SHORT COMMUNICATION
Two Cases of Fungal Melanonychia
Yoshihito MIMA1*, Masako YAMAMOTO1, Koichi MAKIMURA2 and Ken IOZUMI1
1Department of Dermatology, Tokyo Metropolitan Police Hospital, 4-22-1 Nakano, Nakano-ku, Tokyo 164-8541, Japan, and 2Teikyo University Institute of Medical Mycology, Tokyo, Japan. *E-mail: yoshihito11.mima@gmail.com
Citation: Acta Derm Venereol 2024; 104: adv42145. DOI: https://doi.org/10.2340/actadv.v104.42145.
Copyright: © 2024 The Author(s). Published by MJS Publishing, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/).
Submitted: Oct 1, 2024; Accepted: Oct 22, 2024; Published: Nov 19, 2024
Competing interests and funding: The authors have no conflicts of interest to declare.
INTRODUCTION
Onychomycosis was initially thought to be predominantly caused by dermatophytes; however, recent research has revealed that onychomycosis caused by non-dermatophytes is also common (1). Onychomycosis usually presents as a white or yellowish turbid nail (2, 3). However, in rare cases, it may present with dark-brown pigmentation, known as fungal melanonychia (4). This is thought to occur because of melanin pigment deposition resulting from phaeohyphomycotic infections such as those from Curvularia sp., Exophiala sp., and Alternaria sp., which contain melanin in their cell walls. However, non-phaeohyphomycotic infections such as those from Aspergillus sp., Trichophyton sp., and Candida sp. can also cause fungal melanonychia (5, 6).
In a systematic review of 133 cases, the causative fungi of melanonychia were found to be Trichophyton rubrum, Neoscytalidium dimidiatum, Candida spp., Aspergillus niger, Fonsecaea pedrosoi, Fusarium solani, Fusarium oxysporum, Exophiala dermatitidis, Wangiella dermatitidis, Botryosphaeria dothidea, Cladosporium spp., Trichophyton interdigitale, Aspergillus alternata, Scytalidium spp., and Sporothrix spp. (6). Among these, T. rubrum is the most frequent (55%), followed by N. dimidiatum (8 %) and C. parapsilosis (7%) (6).
Here, we report 2 cases of fungal melanonychia, one caused by mixed Aspergillus hiratsukae and Trichosporon faecale infection and the other by mixed Exophiala xenobiotica and T. interdigitale.
CASE REPORT
The first case involved a 77-year-old man who presented with black longitudinal pigmentation on the right toenail (Fig. 1A). Microscopic findings from foot desquamation and his toenail revealed pigmented materials and long hyphal elements (Fig. 1B). The patient was diagnosed with onychomycosis and tinea pedis. Fungal culture of the black-coloured nails on potato dextrose agar revealed both white (Fig. S1A) and yellowish (Fig. S1B) colonies. Slide culture microscopy of the white colony revealed fungal hyphae and spore clusters (Fig. S2A). Genetic analysis of the white colony, examining the partial nucleotide sequences of β-tubulin and internal transcribed spacer ribosomal deoxyribonucleic acid (ITSrDNA), identified A. hiratsukae (Table SI). Slide culture microscopy of the yellowish colony revealed fungal hyphae and yeast-like spores (Fig. S2B); genetic analysis targeting ITSrDNA and 28S ribosomal deoxyribonucleic acid (28SrDNA) identified T. faecale (Table SII). Based on these results, the patient was diagnosed with fungal melanonychia, possibly due to combined infection with A. hiratsukae and T. faecale. The minimum inhibitory concentration (MIC) results of different antifungal ointments against A. hiratsukae and T. faecale indicated that efinaconazole was effective against both. After 120 days of treatment with 10% efinaconazole, nail pigmentation greatly improved.
