QUIZ SECTION
A Depressed Bluish-black Plaque on the Shoulder: A Quiz
Xiaoting SONG1–4, Jiaxing ZHENG1–5 and Shuxia YANG1–4*
1Department of Dermatology and Venerology, Peking University First Hospital, No. 8, Xishiku Street, Xi Cheng District, Beijing,100034, 2Beijing Key Laboratory of Molecular Diagnosis on Dermatoses, Beijing, 3National Clinical Research Center for Skin and Immune Diseases, Beijing, 4NMPA Key Laboratory for Quality Control and Evaluation of Cosmetics, Beijing, 5Beijing Miyun District Hospital, Beijing, China. *E-mail: yangshuxia@bjmu.edu.cn
Citation: Acta Derm Venereol 2024; 104: adv40415. DOI: https://doi.org/10.2340/actadv.v104.40415.
Copyright: © 2024 The Author(s). Published by MJS Publishing, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/).
Published: Oct 10, 2024
An otherwise healthy man in his thirties presented with a plaque on his right shoulder that had been slowly progressing for 5 years. He did not feel any discomfort, and the skin lesion was found by his family by accident. There was no history of trauma to the area. Physical examination showed an asymptomatic, smooth-surfaced, bluish-black plaque of 2 cm×2 cm with central atrophy on the right shoulder (Fig. 1). Punch biopsy of the skin lesion was performed for histopathological examination with haematoxylin-eosin (H&E) staining, and immunohistochemical studies (Fig. 2).

Fig. 1. Clinical presentation. A well-defined 2 cm×2 cm bluish-black atrophic plaque over the right scapular region.
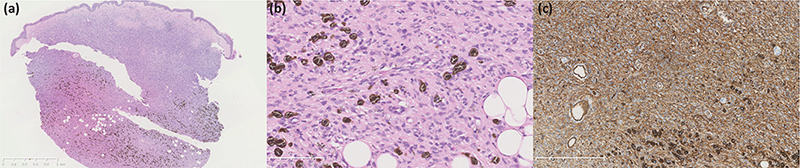
Fig. 2. Histopathological finding. (A) Histologic findings demonstrate infiltration of spindle cells into the deep dermis and subcutaneous tissue (haematoxylin-eosin). Tissue tears exist due to the fragility of tumour tissue, which are non-characteristic. (B) Some of the spindle cells were filled with numerous fine melanin granules, nearly completely obscuring their nuclei (haematoxylin-eosin). (C) Immunohistochemical analysis showed that the spindle cells were strongly positive for CD34.
What is your diagnosis?
Differential diagnosis 1: Morphea
Differential diagnosis 2: Pigmented epithelioid melanocytoma
Differential diagnosis 3: Medallion-like dermal dendrocyte hamartoma
Differential diagnosis 4: Atrophic pigmented dermatofibrosarcoma protuberans
See next page for answer.
ANSWERS TO QUIZ
A Depressed Bluish-black Plaque on the Shoulder: A Commentary
Diagnosis: Atrophic pigmented dermatofibrosarcoma protuberans
Histopathological examination with H&E revealed infiltration of spindle-shaped cells into the reticular dermis and subcutaneous tissue (Fig. 2A), without mitoses. Some of them were filled with numerous fine melanin granules, nearly completely obscuring their nuclei (Fig. 2B). Immunohistochemical analysis showed that the spindle cells were strongly positive for CD34 (Fig. 2C) but negative for S100, SRY-box transcription factor 10 (SOX10), human melanoma black 45 (HMB45), Melan-A and factor XIIIa; the pigment-laden dendritic cells were positive for S100 but negative for CD34.
Dermatofibrosarcoma protuberans (DFSP) is a locally aggressive sarcoma of intermediate malignancy, with a predilection for the shoulder or pelvic region and favouring young to middle-aged adults. It typically manifests as slowly growing, asymptomatic, skin-coloured or violaceous, with firm plaques and nodules. On histopathology with H&E staining, it is characterized by poorly circumscribed, deeply infiltrative spindle cells, arranged in a storiform or fascicular architecture, without substantial cytologic atypia. Both the atrophic and pigmented variants of DFSP are rare. The atrophic variant appears as a depressed plaque rather than typical protuberant nodules, which makes it easily misdiagnosed. It manifests histologically as a dermis-based lesion showing a typical plaque-like growth pattern, with thinning of the dermis (1). Pigmented DFSP, also known as Bednar tumour, is clinically characterized by a bluish-black discoloration and histologically by the presence of CD34+ spindle cells and a varying degree of S100+ melanin-containing dendritic cells. The pigmented cells in the tumour may result from neuroectodermal multidirectional differentiation (2). Atrophic pigmented DFSP shows the characteristics of both atrophic and pigmented variants in the same lesion.
