ORIGINAL REPORT
The Circadian Rhythm of Itching among 241 Adults with Atopic Dermatitis: A Cross-sectional Study
Xiaoxue SANG1#, Jianyun LU2,3#, Lina TAN2,3, Jinrong ZENG2,3, Dan WANG2,3, Aiyuan GUO2,3, Siyuan TANG1, Qian ZENG1, Wei LIU1 and Lihua GAO2,3
1Xiangya Nursing School, Central South University, Changsha, Hunan, 2The Third Xiangya Hospital, Central South University, Changsha, Hunan, and 3Medical Ozone Research Center of Central South University, Changsha, Hunan, China
#These authors contributing equally to this work and share first authorship.
The pattern of itching in patients with atopic dermatitis has not been systematically studied. Therefore, this study aimed to assess the pattern of itching in adults with atopic dermatitis using questionnaires to assess for a circadian rhythm of itching in participating patients at a single institution (n = 241). A self-report questionnaire was used to assess circadian rhythm and intensity of itching in patients. In addition, the patients’ disease severity (Eczema Area and Severity Index [EASI]) and quality of life (Dermatology Life Quality Index [DLQI]) were assessed. Itching occurred most frequently (74.69%) and with the greatest severity (62.66%) between 20:00 and 00:00, and the least number of patients (25.31%) experienced itching between 04:00 and 08:00. The DLQI and EASI scores both correlated with the average and maximum itch intensity (r = 0.582, r = 0.533, respectively; r = 0.539, r = 0.517, respectively; p < 0.001). The DLQI and EASI scores were associated with average itch intensity (B = 0.179, B = 0.204, respectively; 95% CI: 0.112 to 0.246, 95% CI: 0.096 to 0.313, respectively; p < 0.001), and the EASI score was associated with males and family history (B = 0.285, B = 0.287, respectively; 95% CI: 0.094 to 0.476, 95% CI: 0.096 to 0.478, respectively; p = 0.003). Adult patients with atopic dermatitis exhibited a circadian rhythm of itching; these study results could positively impact treatment approaches.
SIGNIFICANCE
This study systematically and comprehensively describes the circadian rhythm characteristics of itching in 241 adult patients with atopic dermatitis. Itch in adult patients with atopic dermatitis occurred most frequently and with the greatest severity between 20:00 and 00:00, and the least number of patients experienced itching between 04:00 and 08:00. This study lays a foundation for further research on the occurrence and regulatory mechanisms of itching, and also provides a basis for chronotherapy (which may enhance treatment efficacy and mitigate medication-related side effects).
Key words: atopic dermatitis; circadian rhythm; itch; questionnaire.
Citation: Acta Derm Venereol 2024; 104: adv35427. DOI: https://doi.org/10.2340/actadv.v104.35427.
Copyright: © 2024 The Author(s). Published by MJS Publishing, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/).
Submitted: Jan 3, 2024. Accepted after revision: Jun 10, 2024. Published: Aug 5, 2024
Corr: Wei Liu, Xiangya Nursing School, Central South University, 172 Tongzipo Road, Changsha, Hunan, 410013, P.R. China and Lihua Gao, The Third Xiangya Hospital, Central South University, 138 Tongzipo Road, Changsha, Hunan, 410013, P.R. China. E-mails: Liuw079@csu.edu.cn, 49516596@qq.com
Competing interests and funding: The authors have no conflicts of interest to declare.
INTRODUCTION
Atopic dermatitis (AD) is a non-fatal dermatosis with the highest global disease burden and is characterized by dry skin and intense itching (1). According to an international time-trend survey of the incidence and prevalence of AD, the prevalence ranges from 2% to 17.6% (2). Itching is not only the most important and typical symptom of AD but is also a contributing factor in the exacerbation and recurrence of AD (3, 4). Itching often worsens at night, which not only seriously affects the physical and mental health of patients, but also may aggravate the disease (1, 5). Therefore, controlling nocturnal itching is of great significance in breaking the itch–scratch cycle and alleviating AD. Elucidating the circadian rhythm and specific characteristics of itching is important information for the development of treatments to manage AD.
