fig. 1. Presence of anhedonia regarding itch severity.
Anticipatory anhedonia, as measured by the ACIPS scale, had a score of 30.3 ± 6.7 points (range: 10–42 points; median: 31 points), whereas the mean score for consummatory anhedonia was 45.9 ± 10.2 points (range: 11–60 points; median: 47 points). The mean social anhedonia (ACIPS total) on the ACIPS scale scored 76.9 ± 16.2 points (range: 21–99 points; median: 80 points). No significant differences were observed between the IFSI groups (Table III). With reference to itch origin, patients with a neurological origin of itch had higher scores on the SBMC subscale of ACIPS score in comparison with patients with itch of another origin (Fig. 2). Patients with other sources of itch did not differ on the anhedonia subscales.
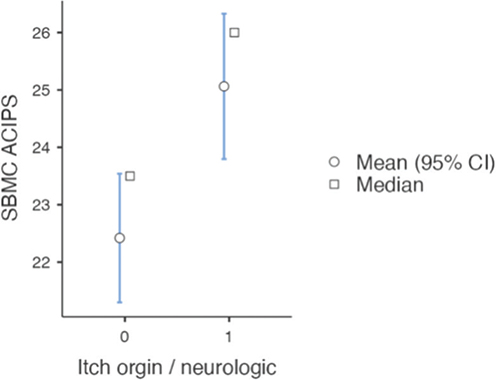
Fig. 2. Independent samples t-test: itch origin neurological and pulled together other causes of itch and relation to social bonding and making connections (p = 0.021). SBMC: social bonding and making connections; ACIPS: Anticipatory and Consummatory Interpersonal Pleasure Scale.
The analysed data revealed the occurrence of significant negative correlations within the study group between the measures of general anhedonia (on the SHAPS scale) and all subscales of the questionnaire assessing the level of pleasure experienced in social scenarios (ACIPS). The negative correlations with the overall level of anhedonia were observed primarily in the domain of consummatory pleasure derived from social relationships, such as satisfaction with social connections, and an anticipatory subscale of ACIPS (r = –0.2, p = 0.01). Furthermore, negative correlations were noted with the pleasure obtained from group social interactions (consummatory subscale of ACIPS) (r = –0.3, p < 0.001), social bonding (GSI ACIPS) (r = –0.3, p < 0.001), and the establishment of new contacts (SBMC ACIPS, r = –0.3, p < 0.001) (detailed data not shown).
There was no correlation found between the duration of itch and anhedonia as measured by either the SHAPS or the ACIPS scales (detailed data not shown). However, there were significant correlations observed between itch intensity measured on the VAS scale (daily mean, daily worst, 4 weeks worst) and the VRS scale (daily mean) and the total SHAPS score (Table IV). On the other hand, no statistically significant correlations were found between ACIPS scores and itch intensity (detailed data not shown).
| Measure | 24 h VASmean & SHAPS | 24 h VASmax & SHAPS | 4 weeks VASmean & SHAPS | 4 weeks VASmax & SHAPS | 24 h VRSmean & SHAPS | 24 h VRSmax & SHAPS |
| R | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.1 |
| p-value | 0.02* | 0.01* | 0.07 | 0.014* | 0.011* | 0.143 |
| VAS: Visual Analogue Scale; VRS: Verbal Rating Scale; SHAPS: Snaith–Hamilton Pleasure Scale. * Statistically significant. | ||||||
Additionally, there were significant correlations observed between the questionnaires measuring anhedonia and pleasure in social relations, as well as the HADS questionnaire in both depressive and anxiety symptoms. Specifically, there were negative correlations observed between the level of pleasure from social relations in all the studied aspects and anxiety symptoms (Table V).
