ORIGINAL REPORT
Exploring Patients’ Perceptions of One-step Surgery for Primary Cutaneous Melanoma: A Qualitative Study
Margueritte LIM1, Thibault KERVARREC2, Youssef MOURTADA1, Laura CHAPUT1, Jean-Pierre LEBEAU3 and Laurent MACHET1,4
1Department of Dermatology, 2Department of Pathology, CHRU Tours, 3Department of General Practice, CHRU Tours, Faculty of Medicine, University of Tours, EA7505 Education Ethics and Health, and 4Faculty of Medicine, University of Tours, UMR Inserm U1253, Tours, France
Abstract
High-frequency ultrasonography (> 20 MHz) has allowed for preoperative measurement of melanoma thickness and thus a one-step surgery strategy. The potential benefits of one-step surgery to patients remain unexplored. From June 2022 to August 2023, 2 dermatologists conducted semi-structured individual interviews with patients who had undergone HFUS examination allowing the choice for one-step surgery (group A) and with patients who had had standard two-step surgery (group B). Analysis of interviews with 21 patients (age range 31–81 years) revealed 5 main themes: (a) understanding the diagnosis, highlighting the significance of clear and comprehensive medical explanations; (b) personal factors considered in treatment decisions, including preferences for minimizing surgical procedures; (c) making choices, bearing responsibility, thus showcasing different levels of patient involvement in decision-making; (d) high-frequency ultrasonography reassurance emphasizing the role of medical reassurance, and (e) patient satisfaction, discussing surgical outcomes and the decision-making process. The majority of participants expressed a clear preference for one-step surgery, perceived as a pragmatic and fast surgical strategy while minimizing interventions. In conclusion, the results emphasize the importance of patient-centred care. These insights can guide improved preoperative consultations and enhance shared decision-making between healthcare professionals and patients regarding melanoma treatment strategies.
SIGNIFICANCE
The standard treatment of cutaneous melanoma is two-step surgery: (i) an initial excision to measure the tumour thickness under a microscope and then (ii) a 1- or 2-cm excision around the initial scar, according to the tumour thickness. High-frequency ultrasonography, by accurately measuring the thickness before surgery, allows for a one-step procedure. No previous research has looked at the potential benefits for patients opting for one-step surgery. We interviewed 21 patients who had undergone one- or two-step surgery. Ultrasonography provided medical reassurance, and most patients preferred one-step surgery, which was perceived as a pragmatic strategy that minimized intervention. Those who did not have a choice between the 2 strategies were satisfied with the two-step procedure but would have preferred the one-step procedure if given the option.
Key words: cutaneous malignant melanoma; patient outcome assessment; qualitative research; shared decision making; ultrasound imaging.
Citation: Acta Derm Venereol 2024; 104: adv40064. DOI: https://doi.org/10.2340/actadv.v104.40064.
Copyright: © 2024 The Author(s). Published by MJS Publishing, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/).
Submitted: Feb 7, 2024. Accepted after revision: Aug 5, 2024; Published: Sep 24, 2024
Corr: Pr. Laurent Machet, Department of Dermatology, CHRU Tours, FR-37044 Tours cedex 09, France. E-mail: machet@univ-tours.fr
Competing interests and funding: The authors have no conflicts of interest to declare.
INTRODUCTION
One-step surgery for melanoma is a novel approach that aims to combine diagnosis and treatment, with appropriate surgical margins based on the measured tumour thickness, in a single surgical intervention. When melanoma is suspected, surgical excision with a 1- to 3-mm margin is recommended according to standard practice (1). Re-excision with or without sentinel lymph node biopsy is guided by the Breslow thickness. Following the French Society of Dermatology (2) and American Academy of Dermatology (3) recommendations, the safety margins are 5 mm for in situ melanoma, 1 to 2 cm for Breslow thickness > 1 mm or in situ melanoma on the face, and 2 cm for Breslow thickness > 2 mm. The updated 2022 European recommendations are similar: 5 mm for in situ melanoma, 1 cm for thickness ≤ 2 mm, and 2 cm for thickness > 2 mm (1). Sometimes an incisional partial skin biopsy may be necessary to confirm the diagnosis when the melanoma is extensive. However, estimating Breslow thickness based on the biopsy may be inaccurate, especially if the thickest part of the tumour is not sampled.