Circadian rhythms are biological rhythms expressed in physiological or biological behaviours in cycles of approximately 24 h (6). These rhythms also play a role in influencing both normal and pathological processes within the skin, including temperature regulation, blood flow, transdermal water loss, and even itching (7–10). Previous studies have shown that itching is worse at night in individuals with AD (11, 12); however, the 24-h circadian rhythms of itching in adults with AD have not been systematically studied.
Chronotherapy is a therapeutic approach that aligns medication administration with circadian rhythms to enhance treatment efficacy and mitigate side effects (13, 14). Yoshioka et al. (15) conducted a study which revealed that nocturnal application of topical corticosteroids led to improved management of psoriasis plaques. This finding highlight the potential benefits of chronotherapeutic strategies for dermatological treatment. Defining the circadian rhythm of itching in patients with AD may elucidate the mechanisms of itch modulation and lead to targeted temporal therapies for managing itching. Therefore, this study aimed to investigate circadian rhythm patterns of itching in adult patients with AD using a cross-sectional questionnaire.
MATERIALS AND METHODS
Study design and participants
A total of 252 questionnaires were collected from patients by convenience sampling at the Third Xiangya Hospital of Central South University, Changsha, China, between September 2021 and October 2023. The response rate was 100%, with a valid questionnaire response rate of 95.63% (241/252). The researchers provided guidance and explanations for patients who had problems completing the questionnaires. The questionnaires were collected anonymously. Finally, a total of 241 patients aged 18–87 years completed the questionnaire. The inclusion criteria were as follows: (i) adult patients (18 years or older), (ii) patients who met the Hanifin–Rajka criteria (16) for the clinical diagnosis of AD, and (iii) patients in whom this was the first dermatological appointment. The exclusion criteria were as follows: (i) recent sleep disorders, irregular eating habits, or sleeping with lights on at night, as these factors can lead to circadian rhythm disruption; (ii) serious physical or mental illnesses that prevented cooperation with the researcher; and (iii) other conditions that could cause itching. This study was approved by the hospital ethics committee (approval number: Fast 23345). Written informed consent was obtained from each participant before any study-related procedures were performed.
Itch questionnaire
All participants were asked to complete a self-report questionnaire that has 5 questions on itch circadian rhythm and intensity (Fig. S1). The self-report questionnaire was developed by 9 experienced experts in our research group and revised in the clinic after 2 months of pre-experiment. Before assessing the circadian rhythm and intensity of itching, patients were asked whether the intensity of itching was the same throughout the day. If the patient reported variations in itch intensity across different times of the day, they were prompted to continue to the next question. Conversely, if the intensity was reported as consistent, the questionnaire was terminated. As to circadian rhythm of itching, we divided 24 h of the day into 6 time periods (00:00–04:00, 04:00–08:00, 08:00–12:00, 12:00–16:00, 16:00–20:00, and 20:00–00:00) (17, 18). The patients selected the time periods of a day when the itching occurred and when the worst itching occurred (multiple choice). To quantify the average itch intensity and the maximum itch intensity of the patient during a day, an 11-point numeric rating scale (NRS) was employed, with 0 representing “no itch“ and 10 indicating “the worst imaginable itch“. Patients choose the scores in NRS respectively for the average itch intensity and the maximum itch intensity of a day (multiple choice).
Eczema Area and Severity Index
The Eczema Area and Severity Index (EASI) provides a comprehensive assessment of the head and neck (H), upper limbs (UL), trunk (T), and lower limbs (LL). Four body regions are assigned a score based on the percentage of the area involved (A): 0 (no eruption), 1 (0–9%), 2 (10–29%), 3 (30–49%), 4 (50–69%), 5 (70–89%), and 6 (90–100%). The 4 body regions are also assessed for erythema (E), induration/population (I), excoriation (Ex), and lichenification (L) depending on their severity. These 4 body regions are assigned a score of 0–3 according to the severity: 0 representing none, 1 representing mild, 2 representing moderate, and 3 representing severe. The EASI scores range from 0 to 72, and are calculated using the following formula: EASI = 0.1× (EH + IH + ExH + LH)×AH + 0.2×(EUL + IUL + ExUL + LUL)× AUL + 0.3× (ET + IT + ExT + LT)× AT + 0.4× (ELL + ILL + ExLL + LLL)× ALL (19, 20).