| Correlation | ACIPS – anticipatory | ACIPS – consummatory | ACIPS – ISI | ACIPS – GSI | ACIPS – SBMC | SHAPS | |
| HADS (total) | r | –0.3 | –0.3 | –0.3 | –0.4 | –0.3 | 0.4 |
| p | 0.003* | <0.001* | 0.004* | <0.001* | 0.003 | <0.001* | |
| HADS – anxiety | r | –0.2 | –0.3 | –0.2 | –0.3 | –0.2 | 0.3 |
| p | 0.016* | 0.002* | 0.015* | 0.002* | 0.015* | <0.001* | |
| HADS depression | r | –0.4 | –0.3 | –0.3 | –0.4 | –0.3 | 0.4 |
| p | <0.001* | <0.001* | <0.001* | <0.001* | 0.001* | <0.001* | |
| HADS: Hospital Anxiety and Depression Scale; ACIPS: Anticipatory and Consummatory Interpersonal Pleasure Scale; ISI: intimate social interactions; GSI: group social interactions; SBMC: social bonding and making connections; SHAPS: Snaith–Hamilton Pleasure Scale. * Statistically significant. |
|||||||
There were significant correlations observed between social pleasure derived from group social interaction (ACIPS-GSI) and the overall QoL associated with chronic itch as measured by ItchQoL (r = –0.2, p = 0.032), as well as its emotion (r = –0.2, p = 0.029) and symptom subtypes (r = –0.2, p = 0.01). Additionally, the level of general anhedonia as measured by the SHAPS scale was significantly associated with the overall QoL associated with itch and its subtypes. Specifically, higher levels of general anhedonia were associated with higher impairment of itch-specific QoL (r = 0.2, p = 0.014), as well as its subtypes related to emotions (r = 0.2, p = 0.048), functioning (r = 0.2, p = 0.032), and symptoms (r = 0.2, p = 0.009). There were statistically significant correlations between the level of anticipatory social pleasure and more advanced age (ACIPS – anticipatory) (r = –0.2, p = 0.02). No statistically significant correlations were found between the results of questionnaires measuring any kind of anhedonia and the level of BMI in the study group (detailed data not shown).
DISCUSSION
To our knowledge, this is the first study measuring anhedonia in the dermatological field. Anhedonia, defined as the reduced ability to experience pleasure, has been widely studied in the context of various psychiatric disorders, such as major depressive disorder and schizophrenia (27, 28). However, its role in dermatological conditions, particularly those characterized by chronic itch, has not been investigated.
In general populations, the prevalence of anhedonia ranges from 5% to 11% (1, 29). In our study, 13.1% of patients were identified as anhedonic, which is slightly higher than the prevalence found in the general population. In our study, the mean SHAPS score was 1.0 ± 1.7 points, while the mean ACIPS total score was 76.9 ± 16.2 points. To put these scores into context, we can compare them with the scores reported in studies involving the general population. According to the meta-analysis provided by Trøstheim et al. (30), a mean SHAPS score in the general population is 0.6 points (0.4–0.8 points), which is lower than the mean score observed in our study. Gooding et al. (31), based on the non-clinical sample, reported a mean total score of 87.83 points, which is higher than the mean score observed in our study. This indicates that patients with chronic itch may experience lower levels of social pleasure compared with the general population.
Anhedonia has been studied in various psychiatric and neurological diseases, such as major depressive disorder, schizophrenia, and Parkinson’s disease. In these conditions, the prevalence of anhedonia, as measured by the SHAPS, ranges from 20% to 60%, with mean SHAPS of 5.8 points (5.2–6.5 points) in major depressive disorder (30), 2.7 points (0.8–4.6 points) in schizophrenia (30), 2.1 points (1.5–2.8 points ) in bipolar disorder (30), 1.7 points (1.5–2.0 points) in substance misuse disorders (30), 1.6 points (1.3–1.9 points) in chronic pain (30), and 1.5 points (1.1–1.9 points) in Parkinson’s disease (30), with higher levels of anhedonia associated with more severe symptoms and poorer prognosis (28, 32, 33).
In our study, we found significant negative correlations between general anhedonia and various aspects of social pleasure, as measured by the ACIPS scale. This is in line with previous research, which has shown that anhedonia is associated with impairments in social functioning and reduced pleasure from social interactions (34, 35). Interestingly, we found that patients with neurological origin of itch had higher scores on the social bonding and making connections subscale of the ACIPS compared patients with itch of other origins. This observation may indicate that the neurological basis of itch might have a unique impact on patients’ social functioning and ability to establish new connections. Further research is needed to elucidate the underlying mechanisms and potential implications of this finding. Furthermore, we found significant associations between anhedonia and both anxiety and depression symptoms, as well as overall QoL associated with itch, regardless of the type of itch. These findings highlight the potential impact of chronic itch on patients’ psychological well-being and underscore the importance of addressing anhedonia in the management of chronic itch.