High-frequency ultrasonography (HFUS), with a probe > 20 MHz, allows for measuring the maximal thickness of primary cutaneous melanoma tumours and shows good correlation with the Breslow thickness measured on histological slides (4–15). Therefore, HFUS could accurately guide surgical planning and be a valid option for one-step surgery (10–18). We have routinely offered one-step surgery guided by HFUS to patients, with low risk of excessive excision or inadequate excision requiring a second excision (17).
It has been suggested that 80% of melanoma patients wanted an active role in treatment decisions (19). Shared decision-making in this situation is deemed appropriate, as patients’ preferences are sought in the context of multiple existing options (20). However, to our knowledge, no study has addressed the potential benefits for melanoma patients choosing one-step versus two-step surgery (excisional biopsy followed by re-excision). The main objective of this study was to explore patients’ perceptions and experiences in deciding between one-step and two-step surgery for melanoma treatment: how patients weighed the 2 options as well as their preferences and factors influencing their decision-making process. We aimed to gain an understanding of patients’ perceptions to improve preoperative consultation and facilitate shared decision-making between physicians and patients regarding the surgical treatment of melanoma.
PATIENTS AND METHODS
Study design
This was an exploratory qualitative study involving individual semi-structured interviews. It was conducted in accordance with the Standards for Reporting Qualitative Research recommendations (21).
Study setting and selection of participants
Participants were referred or directly recruited at the University Hospital Centre of Tours within the dermatology, plastic surgery, and maxillofacial surgery departments. Inclusion criteria were age > 18 years with a sufficiently suspicious lesion or partial biopsy-proven cutaneous melanoma (group A) or previous two-step surgery (group B). Eligible participants were approached by a dermatologist (LM or ML) who discussed the study with them. For group A, during the preoperative consultation, the dermatologist explained that excision could be performed in a single session after HFUS examination of the skin. Surgical margins were guided by sonometric thickness. In the case of a partial biopsy performed before referral, the maximum depth based on histology or HFUS was used to determine the size of surgical margins. The imaging was performed by one of 2 trained operators (LM or YM) with more than 10 years of experience each. Patients could choose between one-step or the standard two-step surgical procedure. During a postoperative consultation, we informed patients in group B about the availability of the HFUS examination and the principle of one-step surgery. We asked them which surgical approach they would have preferred if given the choice.
We interviewed participants after their surgery with a mean number of 39.2 days (range 1–211). None of the patients was known to the interviewer.
We used purposive sampling to achieve maximal variation in sex, age, melanoma location, and time between surgery and interview.
Data collection
Interviews were held between June 2022 and August 2023 by 2 researchers (LM and ML) who were new to qualitative research methods. An interview guide with open-ended questions (Appendix SI) was developed and supervised by a general practitioner experienced in qualitative research (JPL). It was enriched after each interview, whenever new topics or concerns had emerged. Interviews were held in person in a consultation room at Tours hospital, except for 2 patients who were interviewed by telephone and 1 patient at home. Field notes were taken during interviews and non-participants present during interviews were asked to intervene as little as possible.
Data analysis
All interviews were audio-recorded and transcribed verbatim, with deidentified transcripts ensuring confidentiality. Using a general inductive approach to data analysis (22), 2 researchers (LM, ML) independently coded each verbatim line by line. Differences between coders were resolved by discussion, with the arbitration of a third researcher (JPL) if needed. Then codes were organized into main themes and categories were identified. Data saturation was reached when no new codes arose from the interviews, and hence, recruitment was stopped after the 21st participant. Microsoft Word and Excel (Microsoft Corp, Redmond, WA, USA) were used for coding and analysis. Quotations were translated into English for article submission (Appendix SII).
Ethics statement
All participants provided informed consent before study participation.
RESULTS
Study population
Twenty-one patients, divided into groups A (n = 16) and B (n = 5), were interviewed within 7 months of the final diagnosis (Fig. 1). Participant characteristics are listed in Table I. The mean age was 53.7 ± 16.7 years (range 31–81) and the mean interview duration was 21 min (range 9–48).
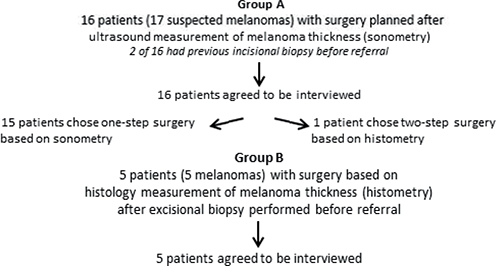
Fig. 1. Flowchart diagram of participants in the study. Flowchart of patients who had surgery after ultrasound measurement of Breslow thickness (group A) and of patients who were interviewed after standard two-step surgery with no previous ultrasound measurement of maximal thickness of the tumour (group B).