Dermatology Life Quality Index
The Dermatology Life Quality Index (DLQI) scale was developed by Finlay and Khan in 1994 and is currently the most frequently used instrument for assessing the quality of life in patients with dermatologic conditions (21). Each question of this scale has four options: “not at all”, “a little”, “a lot”, or “very much”, which correspond to scores of 0, 1, 2, and 3, respectively. A response of “not relevant” is scored as “0”. The DLQI score is computed by summing the scores for each question, ranging from a minimum of 0 to a maximum of 30 points.
Statistical analysis
For this analysis, epidemiological data, clinical data, itch-related data, severity of AD, and the quality of life of the patients were summarised using descriptive statistics. Continuous variables, such as age, were expressed as mean ± standard deviation. Categorical variables were assessed based on the number of patients and the percentage within respective categories of the dataset. Spearman’s correlation was used to evaluate the association between the analysed average and maximum itch intensities and the EASI and DLQI scores. After analysing the differences in sex, age, educational level, age at first onset, and family history of AD using one-way analysis of variance with EASI and DLQI scores as dependent variables, a multivariate analysis of significant correlations was performed using a generalized linear model. The proportions of patients who experienced itching and the most itchy at different times were compared using Cochran’s Q. Significance values have been adjusted by Bonferroni correction for multiple testing. A two-sided p < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS (version 25.0; IBM Corp, Armonk, NY, USA).
RESULTS
Participant characteristics
Among the 241 adults included in this study, 134 (55.60%) were females and 107 (44.40%) were males. The mean age was 44.89 ± 19.61 years (median age 40 years [18 to 87]). Education levels included 35 (14.52%) primary school and below, 48 (19.92%) junior high school, 60 (24.90%) senior high school, and 98 (40.66%) college and postgraduate. A total of 10 (4.15%) patients had a first onset age between 0 and 2 years, and 12 (4.98%) had a first onset age between 3 and 12 years. Furthermore, 180 (74.69%) patients had a first onset between 3 and 60 years of age and 39 (16.18%) had their first onset at ages greater than 60 years. Some 120 (49.79%) patients had a family history of atopy (Table I). We found significant differences in the EASI by sex (p = 0.004) and family history (p = 0.007) (Table I). Most patients experienced their first itch mainly on the trunk (34.02%), followed by the lower (29.88%) and upper limbs (21.16%), face (15.35%), hands (14.52%), neck (12.86%), feet (7.47%), head (4.98%), and ears (3.32%); No patients experienced their first itch on the perineum (Fig. 1).
| Variables | DLQI p |
EASI p |
|
| Sex, n (%) | 0.638 | 0.004* | |
| Male | 107 (44.40) | ||
| Female | 134 (55.60) | ||
| Age, years, mean ± SD | 44.89 ± 19.61 | 0.404 | 0.051 |
| Education level, n (%) | 0.561 | 0.643 | |
| Primary and below | 35 (14.52) | ||
| Junior high school | 48 (19.92) | ||
| High school | 60 (24.90) | ||
| College and above | 98 (40.66) | ||
| Age at first onset, n (%) | 0.347 | 0.108 | |
| 0–2 | 10 (4.15) | ||
| 3–12 | 12 (4.98) | ||
| 13–60 | 180 (74.69) | ||
| >60 | 39 (16.18) | ||
| Family history, n (%) | 0.819 | 0.007* | |
| Yes | 120 (49.79) | ||
| No | 121 (50.21) | ||
| SD: standard deviation. *Statistical significance level at p < 0.05. | |||
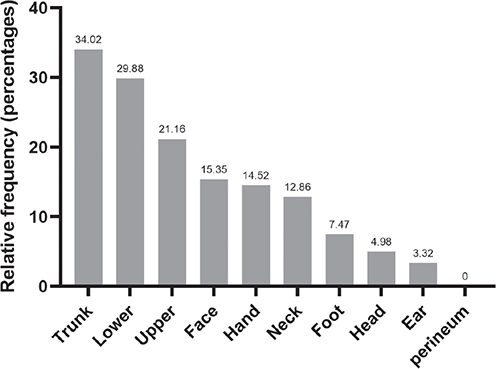
Fig. 1. Body distribution of pruritus associated with atopic dermatitis (AD): percentage of patients with AD experiencing itching in different areas of the body.
