SHORT COMMUNICATION
Improvement of Skin Lesions in an Adult with CHILD Syndrome Treated with 2% Ketoconazole Cream
Michiya OMI, Kana TANAHASHI, Takuya TAKEICHI and Masashi AKIYAMA*
Department of Dermatology, Nagoya University Graduate School of Medicine, Nagoya, Japan. *E-mail: makiyama@med.nagoya-u.ac.jp
Citation: Acta Derm Venereol 2024; 104: adv41929. DOI https://doi.org/10.2340/actadv.v104.41929.
Copyright: 2024 © The Author(s). Published by MJS Publishing, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/).
Submitted: Sep 17, 2024; Accepted after revision: Nov 5, 2024; Published: Nov 20, 2024
Competing interests and funding: The authors have no conflicts to declare.
INTRODUCTION
Congenital hemidysplasia with ichthyosiform erythroderma and limb defects (CHILD syndrome, OMIM: #308050) is an X-linked dominant disorder caused by variants in NAD[P]H steroid dehydrogenase-like protein (NSDHL), resulting in the inhibition of cholesterol synthesis (1). There are no established therapies for the skin lesions. We report an adult CHILD syndrome patient who, to our knowledge, was the first to be treated with topical ketoconazole without recurrence during follow-up.
CASE PRESENTATION
The patient was a 29-year-old Japanese woman. She exhibited scaly, well-demarcated erythema with itching on the left inguinal region and had a history of hair loss on the left parietal area since birth (Fig. 1A). The scaly erythema had recently appeared on her left axilla and left nasal wing (Fig. 1B). Prior to her visit to our hospital, she had undergone excimer light therapy, and had used topical steroids, which had alleviated the itching but had not reduced the affected area or the erythema. She was treated with a topical spray of calcipotriol hydrate and betamethasone dipropionate. This treatment caused pain and worsened the eruption. Her medical history included left face hypoplasia, left hip subluxation, shortening of the left lower extremity, left flatfoot, and aortic stenosis. No significant family history was noted.
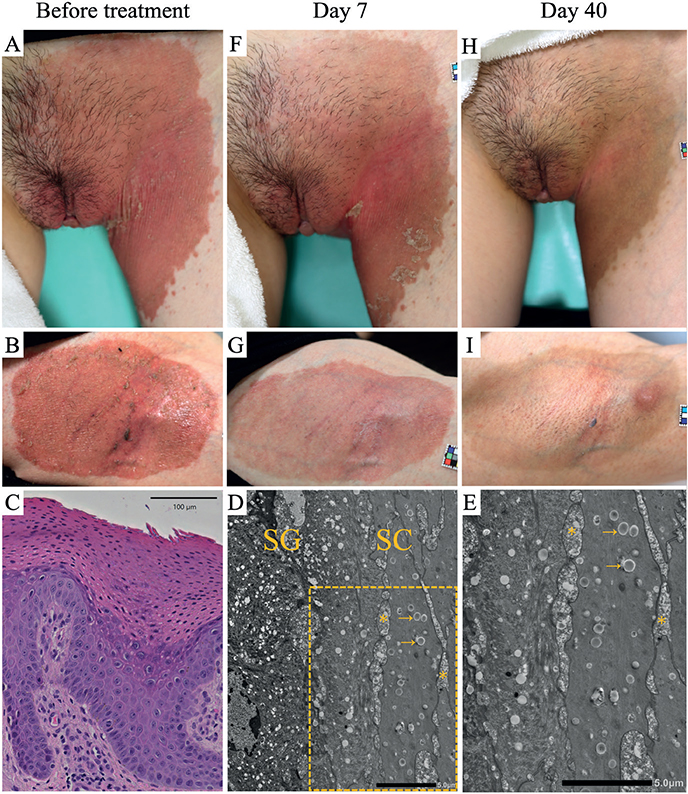
Fig. 1. Clinical course of the skin lesions and the histopathological and ultrastructural features of the present case. (A, B) Clinical photos before treatment with topical ketoconazole show scaly, well-demarcated erythema on the (A) left groin and (B) left axilla. (C) The histopathology of the erythematous lesion on the left groin shows hyperkeratosis and parakeratosis, as well as mild perivascular inflammatory infiltrates in the dermis (haematoxylin–eosin stain, scale bar=100 μm). (D) Ultrastructural features of the stratum granulosum (SG) and stratum corneum (SC) before treatment (bar=5.0 µm). (E) A higher-magnification view of the SC (bar=5.0 µm). A large number of abnormal small vacuoles containing dense materials (arrows) are seen in the cytoplasm of cornified cells. Numerous lipid droplets and vacuoles of various sizes (asterisk) occupy the dilated intercellular spaces, and normal lipid lamellar structures are not observed in the stratum corneum. (F, G) Clinical photos of the skin lesions taken at 7 days of topical ketoconazole therapy. (H, I) Clinical photos at 40 days of therapy show striking improvement of the skin lesions.