Synthesis and interpretation of the data
Five themes emerged from the analysis that provided insight into patients’ experiences and perceptions of one-step surgery: (a) understanding the diagnosis; (b) personal factors considered in treatment decisions; (c) making choices, bearing responsibility; (d) HFUS reassurance; and (e) patient satisfaction.
Understanding the diagnosis
Clear information from healthcare professionals. Participants’ responses revealed varying levels of clarity and comprehension regarding the diagnosis and surgical information provided by the dermatologist. Most participants understood their diagnosis and recalled that their physician suggested one-step surgery as an appropriate treatment. These explanations were generally considered clear and understandable. However, some participants struggled to fully grasp the nuances of their surgical treatment, which resulted in an inability to articulate details, such as margins.
[The physician] explained things well, telling me clearly that it looked like melanoma. It didn’t worry me more than that. It’s removable, so no apprehension. (P06)
It reassured me. When things are clearly stated and explained, there’s no problem making a decision. (P10)
This highlights the participants’ appreciation for being well informed and involved in their own healthcare decisions.
Being aware of cancer risk. The clinical diagnosis was given to the patient during preoperative consultation. Awareness of cancer risk was common, with 5 participants associating their suspicious lesion with a personal or family history of melanoma or other cancer. Perceiving themselves as being at increased risk, these participants had already searched on the Internet or asked relatives about melanoma.
Well, I needed reassurance and to say to myself, I prefer that [large excision], given my dad’s history, to comfort myself and to say to myself “you never know”. (P14)
I suspected it [melanoma]. I suspected it. I’d already even looked it up on the internet.” (P11)
These comments show the participants’ perception of surgery as a protective measure for recovery while minimizing the chances of recurrence or spread.
Personal factors considered in treatment decisions
Patients cited a variety of reasons when deciding to have one- or two-step surgery.
Personal convenience of one-step surgery. All respondents favoured one-step surgery due to aversion to multiple surgeries and the convenience of faster recovery. They also noted the benefits of fewer hospital visits, which saves work and travel time, especially for patients who live far from the hospital. One patient also expressed a fear of needles.
What’s more, by only doing it once, I had no apprehensions or preconceived ideas about how it would go. Whereas if you go back a second time, you know what happened to you, and you don’t want to do it again. (P05)
I live far away, so it was also a choice based on distance. (P08)
It was really the phobia of getting a shot. (P09)
Participants appreciated having a choice and being able to decide based on their personal needs, emphasizing the importance of considering personal convenience and minimizing disruptions in patients’ daily lives.
I thought it was good … to have the choice between two solutions, which seemed to be equally safe, but adapting it to my personal needs. (P03)
Choosing two-step surgery: following the guidelines
Only 1 participant in group A (P16) chose the two-step strategy for a suspicious arm lesion, valuing the “safety” of a definite diagnosis and the possibility of a benign diagnosis before proceeding further.
What I really appreciated was being given the choice between 2 solutions…. I listened, and I chose safety, or caution, or safety, it’s all the same. (P16)
This patient valued adhering to established medical procedures. He preferred a careful approach without taking unnecessary risks of a wrong clinical diagnosis and thus excessive surgery.
Making choices, bearing responsibility
This theme implies different levels of patient involvement in the decision-making process.
Different degrees of involvement. Most patients were satisfied that their opinions were considered, and they could choose the surgical strategy, feeling respected. Participants’ autonomy in decision-making was also influenced by their lack of medical knowledge. Some patients did not feel confident in deciding and asked the dermatologist to guide them, highlighting an interest in shared decision-making. Many patients decided by themselves after hearing the medical explanations, occasionally with family member support. Most patients appreciated having the autonomy to make decisions.
I made the decision all by myself. (P08)
Different views on responsibility. Patients were willing to take or at least share responsibility for the final decision. One emphasized the patient’s right and duty to be involved in decisions whenever possible. In contrast, 1 patient stated that she came to the hospital to be guided but was also satisfied with having the choice.
But I think that hospitals are obliged to leave some responsibility to the patient, in so far as the patient can. (P16)
It’s true that having a choice changes things when sometimes we come to be guided. And in the end, it was good to have it too. (P15)
Need to value the trade-offs. When melanoma was clinically uncertain, patients still accepted the risk of an unnecessarily large excision for a benign lesion, preferring wide local excision (WLE) over undergoing an additional surgical procedure if it turned out to be melanoma.