Circadian rhythm of itch
Patients were found to experience itchiness at any time of the day. Notably, a significant percentage of patients (74.69%) felt itchy between the hours of 20:00 and 00:00, 44.40% between 00:00 and 04:00, 25.31% between 04:00 and 08:00, 53.11% between 08:00 and 12:00, 58.51% between 12:00 and 16:00, and 61.00% between 16:00 and 20:00 (Fig. 2A). The highest percentage of patients (62.66%) experienced the maximum itch intensity between 20:00 and 00:00, 39.42% of patients felt the maximum itch intensity between the hours of 00:00 and 04:00, 12.86% between 04:00–08:00, 19.09% between 08:00–12:00, 28.22% between 12:00–16:00, and 32.37% between 16:00–20:00 (Fig. 2B). The Cochran Q test showed that the proportions of patients who experienced itching and the most itchy at different time periods both differed significantly (Q = 169.32, Q = 75.85, respectively; p < 0.05). Further analysis of multiple comparisons showed that the proportion of patients who experienced itchy was significantly higher at 20:00–00:00 than at other time periods (p < 0.05), and the proportion of patients who experienced itchy was significantly lower at 00:00–04:00 than at other time periods (p < 0.05) (Fig. 2A). The proportion of patients who experienced the most itchy was significantly higher at 20:00–00:00 than at other time periods (p < 0.05) (Fig. 2B).
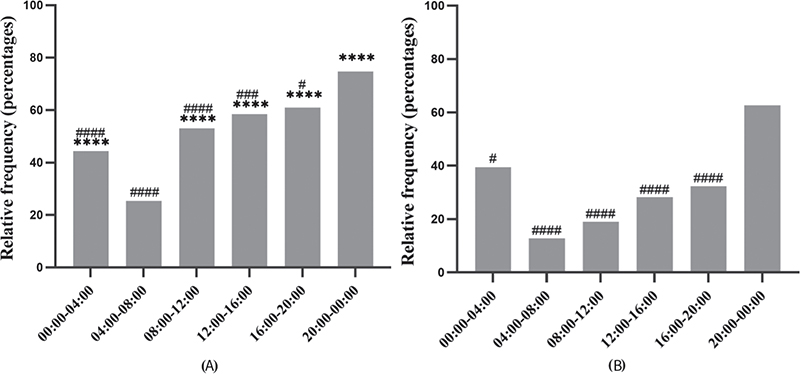
Fig. 2. (A) Time period during which the patient experiences itching; (B) time period during which the patient experiences maximum itching. ****p < 0.0001 vs 04:00–08:00, #p < 0.05, ###p < 0.001, ####p < 0.0001 vs 20:00–00:00.
The above trends showed that adult patients with AD may experience itchiness at any time of the day. However, notably, the highest number of patients reporting itching with the maximum itch intensity within the 20:00–00:00 time period.