Microscopic examinations for fungal infection in the scratched scales of the inguinal region and the left axilla were negative. A skin biopsy from the left inguinal region showed acanthotic epidermis with parakeratosis, hyperkeratosis, and mild perivascular inflammatory infiltrates throughout the dermis (Fig. 1C). The skin specimen of the left inguinal region was stained with ruthenium for transmission electron microscopy (JEM-1400PLUS, JEOL). This revealed many small, abnormal cytoplasmic vacuoles containing dense materials in the cornified cells. In the intercellular spaces of the stratum corneum, a large number of lipid droplets and vacuoles of various sizes were seen, but normal lipid lamellar structures were absent (Fig. 1D, E).
All research was conducted in accordance with the principles of the Declaration of Helsinki after ethical approval was received and written informed consent from the patient was obtained. Whole-exome sequencing of DNA extracted from the peripheral blood showed the patient to have the mono-allelic mutation c.727G > A, p.(Val243Met) in exon 8 of NSDHL. Sanger sequencing confirmed the variant in the patient, but not in either parent. No other pathogenic sequence variants were found in NSDHL. According to standards and guidelines of the American College of Medical Genetics and Genomics (ACMG), the variant was assessed as “likely pathogenic”, satisfying PS2, PM2, and PP4 (2).
Institutional approval was obtained for the off-label use of 2% ketoconazole cream. The pre-treatment Dermatology Life Quality Index (DLQI) score was 3 out of 30. The cream was topically applied twice daily to the left axilla, left inguinal area, and left nasal wing. The itching improved after 2 days of treatment. At 7 days after the start of the treatment, the area of erythema was unchanged, but the desquamation had generally disappeared and the redness of the erythema had improved (Fig. 1F, G).
At 40 days of treatment, the skin lesions had significantly improved, with only minimal pigmentation. The itching at the site of the skin lesions had completely disappeared (Fig. 1H, I). On day 40, the DLQI score was 1. After the remission of symptoms, the patient was treated topically at the affected area twice daily to once every few days with no recurrence of skin symptoms. We followed the patient for a total of 2½ months with no apparent side effects.
DISCUSSION
The phenotypic changes seen in CHILD syndrome are thought to result from the accumulation of toxic metabolites and/or cholesterol deficiency (1). The topical application of lovastatin-cholesterol was reported to resolve the skin symptoms of CHILD syndrome (1). The treatment is a reasonable pathogenesis-based treatment, as statins inhibit HCGMR and cholesterol is a pathway end product of the cholesterol synthesis pathway. There are also 2 reported paediatric cases of CHILD syndrome that were treated with topical 2% ketoconazole, which inhibits CYP51 (3, 4). In the case reported by Liu et al. (3), there was no recurrence after 3 months of topical maintenance treatment and the application was discontinued. Over the next 4 years, signs of recurrence appeared about twice a year in the form of small lesions that cleared within 2 to 4 weeks of topical ketoconazole application (3). Maceda et al. (4) treated their patient with the intermittent application of ketoconazole cream once a day, which resulted in a reduction in waxy scaling, but the symptom recurred after about 5 days. The cases reported by Liu et al. (3) and Maceda et al. (4) were both paediatric. We do not consider the disease nature or pathogenesis to differ between adult patients and paediatric patients. However, it is noteworthy that the chronic skin lesions of the present adult case, which had resulted from the accumulation of toxic metabolites and/or cholesterol deficiency for a long time until adulthood, had significantly improved with only minimal pigmentation. Given the step at which CYP51 acts in the cholesterol synthesis pathway, it is assumed that, unlike statins, ketoconazole does not inhibit the formation of squalene. As squalene is known to have some benefits for the skin as an emollient, antioxidant, and moisturizer, ketoconazole may be more beneficial for the skin than statin ointment (5).