I was able to choose to have a slightly larger scar right away to avoid a second procedure. (P03)
Well, at least we know everything’s off. So, it’s all gone. (P06)
Those who had a lesion on the body said that this decision was not the case for tumours located in visible anatomic regions such as the face, because of the aesthetic impact of a scar.
Beyond the face, of course, but even on the hands, on … well, on a more visible part of the body, I would have made a different decision. (P04)
And as the mole was on my back, I didn’t mind having a slightly larger scar. It’s true that if it had been on another part of my body … I might not have made that choice. (P01)
Two participants (P08, P13) with facial melanoma did not regret choosing one-step surgery. P08 had a partial biopsy that confirmed the diagnosis and gave her the option of 5- or 10-mm margins because the sonography thickness revealed an intra-epidermal lesion. She chose the smaller margins because she was concerned about the potential width of the scar. P13 did not have a prior biopsy, but he easily decided on WLE from the outset given the sonometric thickness of 0.4 mm.
High-frequency ultrasonography reassurance
Reducing anxiety. Patients receive the news of the diagnosis during the same consultation as the HFUS examination and surgical explanations. From clinical diagnosis until the histology results, participants may feel worried and anxious.
And then, yes, we’re always afraid of whether it’s cancerous or what. Because it’s a long wait, we have to wait 3 weeks to find out if the tumour is cancerous or not. (P13)
The fact that you measured it and saw that it wasn’t too thick reassured me. (P15)
Participants found the HFUS examination reassuring because it gave them immediate information concerning the tumour’s depth and thus its prognosis without having to wait for the histology report. They expressed being relieved that the tumour was not too thick and that the physician explained the results. This finding suggests that US examination can be a valuable tool for reducing anxiety.
Reducing the delay in being treated
Most participants felt rushed into having the melanoma removed with WLE for complete treatment. They often reported that HFUS examination allowed the physicians to see in-depth, which justified one-step surgery. They may have been anxious about their diagnosis and wanted to get the surgery over with as soon as possible. They may also have been concerned about the risk of waiting, such as the possibility that the cancer could spread.
But in one-step, you get rid of it. (P06)
One-step surgery is better. It’s over, it’s done. That’s why. (P09)
These comments underline patients’ awareness of the benefits of one-step surgery and a desire for the cancer to be treated as quickly as possible.
Patient satisfaction
Taking results as a judge for a right or wrong decision. This category explored participants’ reactions to histology analysis after surgery. The analysis seemed to influence the perception of their decision. Six patients had an excessive excision from 5 to 10 mm, and 1 (P02) expressed disappointment because of an excessive margin of 5 mm. P12, who underwent both one- and two-step surgery for 2 different lesions, would have preferred one-step surgery for both and felt disappointed that his preference was not understood during the preoperative consultation.
Oh dear, we’ve taken everything off! Oh well, that’s all right…. (P02)
Well, the diagnosis was right in the end; it was the right solution, so I think we made the right choice. (P08)
What counts is the result … without having to intervene a second time. (P10)
Many patients were satisfied with their decision to avoid an additional intervention, even when the final diagnosis was benign. Of the 4 patients in group A with a personal or family history of melanoma, 3 ultimately had a diagnosis of nevi. P04, with a history of melanoma and a painful memory of his first surgical experience, appreciated managing his emotions by choosing the surgical strategy. P07 and P14 opted for WLE because the suspected lesion was in a less visible region (trunk, arm). P14 also had a family history of melanoma in her father and grandfather, and she expressed a fear of the same diagnosis.
Improving communication to achieve satisfaction. Participants were generally satisfied with surgical outcomes, particularly the appearance of the scar, but some were surprised at the width of the scar. However, they would choose the same procedure again. Two patients (P05, P10) with plantar melanoma did not expect a long recovery with limited movement. They felt that the dermatologist did not adequately prepare them for this, which affected their emotional and physical outcomes.
When I first saw this crater, I was impressed! (P10)
I didn’t expect it to take this long at all, and no one can tell me…. So, it’s already been almost 2 months, and I can only walk on tiptoe and I’m in a wheelchair … so nobody said it would take this long. (P05)
Patients felt that the dermatologist should have given them more information regarding what to expect after surgery. The importance of informing patients about postoperative outcomes must be emphasized.