The average and maximum itch intensity scores were 5.48 ± 1.69 and 7.09 ± 1.70, respectively. The EASI was significantly and positively correlated with the average (r = 0.539, p < 0.001) and maximum itch intensities (r = 0.517, p < 0.001, whereas the DLQI was significantly and positively correlated with the average (r = 0.582, p < 0.001) and maximum itch intensities (r = 0.533, p < 0.001) (Table II). Males (B = 0.285, 95% CI: 0.094 to 0.476, p = 0.003), family history (B = 0.287, 95% CI: 0.096 to 0.478, p = 0.003) and average itch intensity (B = 0.204, 95% CI: 0.096 to 0.313, p < 0.001) were associated with EASI scores (Table III). The average itch intensity (B = 0.179, 95% CI: 0.112 to 0.246, p < 0.001) was associated with DLQI scores (Table IV).
| DLQIa | EASIb | |||
| r | p | r | p | |
| Average itch intensityc | 0.582 | <0.001* | 0.539 | <0.001* |
| Maximum itch intensityd | 0.533 | <0.001* | 0.517 | <0.001* |
| aTotal scores range from 0 to 30, with higher scores indicating poorer quality of life. The DLQI was 10.62 ± 5.38. bTotal scores range from 0 to 72, with higher scores indicating more severe conditions. The EASI was 9.40 ± 10.11. cTotal scores ranged from 0 to 10, with higher scores indicating greater itching. The average itch intensity was 5.48 ± 1.69. dTotal scores ranged from 0 to 10, with higher scores indicating greater itching. The maximum itch intensity was 7.09 ± 1.70. *Statistical significance level at p < 0.05. |
||||
| Parameter | B | SE | 95% CI | Wald χ² | p |
| (Intercept) | 0.156 | 0.224 | -0.283,0.595 | 0.483 | 0.487 |
| Male | 0.285 | 0.097 | 0.094,0.476 | 8.557 | 0.003* |
| Female | – | – | – | – | |
| Family history (YES) | 0.287 | 0.097 | 0.096,0.478 | 8.677 | 0.003* |
| Family history (NO) | – | – | – | – | |
| Average itch intensity | 0.204 | 0.055 | 0.096,0.313 | 13.753 | <0.001* |
| Maximum itch intensity | 0.078 | 0.057 | -0.035,0.190 | 1.837 | 0.175 |
| SE: standard error; CI: confidence interval. *Statistical significance level at p < 0.05. | |||||
| Parameter | B | SE | 95% CI | Wald χ² | p |
| (Intercept) | 1.332 | 0.128 | 1.081, 1.583 | 108.386 | <0.001 |
| Average itch intensity | 0.179 | 0.034 | 0.112, 0.246 | 27.751 | <0.001* |
| Maximum itch intensity | <0.001 | 0.034 | –0.065, 0.066 | <0.001 | 0.990 |
| SE: standard error; CI: confidence interval. *Statistical significance level at p < 0.05. | |||||
DISCUSSION
The results of this study showed that itching in patients with AD follows a typical circadian rhythm. Most patients felt the most frequent and the most severe itch during the 20:00–00:00 time period, whereas the least number of patients felt itching during the 04:00–08:00 period. The EASI and DLQI of patients with AD correlated with the average and maximum itch intensities. In addition, this study found that males, family history and average itch intensity were all significantly correlated with EASI scores. It suggests that we need to consider the impact of gender, genetic factors and itch symptoms on disease when assessing and treating AD. At the same time, the average itch intensity was also significantly correlated with the DLQI scores, indicating that itch symptoms not only affect the patient’s condition, but may also have a significant impact on their quality of life. Therefore, future research and clinical practice should focus on these factors and explore more effective treatment strategies to comprehensively improve patients’ condition and quality of life.