The lack of correlation between the duration of itch and anhedonia in our study suggests that the impact of chronic itch on patients’ ability to experience pleasure may be more closely related to the severity of itch rather than its duration. In contrast, some studies in other conditions, such as major depressive disorder and schizophrenia, have reported associations between the duration of illness and anhedonia (28, 32). This discrepancy might be attributed to differences in the underlying pathophysiology and psychological impact of chronic itch compared with these psychiatric disorders. Our results are in line with previous research on the impact of itch severity on patients’ QoL and psychological well-being in dermatological conditions. For example, in our previous study on itch in diabetes, the severity of itch in diabetic patients was significantly associated with increased anxiety and depression (10). Similarly, a study by Dalgard et al. (36) found that the severity of skin symptoms in patients with various dermatological conditions was significantly correlated with psychological distress and impairments in QoL. Also, other psychodermatological factors, such as perceived stigmatization, depend on higher clinician-assessed disease severity and the presence of itch, as it was shown in previous studies (37). The association between anhedonia and itch severity in our study highlights the importance of addressing itch severity in the clinical management of patients with chronic itch. Effective interventions targeting itch severity may not only improve patients’ physical symptoms but also enhance their psychological well-being by reducing anhedonia.
The relationship between chronic itch and anhedonia may be mediated by various factors, such as the direct impact of itch on patients’ mood and sleep, the social stigma associated with visible skin lesions and need to scratch, and the psychological distress caused by the chronic and often unpredictable nature of itch (38). In light of these findings, it is crucial for healthcare professionals to consider anhedonia when assessing and treating patients with chronic itch. This may involve the use of targeted psychological interventions, such as cognitive-behavioural therapy or mindfulness-based approaches, which have been shown to be effective in reducing anhedonia and improving psychological well-being in various clinical populations (28, 39). Also, there is a possibility worth exploring: that improving itch by treating the disease could improve anhedonia.
Limitations
There are several limitations to our study that should be acknowledged. First, the cross-sectional design of the study does not allow for the examination of causal relationships between anhedonia and itch severity, QoL, and psychological distress. Also, feeling anhedonia could modify the perception of itch. Longitudinal studies are needed to investigate the temporal relationships between these variables and to determine whether anhedonia is a risk factor for or a consequence of chronic itch. Second, our sample was relatively small and consisted of patients from a single centre, which may limit the generalizability of our findings to other populations. Future research should aim to replicate our findings in larger, more diverse samples of patients with chronic itch.
Conclusion
Our study provides novel insights into the relationship between chronic itch and anhedonia in patients with various itchy disorders. Our findings highlight the significant impact of chronic itch on patients’ ability to experience pleasure and suggest that addressing anhedonia and related psychological factors should be an integral part of the clinical management of chronic itch. Further research is needed to better understand the underlying mechanisms linking chronic itch and anhedonia, as well as to develop effective interventions for improving patients’ well-being and QoL.
REFERENCES
- Snaith RP, Hamilton M, Morley S, Humayan A, Hargreaves D, Trigwell P. A scale for the assessment of hedonic tone: the Snaith-Hamilton Pleasure Scale. Br J Psychiatry 1995; 167: 99–103. https://doi.org/10.1192/bjp.167.1.99