Group B perceptions of one-step surgery
Participants who were not given the opportunity to discuss the one-step surgery option before undergoing WLE were asked what they would do if given the choice between the one-step and two-step procedure. All 5 of these patients replied that they would probably have preferred a one-step strategy because they did not see much difference between the 2 strategies and preferred avoiding additional surgical interventions.
Well, I don’t see the point of doing it twice when you can do it all at once. (P20)
They said that they would trust the physician in either case. However, they acknowledged the difficulty of answering since they had already undergone surgery. Nevertheless, satisfaction with the two-step procedure and overall experience was also noted.
DISCUSSION
To the best of our knowledge, this is the first qualitative study to explore patients’ perceptions and experiences of one-step surgery for primary cutaneous melanoma. The findings provide insights into the various factors affecting patients’ understanding, preferences, emotions, and satisfaction as they go through the diagnosis, decision-making, and postoperative outcomes. Patients expressed an overall positive experience. Twenty of the 21 participants expressed a clear preference for one-step surgery, citing a personal aversion to surgery as the main reason for their preference.
Participants emphasized the critical role of clear and understandable medical explanations of the diagnosis and surgical treatment options in guiding their decision. However, some patients did not fully understand the one-step surgical approach, which underscores the importance of effective communication between healthcare professionals and patients. This finding is consistent with existing research that underlines the importance of patient-centred communication and shared decision-making in promoting informed choices (23). Some participants had a high awareness of their skin cancer risk due to a personal or family history of cancer. These patients were more likely to show interest in one-step surgery rather than standard two-step surgery, probably because of their fear of cancer and desire for rapid treatment. At-risk families have been identified as ambassadors who can provide information to others on melanoma prevention and detection (24).
Regarding patient involvement, few patients adopted a traditional role, relying on healthcare professionals to make treatment decisions on their behalf. However, this approach may inadvertently overlook patient values and preferences, thus resulting in a disconnect between the treatment plan and the patient’s wishes in that the physician may misunderstand (25). Most patients were satisfied with deciding for themselves in a shared decision-making process. This observation aligns with melanoma patients’ wish to be seen as capable and resourceful individuals who can manage information during the diagnostic process and access to care (26). Participants’ choices were influenced by several factors such as the perceived convenience of the procedure, medical reassurance, and the desire to avoid additional surgery. The decision-making differed depending on the tumour location because the aesthetic outcome was a major concern that could affect patients’ social life. Patients reported that they were more likely to undergo two-step surgery for melanoma located on the face to avoid excessive margins. In fact, patients are more satisfied if the scar is small and located away from the centre of the face (27).
The impact of anxiety and uncertainty of a melanoma diagnosis and the decision-making process cannot be underestimated. Patients often experienced these feelings, which were alleviated to some extent by the reassurance provided by the dermatologist with the HFUS examination. These findings underscore the need for better psychological support for patients within their care and the importance of integrating psychology into cancer care to address patients’ emotional challenges (28). Trust in the healthcare professional could have influenced patients’ choice. In fact, several patients mentioned the feeling of trust if they wanted to undergo treatment. Because of limited medical understanding, patients often follow physicians’ instructions. Therefore, patients must be provided with clear, honest, and truthful information regarding the diagnosis and surgical treatment, recognizing that they may be going through an overwhelming experience when receiving the diagnosis during preoperative consultation (29, 30). Beyond counselling, time to think and educational material would help patients learn about their diagnosis and treatment options (31).
Patients’ satisfaction with the surgical outcomes was tied to their overall care experience, including postoperative support and information concerning potential postoperative outcomes. Another qualitative study noted the discrepancy between patients’ expectations of a scar versus their actual postoperative appearance (32), which suggests that the healthcare professional should focus on not only the surgical procedure itself but also the holistic care of the patient.
Strengths and limitations
This study is the first qualitative study to provide an insight into patients’ perceptions of this unexplored topic. Using semi-structured interviews soon after surgery reduced recall bias.