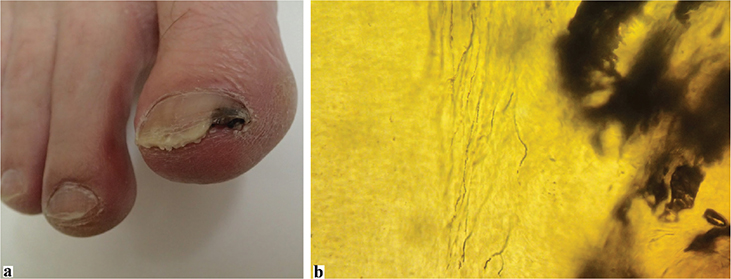
Fig. 1. (A) Clinical photograph: black longitudinal pigmentation on right toenail. (B) Microscopic findings from nail: black pigmented materials and long hyphal elements.
The second case involved a 56-year-old man who presented with dark brown longitudinal pigmentation on the left toenail (Fig. 2). Microscopic examination of foot desquamation and nails revealed pigmented materials and fungal hyphal elements, and he was diagnosed with onychomycosis and tinea pedis. Fungal cultures of the dark-brown nails on Sabouraud dextrose agar identified E. xenobiotica and T. interdigitale. Fungal culture of the pigmented nail on potato dextrose agar revealed a black colony (Fig. S3A); slide culture microscopy revealed fungal hyphae and spores (Fig. S3B), and genetic analysis targeting ITSrDNA and 28SrDNA identified E. xenobiotica (Table SIII). T. interdigitale was not detected by genetic analysis, but was repeatedly identified by fungal culture tests. From this, the patient was diagnosed with fungal melanonychia, possibly due to combined infection with E. xenobiotica and T. interdigitale. The MIC results of various antifungal ointments against E. xenobiotica and T. interdigitale indicated that efinaconazole was effective. After 173 days of 10% efinaconazole treatment, dark-brown nail pigmentation completely resolved.

Fig. 2. Clinical photograph: dark-brown longitudinal pigmentation on left toenail.
DISCUSSION
In these 2 cases, 4 fungi (A. hiratsukae, T. faecale, E. xenobiotica, and T. interdigitale) were found to cause melanonychia. Exophiala sp., Aspergillus sp., and Trichophyton sp. have all been reported to cause fungal melanonychia; however, Trichosporon sp. have never been reported to induce fungal melanonychia. More than 40 cases of Trichophyton sp.-associated fungal melanonychia have been reported, and it is the most common causative fungus. In contrast, Exophiala sp. and Aspergillus sp.-associated fungal melanonychia are rare; to the best of our knowledge, only 3 cases each of Exophiala sp.-associated (7,8) and Aspergillus sp.-associated fungal melanonychia (9, 10) have been reported. A similar case of fungal melanonychia from combined fungal infections has also been reported (10). Only 1 case of fungal melanonychia due to T. interdigitale has been reported (6); however, cases due to E. xenobiotica, A. hiratsukae, or T. faecale, as observed here, have never been reported.
Three types of melanin have been described in human pathogenic fungi: eumelanin, which is formed from dihydroxyphenylalanine (DOPA)-quinones such as L-DOPA; pyomelanin, derived from homogeneous acid produced by tyrosine catabolism; and allomelanins, formed from nitrogen-free precursors such as dihydroxynaphthalene (DHN) (11). Phaeohyphomycosis, such as Exophiala sp., contains melanin in its cell walls that is produced through the L-DOPA melanin, tyrosine catabolism, or DHN pathways (5, 11). Melanin storage characteristics contribute to fungal melanonychia occurrence (11). Non-phaeohyphomycotic infections, such as those from Aspergillus sp. and Trichosporon sp. as observed in our cases, are also thought to produce melanin through these pathways (12, 13). Aspergillus sp. have been reported to produce melanin through the L-DOPA melanin or DHN pathways (12). A. hiratsukae has not been reported to produce melanin pigmentation, but might produce melanin through the same mechanism as other Aspergillus spp. T. faecale produces melanin through the L-DOPA pathway, resulting in a black polyphenolic heteropolymer (13, 14). The mechanism of melanin production in E. xenobiotica has never been discussed; however, T. interdigitale may produce melanin by activating melanocytes, similar to other fungi (6). Consequently, non-phaeohyphomycotic infections, such as those from A. hiratsukae, T. faecale, and T. interdigitale, can cause fungal melanonychia.