- Franz M, Lemke MR, Meyer T, Schroeder T, Schaub RT, Wolf K. Die deutsche Version der Snaith-Hamilton-Pleasure-Skala (SHAPS-D). Anhedonie bei schizophrenen und depressiven Patienten. Fortschr Neurol Psychiatr 1998; 66: 407–413. https://doi.org/10.1055/s-2007-995279
- Gooding DC, Pflum MJ. The ACIPS: moving forward in the assessment of negative symptoms. Schizophr Res 2016; 176: 327–328. https://doi.org/10.1016/j.schres.2016.06.002
- Thomsen KR, Whybrow PC, Kringelbach ML. Reconceptualizing anhedonia: novel perspectives on balancing the pleasure networks in the human brain. Front Behav Neurosci 2015; 9: 49. https://doi.org/10.3389/fnbeh.2015.00049
- Ständer S, Streit M, Darsow U, Metze D, Luger T, Szepietowski JC. Diagnostische und therapeutische Verfahren bei chronischem Pruritus. J Dtsch Dermatol Ges 2006; 4: 350–370. https://doi.org/10.1111/j.1610-0387.2006.05887.x
- Steinhoff M, Bienenstock J, Schmelz M, Luger T, Weisshaar E, Metze D. Neurophysiological, neuroimmunological, and neuroendocrine basis of pruritus. J Invest Dermatol 2006; 126: 1705–1718. https://doi.org/10.1038/sj.jid.5700231
- Stefaniak A, Chlebicka I, Szepietowski J. Itch in diabetes: a common underestimated problem. Adv Dermatol Allergol 2021; 38: 177–183. https://doi.org/10.5114/ada.2019.89712
- Chlebicka I, Stefaniak AA, Matusiak Ł, Szepietowski JC. Is basal cell carcinoma an itchy tumor? Clinical characteristics of itch in basal cell carcinoma. J Clin Med 2020; 9: 2386. https://doi.org/10.3390/jcm9082386
- Stefaniak AA, Zubkiewicz-Kucharska A, Matusiak Ł, Szepietowski JC. Itch in children with Type 1 diabetes: a cross-sectional study. Dermatol Ther (Heidelb) 2020; 10: 745–756. https://doi.org/10.1007/s13555-020-00403-w
- Stefaniak AA, Krajewski PK, Bednarska-Chabowska D, Szepietowski JC. Itch in adult population with type 2 diabetes mellitus: clinical profile, pathogenesis and disease-related burden in a cross-sectional study. Biology (Basel) 2021; 10: 1332. https://doi.org/10.3390/biology10121332
- Weisshaar E, Szepietowski J, Darsow U, Misery L, Wallengren J, Mettang T. European Guideline on chronic pruritus. Acta Derm Venereol 2012; 92: 563–581. https://doi.org/10.2340/00015555-1400
- Szepietowski JC, Reich A. [Itch: Pathomechanism, clinical aspects, treatment.] Poznań: Termedia, 2010.
- Chlebicka I, Stefaniak A, Matusiak Ł, Szepietowski JC. Burden of itch in patients with basal cell carcinoma. Acta Derm Venereol 2021; 101: adv00507. https://doi.org/10.2340/00015555-3871
- Reszke R, Szepietowski JC. Itch and psyche: bilateral associations. Acta Derm Venereol 2020; 100: 28–36. https://doi.org/10.2340/00015555-3346
- Ständer S, Weisshaar E, Mettang T, Szepietowski JC, Bergasa NV, Gieler U. Clinical classification of itch: a position paper of the International Forum for the Study of Itch. Acta Derm Venereol 2007; 87: 291–294. https://doi.org/10.2340/00015555-0305
- Reich A, Riepe C, Anastasiadou Z, Homola A, Ständer S, Szepietowski JC. Itch assessment with visual analogue scale and numerical rating scale: determination of minimal clinically important difference in chronic itch. Acta Derm Venereol 2016; 96: 978–980. https://doi.org/10.2340/00015555-2433
- Phan NQ, Blome C, Fritz F, Gerss J, Reich A, Ebata T. Assessment of pruritus intensity: prospective study on validity and reliability of the visual analogue scale, numerical rating scale and verbal rating scale in 471 patients with chronic pruritus. Acta Derm Venereol 2012; 92: 502–507. https://doi.org/10.2340/00015555-1246
- Reich A, Chatzigeorkidis E, Zeidler C, Osada N, Schaap FJ, Ständer S. Tailoring the cut-off values of the visual analogue scale and numeric rating scale in itch assessment. Acta Derm Venereol 2017; 97: 759–760. https://doi.org/10.2340/00015555-2642
- Love EM, Marrazzo GA, Kini S, Mancini AJ, Muizzuddin N, Maibach HI. ItchyQoL bands: pilot clinical interpretation of scores. Acta Derm Venereol 2015; 95: 114–115. https://doi.org/10.2340/00015555-1891
- Zeidler C, Steinke S, Riepe C, Storck M, Thierry L, Arents BWM. Cross-European validation of the ItchyQoL in pruritic dermatoses. J Eur Acad Dermatol Venereol 2019; 33: 391–397. https://doi.org/10.1111/jdv.15225