The first limitation is inherent to the qualitative nature of the study in that the results are only exploratory and cannot be widely applied. Second, HFUS is not widely available in all hospitals and requires experienced operators. Therefore, one-step surgery may not be adopted in daily practice in France. However, 13- to 18-MHz US probes are more commonly used in radiological clinical practice and could be used to measure cutaneous melanoma thickness but with lower resolution than HFUS (4, 12, 33, 34). The risks of overestimating Breslow thickness and of false diagnosis of malignancy are the main disadvantages of the one-step surgery. Third, accuracy of sentinel lymph node biopsy (SLNB) might be affected by previous wide surgery. However, this point was previously addressed and 1–2 cm wide surgery did not significantly affect the SLNB positivity rate (35, 36). Fourth, almost all patients did not choose the two-step surgery. Thus, we lacked patients’ experiences of two-step surgery. Therefore, we asked patients who underwent WLE in two-step surgery without preoperative HFUS examination what they would have thought of one-step surgery guided by HFUS sonometry and what choice they would have made. Fifth, the researcher LM may have induced a bias by his experience in the use of HFUS and one-step surgery and could have affected patients’ responses during the preoperative consultation. However, he was also the most experienced to explain the procedure. Finally, almost all histology analyses showed < 1 mm Breslow thickness, which resulted in 10-mm margins and could have been more acceptable to patients than a maximum of 20-mm margins. Also, participants did not check the interview transcripts, which would have supported the validity of the findings.
Clinical implications
The clearest message to emerge from these interviews is the overall satisfaction with one-step surgery, explained by a perception of a pragmatic and fast surgical strategy guided by HFUS, a non-invasive examination, for melanoma. Clear and comprehensible delivery of information can empower patients to make informed decisions that align with their preferences and values to improve their quality of care.
Further research is needed on several aspects. For example, a study on the same topic could investigate perceptions of healthcare professionals (dermatologists, pathologists, surgeons) regarding one-step surgery. A decision support tool could facilitate both physicians and patients in this decision making, similar to the validated patient decision aid for treating lentigo maligna of the head and neck (37). Finally, better understanding patients’ preferences may reduce the cost of public healthcare given the reduced implication of histology analysis, surgeon’s time, travel, and medical leave. Moreover, medico-economic advantages could be further studied.
Conclusions
One-step surgery should be proposed to patients after they are given adequate information. Our study emphasizes the importance of patient-centred care associated with effective patient–physician communication providing informed choices. These insights can guide improved preoperative consultations and enhance shared decision-making between healthcare professionals and patients regarding melanoma treatment strategies. Further research is needed to understand healthcare professionals’ perceptions concerning one-step surgery and to develop decision support tools for optimizing decision-making in melanoma treatment.
ACKNOWLEDGEMENTS
The authors would like to thank all the patients who took the time to participate in this study, and Mrs Laura Smales for editing the manuscript.
IRB approval status: This research was approved by the Ethics Committee in Human Research of the Medical Faculty of Tours (no. 2022 027).
REFERENCES
- Garbe C, Amaral T, Peris K, Hauschild A, Arenberger P, Basset-Seguin N, et al. European consensus-based interdisciplinary guideline for melanoma. Part 2: Treatment - Update 2022. Eur J Cancer 2022; 170: 256-284. https://doi.org/10.1016/j.ejca.2022.04.018
- Guillot B, Dalac S, Denis MG, Dupuy A, Emile JF, De La Fouchardiere A, et al. French updated recommendations in Stage I to III melanoma treatment and management. J Eur Acad Dermatol Venereol 2017; 31: 594-602. https://doi.org/10.1111/jdv.14064
- Swetter SM, Tsao H, Bichakjian CK, Curiel-Lewandrowski C, Elder DE, Gershenwald JE, et al. Guidelines of care for the management of primary cutaneous melanoma. J Am Acad Dermatol 2019; 80: 208-250. https://doi.org/10.1016/j.jaad.2018.08.055
- Fernández Canedo I, de Troya Martín M, Fúnez Liébana R, Rivas Ruiz F, Blanco Eguren G, Blázquez Sánchez N. Preoperative 15-MHz ultrasound assessment of tumor thickness in malignant melanoma. Actas Dermosifiliogr (Engl Ed) 2013; 104: 227-231. https://doi.org/10.1016/j.ad.2012.06.007
- Kaikaris V, Samsanavičius D, Maslauskas K, Rimdeika R, Valiukevičienė S, Makštienė J, et al. Measurement of melanoma thickness - comparison of two methods: ultrasound versus morphology. J Plast Reconstr Aesthet Surg 2011; 64: 796-802. https://doi.org/10.1016/j.bjps.2010.10.008
- Hinz T, Ehler L-K, Voth H, Fortmeier I, Hoeller T, Hornung T, et al. Assessment of tumor thickness in melanocytic skin lesions: comparison of optical coherence tomography, 20-MHz ultrasound and histopathology. Dermatology 2011; 223: 161-168. https://doi.org/10.1159/000332845
- Maj M, Warszawik-Hendzel O, Szymanska E, Walecka I, Rakowska A, Antczak-Marczak M, et al. High frequency ultrasonography: a complementary diagnostic method in evaluation of primary cutaneous melanoma. G Ital Dermatol Venereol 2015; 150: 595-601.