The incidence of scratching is lower during orthodox deep sleep (22, 23). Ebata et al. found in a videotaped study of nighttime scratching that patients with AD experienced itching leading to scratching more in the first half of the night than in two-thirds of the second half of the night (24). A questionnaire by Yosipovitch et al. showed that 65% of patients with AD had frequent itching during the night, and only 20% reported a high frequency of itching during the morning (12). The results of our study are consistent with those of the above studies, showing that itching increases at night in patients with AD. In previous studies, instrument tests (such as video or bracelet monitors) and questionnaires have been widely used to evaluate itching. Instrument tests can reflect itch more objectively and directly, but the operation is complicated and time-consuming, which is not suitable for large-scale investigation. In contrast, the questionnaire has the advantages of low cost, simple operation, and easy implementation, and is more suitable for large-scale investigation. For specific populations with limited communication abilities, such as paediatric patients with AD, instrumental tests may be a more appropriate choice, while, for adult AD patients who can communicate effectively, questionnaire survey is more efficient and convenient (12, 24). In contrast to previous questionnaire studies, our research focused uniquely on the 24-h itch pattern in adult patients with AD. Previous studies have generally focused on night-time itching and not on specific time periods that extend the analysis throughout the day. By examining the complete circadian cycle, we uncovered a more accurate and comprehensive depiction of itch patterns in AD, which may have significant implications in the management and treatment of the disease. The circadian rhythm of itch that we identified indicates that there are peak times during which patients are more susceptible to itching. These findings may lead to targeted timing of interventions and medication dosing to provide maximum relief when patients are most affected.
Despite recent significant improvements in the understanding of AD and itching, no effective clinical treatments have been found to control itching. The treatment of AD remains challenging and presents an urgent need for new, effective, safe, and targeted therapies. Our findings and further studies may lead to optimized options for clinical pharmacotherapy, such as chronotherapy, which has been validated for its effectiveness and is commonly used in other atopic disorders (e.g., nocturnal asthma) (25, 26). Chronotherapy improves the efficacy and decreases the side effects of existing medications and reduces the financial burden on the patient (13, 14, 27). Notably, our study population was recruited from a single hospital; therefore, the circadian rhythm of itching found in our study may be more pronounced than that reported in studies involving multiple settings. We must consider the issue of recall bias, which arises when participants rely on their memories to report their itching experiences. Memories are often subjective and can be influenced by various factors, such as the passage of time or emotional associations. This can lead to inaccuracies in the reported timing and intensity of itching symptoms. Therefore, in order to reduce the recall bias of time period, we set the time period to a wider 4-hour interval in order to reduce the recall bias of itchy intensity. Subsequent studies are required in which the time period is shortened to elucidate the temporal pattern of itching more precisely.
Consistent with the results of other studies, we found that the EASI and DLQI were associated with itch intensity in patients with AD, with higher intensity of itching associated with higher AD severity and lower quality of life (4, 28, 29). Therefore, controlling itching may reduce the severity of AD and improve quality of life. In our study of adult patients with AD, we found that males had higher EASI scores than females, which may be related to gender-specific behaviours and lifestyles. Our study also revealed that the EASI scores were higher in patients with a family history of atopy than the scores of patients without a family history of atopy. Therefore, when treating patients with a family history of atopic disease, clinicians must consider the family history and characteristics of the patient’s current disease process. In addition, the immediate family members of patients with AD should be encouraged to perform basic skin moisturization and avoid skin irritants as preventative measures.
In conclusion, our study demonstrated that itch in patients with AD follows a circadian rhythm. The time period of 20:00–00:00 had the highest frequency of itching and the most severe itching, whereas the period of 04:00–08:00 had the lowest itch frequency. In addition, our study also demonstrated a correlation between EASI and DLQI scores and itching, and identified male and atopic family history as key factors influencing EASI scores. Our study and further studies may lead to the development of novel, personalized, and targeted temporal therapy strategies for the treatment of itching in patients with AD, reducing the severity of the disease and improving the quality of life of patients.
ACKNOWLEDGEMENTS
This work was supported by grants from the National Natural Science Foundation (82273508), Natural Science Foundation of Hunan Province (2023JJ30821), and Natural Science Foundation of Changsha(kq2208358).
This study was approved by the Third Xiangya Hospital of Central South University (Changsha, China) ethics committee (approval number: Fast 23345).