- Stumpf A, Pfleiderer B, Fritz F, Nau R, Darsow U, Ständer S. Assessment of quality of life in chronic pruritus: relationship between itchyQoL and dermatological life quality index in 1,150 patients. Acta Derm Venereol 2018; 98: 142–143. https://doi.org/10.2340/00015555-2782
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983; 67: 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
- Snaith RP, Hamilton M, Morley S, Humayan A, Hargreaves D, Trigwell P. A scale for the assessment of hedonic tone: the Snaith-Hamilton Pleasure Scale. Br J Psychiatry 1995; 167: 99–103. https://doi.org/10.1192/bjp.167.1.99
- Gooding DC, Pflum MJ. The assessment of interpersonal pleasure: introduction of the Anticipatory and Consummatory Interpersonal Pleasure Scale (ACIPS) and preliminary findings. Psychiatry Res 2014; 215: 237–243. https://doi.org/10.1016/j.psychres.2013.10.012
- Gooding DC, Fonseca-Pedrero E, de Albéniz AP, Ortuno-Sierra J. Spanish adaptation of the adult version of the Anticipatory and Consummatory Interpersonal Pleasure Scale. Rev Psiquiatr Salud Ment 2016; 9: 70–77. https://doi.org/10.1016/j.rpsm.2015.10.006
- Daniels A, Wellan SA, Walter H. Learning it the hard way: how enjoying life and positive appraisal buffer the negative effects of stressors on mental health in the COVID-19 pandemic. J Affect Disord Rep 2021; 6: 100266. https://doi.org/10.1016/j.jadr.2021.100200
- Treadway MT, Zald DH. Reconsidering anhedonia in depression: lessons from translational neuroscience. Neurosci Biobehav Rev 2011; 35: 537–555. https://doi.org/10.1016/j.neubiorev.2010.06.006
- Rizvi SJ, Pizzagalli DA, Sproule BA, Arnone D, Kennedy SH. Assessing anhedonia in depression: potentials and pitfalls. Neurosci Biobehav Rev 2016; 65: 21–35. https://doi.org/10.1016/j.neubiorev.2016.03.004
- Franken IHA, Rassin E, Muris P. The assessment of anhedonia in clinical and non-clinical populations: further validation of the Snaith-Hamilton Pleasure Scale (SHAPS). J Affect Disord 2007; 99: 83–89. https://doi.org/10.1016/j.jad.2006.08.020
- Trøstheim M, Eikemo M, Meir R, Zunhammer M, Jääskeläinen IP, Leknes S. Assessment of anhedonia in adults with and without mental illness: a systematic review and meta-analysis. JAMA Netw Open 2020; 3: e2013233. https://doi.org/10.1001/jamanetworkopen.2020.13233
- Gooding DC, Pflum MJ. Further validation of the ACIPS as a measure of social hedonic response. Psychiatry Res 2014; 215: 771–777. https://doi.org/10.1016/j.psychres.2013.11.009
- Pelizza L, Ferrari A. Anhedonia in schizophrenia and major depression: state or trait? Ann Gen Psychiatry 2009; 8: 22. https://doi.org/10.1186/1744-859X-8-22
- Assogna F, Cravello L, Caltagirone C, Spalletta G. Anhedonia in Parkinson's disease: a systematic review of the literature. Mov Disord 2011; 26: 1825–1834. https://doi.org/10.1002/mds.23815
- Gooding DC, Winston TM, Pflum MJ, Burgin CJ. Individual differences in hedonic experience: further evidence for the construct validity of the ACIPS. Psychiatry Res 2015; 229: 524–532. https://doi.org/10.1016/j.psychres.2015.05.061
- Gard DE, Kring AM, Gard MG, Horan WP, Green MF. Anhedonia in schizophrenia: distinctions between anticipatory and consummatory pleasure. Schizophr Res 2007; 93: 253–260. https://doi.org/10.1016/j.schres.2007.03.008
- Dalgard FJ, Gieler U, Tomas-Aragones L, Lien L, Poot F, Jemec GBE. The psychological burden of skin diseases: a cross-sectional multicenter study among dermatological out-patients in 13 European countries. J Invest Dermatol 2015; 135: 984–991. https://doi.org/10.1038/jid.2014.530
- Van Beugen S, Schut C, Kupfer J, Smits T, Ferwerda M, Spillekom-van Koulil S. Perceived stigmatization among dermatological outpatients compared with controls: an observational multicentre study in 17 European countries. Acta Derm Venereol 2023; 103: e6485. https://doi.org/10.2340/actadv.v103.6485
- Yosipovitch G, Rosen JD, Hashimoto T. Itch: From mechanism to (novel) therapeutic approaches. J Allergy Clin Immunol 2018; 142: 1375–1390. https://doi.org/10.1016/j.jaci.2018.09.005
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol 2010; 78: 169–183. https://doi.org/10.1037/a0018555