- Crisan M, Crisan D, Sannino G, Lupsor M, Badea R, Amzica F. Ultrasonographic staging of cutaneous malignant tumors: an ultrasonographic depth index. Arch Dermatol Res 2013; 305: 305-313. https://doi.org/10.1007/s00403-013-1321-1
- Botar-Jid CM, Cosgarea R, Bolboacă SD, Şenilă SC, Lenghel LM, Rogojan L, et al. Assessment of cutaneous melanoma by use of very-high-frequency ultrasound and real-time elastography. AJR Am J Roentgenol 2016; 206: 699-704. https://doi.org/10.2214/AJR.15.15182
- Machet L, Belot V, Naouri M, Boka M, Mourtada Y, Giraudeau B, et al. Preoperative measurement of thickness of cutaneous melanoma using high-resolution 20 MHz ultrasound imaging: a monocenter prospective study and systematic review of the literature. Ultrasound Med Biol 2009; 35: 1411-1420. https://doi.org/10.1016/j.ultrasmedbio.2009.03.018
- Meyer N, Lauwers-Cances V, Lourari S, Laurent J, Konstantinou MP, Lagarde JM, et al. High-frequency ultrasonography but not 930-nm optical coherence tomography reliably evaluates melanoma thickness in vivo: a prospective validation study. Br J Dermatol 2014; 171: 799-805. https://doi.org/10.1111/bjd.13129
- Mušič MM, Hertl K, Kadivec M, Pavlović M, Hočevar M. Pre-operative ultrasound with a 12-15 MHz linear probe reliably differentiates between melanoma thicker and thinner than 1 mm. J Eur J Dermatol Venereol 2010; 24: 1105-1108. https://doi.org/10.1111/j.1468-3083.2010.03587.x
- Vilana R, Puig S, Sanchez M, Squarcia M, Lopez A, Castel T, et al. Preoperative assessment of cutaneous melanoma thickness using 10-MHz sonography. AJR Am J Roentgenol 2009; 193: 639-643. https://doi.org/10.2214/AJR.08.1387
- Guitera P, Li LX, Crotty K, Fitzgerald P, Mellenbergh R, Pellacani G, et al. Melanoma histological Breslow thickness predicted by 75-MHz ultrasonography. Br J Dermatol 2008; 159: 364-369. https://doi.org/10.1111/j.1365-2133.2008.08681.x
- Hayashi K, Koga H, Uhara H, Saida T. High-frequency 30-MHz sonography in preoperative assessment of tumor thickness of primary melanoma: usefulness in determination of surgical margin and indication for sentinel lymph node biopsy. Int J Clin Oncol 2009; 14: 426-430. https://doi.org/10.1007/s10147-009-0894-3
- Tchernev G. One step surgery for cutaneous melanoma: “We cannot solve our problems with the same thinking we used when we created them?”. Open Access Maced J Med Sci 2017; 5: 774-776. https://doi.org/10.3889/oamjms.2017.168
- Chaput L, Laurent E, Pare A, Sallot A, Mourtada Y, Ossant F, et al. One-step surgical removal of cutaneous melanoma with surgical margins based on preoperative ultrasound measurement of the thickness of the melanoma. Eur J Dermatol 2018; 28: 202-208. https://doi.org/10.1684/ejd.2018.3298
- Russo-de la Torre F. One-step surgical removal of a cutaneous melanoma: current evidence. Actas Dermosifiliogr (Engl Ed) 2020; 111: 541-544. https://doi.org/10.1016/j.ad.2019.02.019
- Albrecht KJ, Nashan D, Meiss F, Bengel J, Reuter K. Shared decision making in dermato-oncology: preference for involvement of melanoma patients. Melanoma Res 2014; 24: 68-74. https://doi.org/10.1097/CMR.0000000000000030
- Van der Horst DEM, Garvelink MM, Bos WJW, Stiggelbout AM, Pieterse AH. For which decisions is Shared Decision Making considered appropriate? - A systematic review. Patient Educ Couns 2023; 106: 3-16. https://doi.org/10.1016/j.pec.2022.09.015
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014; 89: 1245-1251. https://doi.org/10.1097/ACM.0000000000000388
- Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Evaluation 2006; 27: 237-246. https://doi.org/10.1177/1098214005283748