REFERENCES
- Laughter MR, Maymone MBC, Mashayekhi S, Arents BWM, Karimkhani C, Langan SM, et al. The global burden of atopic dermatitis: lessons from the Global Burden of Disease Study 1990-2017. Br J Dermatol 2021; 184: 304–309. https://doi.org/10.1111/bjd.19580
- Deckers IA, McLean S, Linssen S, Mommers M, van Schayck CP, Sheikh A. Investigating international time trends in the incidence and prevalence of atopic eczema 1990-2010: a systematic review of epidemiological studies. PLoS One 2012; 7: e39803. https://doi.org/10.1371/journal.pone.0039803
- Ishiuji Y. Addiction and the itch-scratch cycle. What do they have in common? Exp Dermatol 2019; 28: 1448–1454. https://doi.org/10.1111/exd.14029
- Sugiyama A, Murakami Y, Okamoto K, Nakano H, Wakatsuki M, Kawano T, et al. Nocturnal scratching and quality of sleep in children with atopic dermatitis. Acta Derm Venereol 2023; 103: adv12345. https://doi.org/10.2340/actadv.v103.12345
- Lei D, Yousaf M, Janmohamed SR, Vakharia PP, Chopra R, Chavda R, et al. Validation of four single-item patient-reported assessments of sleep in adult atopic dermatitis patients. Ann Allergy Asthma Immunol 2020; 124: 261–266. https://doi.org/10.1016/j.anai.2019.12.002
- Bumgarner JR, Walker WH 2nd, Nelson RJ. Circadian rhythms and pain. Neurosci Biobehav Rev 2021; 129: 296–306. https://doi.org/10.1016/j.neubiorev.2021.08.004
- Duan J, Greenberg EN, Karri SS, Andersen B. The circadian clock and diseases of the skin. FEBS Lett 2021; 595: 2413–2436. https://doi.org/10.1002/1873-3468.14192
- Le Fur I, Reinberg A, Lopez S, Morizot F, Mechkouri M, Tschachler E. Analysis of circadian and ultradian rhythms of skin surface properties of face and forearm of healthy women. J Invest Dermatol 2001; 117: 718–724. https://doi.org/10.1046/j.0022-202x.2001.01433.x
- Salazar A, von Hagen J. Circadian oscillations in skin and their interconnection with the cycle of life. Int J Mol Sci 2023; 24: 5635. https://doi.org/10.3390/ijms24065635
- Yosipovitch G, Xiong GL, Haus E, Sackett-Lundeen L, Ashkenazi I, Maibach HI. Time-dependent variations of the skin barrier function in humans: transepidermal water loss, stratum corneum hydration, skin surface pH, and skin temperature. J Invest Dermatol 1998; 110: 20–23. https://doi.org/10.1046/j.1523-1747.1998.00069.x
- Dawn A, Papoiu AD, Chan YH, Rapp SR, Rassette N, Yosipovitch G. Itch characteristics in atopic dermatitis: results of a web-based questionnaire. Br J Dermatol 2009; 160: 642–644. https://doi.org/10.1111/j.1365-2133.2008.08941.x
- Yosipovitch G, Goon AT, Wee J, Chan YH, Zucker I, Goh CL. Itch characteristics in Chinese patients with atopic dermatitis using a new questionnaire for the assessment of pruritus. Int J Dermatol 2002; 41: 212–216. https://doi.org/10.1046/j.1365-4362.2002.01460.x
- Lee Y, Field JM, Sehgal A. Circadian rhythms, disease and chronotherapy. J Biol Rhythms 2021; 36: 503–531. https://doi.org/10.1177/07487304211044301
- Rogers VE, Mowbray C, Rahmaty Z, Hinds PS. A morning bright light therapy intervention to improve circadian health in adolescent cancer survivors: methods and preliminary feasibility. J Pediatr Oncol Nurs 2021; 38: 70–81. https://doi.org/10.1177/1043454220975457