Kallis et al. (6) reported a case of CHILD syndrome with the same NSDHL variant – p.(Val243Met) – as that in the present case, supporting the idea that this missense variant is pathogenic (6). In a 10-month-old girl reported by Kallis et al., a scaly, well-defined, reddish-pink plaque on the right side of the body was improved by topical petroleum-based simvastatin (5%) applied twice daily. Kallis et al. also reported a 50% to 60% improvement in the skin symptoms of the patient after only 5 days of topical simvastatin treatment, showing a therapeutic effect similar to that of the topical ketoconazole cream in our case (6). In addition, Bajawi et al. (7) also reported topical simvastatin monotherapy to be effective for CHILD syndrome.
Thus, our present case suggests that topical ketoconazole cream has comparable efficacy even in longstanding and fully developed skin lesions in an adult patient.
Ketoconazole is commonly used to treat dermatomycoses. As of May 2020, ketoconazole was approved for topical and vaginal use in 117 countries worldwide (information from Janssen Pharmaceutical K.K., data not shown). In countries where topical statins are not available, ketoconazole cream could be an off-label treatment option for CHILD syndrome.
In conclusion, to the best of our knowledge, the present case is the first adult case of CHILD syndrome in which the skin lesions showed improvement with ketoconazole cream. Ketoconazole is a widely accessible, easy-to-handle, safe topical medication that holds promise as a potential treatment for skin symptoms in CHILD syndrome. This case suggests that ketoconazole may be effective not only in paediatric patients, as previously reported, but also in adults with longstanding and fully developed skin lesions. Given the limited number of reports on this treatment approach, further studies including randomized, double-blind, placebo-controlled clinical studies and detailed investigations into the underlying pharmacological mechanisms are warranted.
ACKNOWLEDGEMENTS
The authors would like to thank the patient for her cooperation. They also thank Ms Yuka Terashita for technical assistance in preparing samples for TEM observation and Ms Haruka Ozeki for assistance in Sanger sequencing. The authors would like to thank the Division of Medical Research Engineering at Nagoya University Graduate School of Medicine for allowing them to use their electron microscope. They thank Mr Koji Itakura (Technical Center, Nagoya University) for his technical assistance.
Funding sources: This research was supported by a Health and Labor Sciences Research Grant for Research on Intractable Diseases (23FC1039) from the Ministry of Health, Labor and Welfare of Japan to MA. This work was supported by a JST FOREST Program grant (Number JPMJFR210R) to TT, by JSPS KAKENHI (Grant Number 24K02470) to MA, and by AMED under Grant Number JP23ek0109678 to TT and MA.
REFERENCES
- Paller AS, van Steensel MA, Rodriguez-Martín M, Jennifer S, Candrice H, Debra C, et al. Pathogenesis-based therapy reverses cutaneous abnormalities in an inherited disorder of distal cholesterol metabolism. J Invest Dermatol 2011; 131: 2242–2248. https://doi.org/10.1038/jid.2011.189
- Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 2015; 17: 405–424. https://doi.org/10.1038/gim.2015.30
- Liu T, Qian G, Wang XX, Zhang YG. CHILD syndrome: effective treatment of ichthyosiform naevus with oral and topical ketoconazole. Acta Derm Venereol 2015; 95: 91–92. https://doi.org/10.2340/00015555-1859
- Maceda EBG, Kratz LE, Ramos VME, Abacan MAR. Novel NSDHL gene variant for congenital hemidysplasia with ichthyosiform erythroderma and limb defects (CHILD) syndrome. BMJ Case Rep 2020; 13: e236859. https://doi.org/10.1136/bcr-2020-236859
- Huang ZR, Lin YK, Fang JY. Biological and pharmacological activities of squalene and related compounds: potential uses in cosmetic dermatology. Molecules 2009; 14: 540–554. https://doi.org/10.3390/molecules14010540
- Kallis P, Bisbee E, Garganta C, Schoch JJ. Rapid improvement of skin lesions in CHILD syndrome with topical 5% simvastatin ointment. Pediatr Dermatol 2022; 39: 151–152. https://doi.org/10.1111/pde.14865
- Bajawi SM, Jafarri SA, Buraik MA, Al Attas KM, Hannani HY. Pathogenesis-based therapy: cutaneous abnormalities of CHILD syndrome successfully treated with topical simvastatin monotherapy. JAAD Case Rep 2018; 4: 232–234. https://doi.org/10.1016/j.jdcr.2017.11.019