- Tamirisa NP, Goodwin JS, Kandalam A, Linder SK, Weller S, Turrubiate S, et al. Patient and physician views of shared decision making in cancer. Health Expect 2017; 20: 1248-1253. https://doi.org/10.1111/hex.12564
- Loescher LJ, Crist JD, Siaki LACL. Perceived intra-family melanoma risk communication. Cancer Nurs 2009; 32: 203-210. https://doi.org/10.1097/NCC.0b013e31819ae11c
- Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: patients’ preferences matter. BMJ 2012; 345: e6572. https://doi.org/10.1136/bmj.e6572
- Hultstrand Ahlin C, Hörnsten Å, Coe A-B, Lilja M, Hajdarevic S. Wishing to be perceived as a capable and resourceful person - a qualitative study of melanoma patients’ experiences of the contact and interaction with healthcare professionals. J Clin Nurs 2019; 28: 1223-1232. https://doi.org/10.1111/jocn.14730
- Lee EH, Klassen AF, Lawson JL, Scott AM, Pusic AL. Patient experiences and outcomes following facial skin cancer surgery: a qualitative study. Australas J Dermatol 2016; 57: e100-e104. https://doi.org/10.1111/ajd.12323
- Nuttall P, Fothergill A, Hemington-Gorse SJ, Dobbs TD, Tree JJ. Letter to the Editor: Confronting the psychological challenges of skin cancer: a qualitative study investigating patient’s experience of a skin cancer diagnosis and support received. J Plast Reconstr Aesthet Surg 2023; 83: 301-304. https://doi.org/10.1016/j.bjps.2023.05.041
- Vogel RI, Strayer LG, Ahmed RL, Blaes A, Lazovich D. A qualitative study of quality of life concerns following a melanoma diagnosis. J Skin Cancer 2017; 2017: 2041872. https://doi.org/10.1155/2017/2041872
- Bird J, Coleman P, Danson S. Coping with melanoma-related worry: a qualitative study of the experiences and support needs of patients with malignant melanoma. J Clin Nurs 2015; 24: 937-947. https://doi.org/10.1111/jocn.12758
- Wolner ZJ, Flowers NI, Yushak ML, Chen SC, Yeung H. Exploring the melanoma survivorship experience: a qualitative study. Br J Dermatol 2021; 185: 221-223. https://doi.org/10.1111/bjd.19868
- Stamataki Z, Brunton L, Lorigan P, Green AC, Newton-Bishop J, Molassiotis A. Assessing the impact of diagnosis and the related supportive care needs in patients with cutaneous melanoma. Support Care Cancer 2015; 23: 779-789. https://doi.org/10.1007/s00520-014-2414-x
- Kučinskienė V, Samulėnienė D, Gineikienė A, Raišutis R, Kažys R, Valiukevičienė S. Preoperative assessment of skin tumor thickness and structure using 14-MHz ultrasound. Medicina (Kaunas) 2014; 50: 150-155. https://doi.org/10.1016/j.medici.2014.08.002
- Crisan D, Kastler S, Scharffetter-Kochanek K, Crisan M, Schneider L-A. Ultrasonographic assessment of depth infiltration in melanoma and non-melanoma skin cancer. J Ultrasound Med 2023; 42: 1609-1616. https://doi.org/10.1002/jum.16180
- Leong WL, Ghazarian DM, McCready DR. Previous wide local excision of primary melanoma is not a contraindication for sentinel lymph node biopsy of the trunk and extremity. J Surg Oncol 2003; 82: 143-146. https://doi.org/10.1002/jso.10205
- Gannon CJ, Rousseau DL, Ross MI, Johnson MM, Lee JE, Mansfield PF, et al. Accuracy of lymphatic mapping and sentinel lymph node biopsy after previous wide local excision in patients with primary melanoma. Cancer 2006; 107: 2647-2652. https://doi.org/10.1002/cncr.22320
- Vaidya TS, Bander TS, Musthaq S, Lampley N, Lee EH, Nehal KS, et al. Validation of a patient decision aid for the treatment of lentigo maligna. J Am Acad Dermatol 2021; 84: 1751-1753. https://doi.org/10.1016/j.jaad.2020.10.043