- Yoshioka D, Ando H, Ushijima K, Kumazaki M, Fujimura A. Chronotherapy of maxacalcitol on skin inflammation induced by topical 12-O-tetradecanoylphorbol-13-acetate in mice. Chronobiol Int 2018; 35: 1269–1280. https://doi.org/10.1080/07420528.2018.1474890
- Hanifin JM R G. Diagnostic features of atopic dermatitis. Acta Derm Venereol 1980; Suppl 92: 44–47. https://doi.org/10.2340/00015555924447
- Hiramoto K, Orita K, Yamate Y, Kasahara E, Yokoyama S, Sato EF. The clock genes are involved in the deterioration of atopic dermatitis after day-and-night reversed physical stress in NC/Nga mice. Open Biochem J 2018; 12: 87–102. https://doi.org/10.2174/1874091X01812010087
- Pariollaud M, Ibrahim LH, Irizarry E, Mello RM, Chan AB, Altman BJ, et al. Circadian disruption enhances HSF1 signaling and tumorigenesis in Kras-driven lung cancer. Sci Adv 2022; 8: eabo1123. https://doi.org/10.1126/sciadv.abo1123
- Hanifin JM, Thurston M, Omoto M, Cherill R, Tofte SJ, Graeber M. The eczema area and severity index (EASI): assessment of reliability in atopic dermatitis. EASI Evaluator Group. Exp Dermatol 2001; 10: 11–18. https://doi.org/10.1034/j.1600-0625.2001.100102.x
- Rullo VE, Segato A, Kirsh A, Sole D. Severity scoring of atopic dermatitis: a comparison of two scoring systems. Allergol Immunopathol (Madr) 2008; 36: 205–211. https://doi.org/10.1016/S0301-0546(08)72551-5
- Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI): a simple practical measure for routine clinical use. Clin Exp Dermatol 1994; 19: 210–216. https://doi.org/10.1111/j.1365-2230.1994.tb01167.x
- Aoki T, Kushimoto H, Hishikawa Y, Savin JA. Nocturnal scratching and its relationship to the disturbed sleep of itchy subjects. Clin Exp Dermatol 1991; 16: 268–272. https://doi.org/10.1111/j.1365-2230.1991.tb00372.x
- Savin JA, Paterson WD, Oswald I, Adam K. Further studies of scratching during sleep. Br J Dermatol 1975; 93: 297–302. https://doi.org/10.1111/j.1365-2133.1975.tb06495.x
- Ebata T, Aizawa H, Kamide R, Niimura M. The characteristics of nocturnal scratching in adults with atopic dermatitis. Br J Dermatol 1999; 141: 82–86. https://doi.org/10.1046/j.1365-2133.1999.02924.x
- Smolensky MH, Lemmer B, Reinberg AE. Chronobiology and chronotherapy of allergic rhinitis and bronchial asthma. Adv Drug Deliv Rev 2007; 59: 852–882. https://doi.org/10.1016/j.addr.2007.08.016
- Spörl F, Schellenberg K, Blatt T, Wenck H, Wittern KP, Schrader A, et al. A circadian clock in HaCaT keratinocytes. J Invest Dermatol 2011; 131: 338–348. https://doi.org/10.1038/jid.2010.315
- Zhou Z, Lin Y, Gao L, Yang Z, Wang S, Wu B. Circadian pharmacological effects of berberine on chronic colitis in mice: role of the clock component Rev-erbα. Biochem Pharmacol 2020; 172: 113773. https://doi.org/10.1016/j.bcp.2019.113773
- Huet F, Faffa MS, Poizeau F, Merhand S, Misery L, Brenaut E. Characteristics of pruritus in relation to self-assessed severity of atopic dermatitis. Acta Derm Venereol 2019; 99: 279–283. https://doi.org/10.2340/00015555-3053
- Weisshaar E, Bentz P, Apfelbacher C, Haufe E, Heinrich L, Heratizadeh A, et al. Itching in atopic dermatitis: patient- and physician-reported outcomes in the German Atopic Dermatitis Registry TREATgermany. Acta Derm Venereol 2023; 103: adv00854. https://doi.org/10.2340/actadv.v103.4426