Clinical history and histologic characteristics can help differentiate atrophic pigmented DFSP from other atrophic disorders and melanocyte diseases. Morphea is characterized by erythematous or violaceous plaques, progressing into sclerotic, scar-like tissue and post-inflammatory hyperpigmentation, with homogeneous dense collagen bundles (3). Pigmented epithelioid melanocytoma is a melanocytic tumour of intermediate malignant potential, with a predilection for younger patients. On pathology, it is characterized by spindled and heavily pigmented cells, positive for melanocyte markers, such as S100, SOX10, and HMB45, and negative for CD34 in immunohistochemistry staining (4). Medallion-like dermal dendrocyte hamartoma (MDDH) is clinically characterized by asymptomatic, round, erythematous, and atrophic patches in the thoracic area, usually congenital but sometimes acquired. Histologically, it is featured by an infiltration of CD34+ dermal spindle-cells, which can coexpress factor XIIIa. Although the congenital MDDH may show involvement of deep dermis and adjacent subcutaneous septa, in adult neoplasms invasion is often limited to the superficial dermis. In challenging cases with negative factor XIIIa, fluorescence in situ hybridization analysis (FISH) can be useful to access COL1A1-PDGFB gene rearrangement for confirming DFSP. FISH analysis was not performed in this case. However, the late onset, involvement of subcutaneous tissue, and presence of pigment-laden dendritic cells more likely suggest the diagnosis of DFSP (5).
For resectable DFSP, surgical removal is the first-line treatment, including wide local excision with negative margins and Mohs micrographic surgery (6). Considering the high risk of local recurrence and rare potential to metastasize to the lungs, long-term follow up is necessary. For unresectable, metastatic, or recurrent tumours, radiation modality and targeted therapy with tyrosine kinase inhibitors might be considered as beneficial adjuvant therapies (7). The patient underwent Mohs microscopic surgery, remaining recurrence free at 7 months.
Atrophic pigmented DFSP is often neglected due to the initial indolent behaviour and easily misdiagnosed as cutaneous atrophic disorders and melanocyte diseases. The pathological features of storiform islands of bland spindle cells with diffuse and strong positivity with CD34 are helpful for the diagnosis of DFSP. Owing to local invasion and tendency to recur, prompt treatment and long-term follow-up are warranted.
ACKNOWLEDGEMENT
The authors thank the patient for granting permission to publish this information.
REFERENCES
- Xu S, Zhao L, Wang J. Atrophic dermatofibrosarcoma protuberans: a clinicopathological study of 16 cases. Pathology 2019; 51: 615–620. https://doi.org/10.1016/j.pathol.2019.06.002
- Goncharuk V, Mulvaney M, Carlson JA. Bednár tumor associated with dermal melanocytosis: melanocytic colonization or neuroectodermal multidirectional differentiation? J Cutan Pathol 2003; 30: 147–151. https://doi.org/10.1034/j.1600-0560.2003.00030.x
- Fett NM. Morphea (localized scleroderma). JAMA Dermatol 2013; 149: 1124. https://doi.org/10.1001/jamadermatol.2013.5079
- Moscarella E, Ricci R, Argenziano G, Lallas A, Longo C, Lombardi M, et al. Pigmented epithelioid melanocytoma: clinical, dermoscopic and histopathological features. Br J Dermatol 2016; 174: 1115–1117. https://doi.org/10.1111/bjd.14322
- Kutzner H, Mentzel T, Palmedo G, Hantschke M, Rütten A, Paredes BE, et al. Plaque-like CD34-positive dermal fibroma (“medallion-like dermal dendrocyte hamartoma”): clinicopathologic, immunohistochemical, and molecular analysis of 5 cases emphasizing its distinction from superficial, plaque-like dermatofibrosarcoma protuberans. Am J Surg Pathol 2010; 34: 190–201. https://doi.org/10.1097/PAS.0b013e3181c7cf11
- Acosta AE, Vélez CS. Dermatofibrosarcoma protuberans. Curr Treat Options Oncol 2017; 18: 56. https://doi.org/10.1007/s11864-017-0498-5
- Badhey AK, Tikhtman R, Tang AL. Management of dermatofibrosarcoma protuberans. Curr Opin Otolaryngol Head Neck Surg 2021; 29: 278–282. https://doi.org/10.1097/MOO.0000000000000721