Three of the fungi (E. xenobiotica, A. hiratsukae, and T. faecale) in these cases have not been previously reported to cause fungal melanonychia. However, in approximately half of the fungal melanonychia cases, fungal cultures are negative, making accurately identifying causative fungi difficult (6), and a wider variety of fungi may induce melanonychia than previously reported. Here, both patients had confirmed infections with both types of fungi; however, it is unclear whether both were involved in melanin production and melanonychia development. Differential diagnoses of fungal melanonychia include subungual melanoma, subungual haemorrhage, drug-induced pigmentation, endocrine diseases, benign melanocytic lesions, and other cutaneous malignancies such as pigmented squamous cell carcinoma (15). As life-threatening conditions must also be considered in differential diagnosis, other possibilities should be carefully investigated and ruled out when fungal melanonychia is suspected.
REFERENCES
- Gupta AK, Stec N, Summerbell RC, Shear NH, Piguet V, Tosti A, et al. Onychomycosis: a review. J Eur Acad Dermatol Venereol 2020; 34: 1972–1990. https://doi.org/10.1111/jdv.16394
- Gupta AK. Types of onychomycosis. Cutis 2001; 68: 296. https://doi.org/10.1109/35.968814
- Shi D, Lu G, Mei H, de Hoog GS, Zheng H, Liang G, et al. Onychomycosis due to chaetomium globosum with yellowish black discoloration and periungual inflammation. Med Mycol Case Rep 2016; 13: 12–16. https://doi.org/10.1016/j.mmcr.2016.09.001
- Lee DK, Lipner SR. Optimal diagnosis and management of common nail disorders. Ann Med 2022; 54: 694–712. https://doi.org/10.1080/07853890.2022.2044511
- Arcobello JT, Revankar SG. Phaeohyphomycosis. Semin Respir Crit Care Med 2020; 41: 131–140. https://doi.org/10.1055/s-0039-3400957
- Rodríguez-Cerdeira C, Martínez-Herrera E, Cortés-López PN, Guzmán-Montijo E, Sánchez-Cárdenas CD, Arenas R, et al. Fungal melanonychia: a systematic review. Microorganisms 2024; 12: 1096. https://doi.org/10.3390/microorganisms12061096
- Lo Schiavo A, Gambardella A, Caccavale S. Fungal melanonychia and Exophiala dermatitidis. Mycoses 2013; 56: 187–188. https://doi.org/10.1111/j.1439-0507.2012.02217.x
- Hata Y, Naka W, Nishikawa T. [A case of melanonychia caused by Exophiala dermatitidis]. Nihon Ishinkin Gakkai Zasshi 1999; 40: 231–234. https://doi.org/10.3314/jjmm.40.231
- Garcia C, Arenas R, Vasquez del Mercado E. Subungual black onychomycosis and melanonychia striata caused by aspergillus niger. Skinmed 2015; 13: 154–156.
- Lee SW, Kim YC, Kim DK, Yoon TY, Park HJ, Cinn YW. Fungal melanonychia. J Dermatol 2004; 31: 904–909. https://doi.org/10.1111/j.1346-8138.2004.tb00624.x
- Cao W, Zhou X, McCallum NC, Hu Z, Ni QZ, Kapoor U, et al. Unraveling the structure and function of melanin through synthesis. J Am Chem Soc 2021; 143: 2622–2637. https://doi.org/10.1021/jacs.0c12322
- Pal AK, Gajjar DU, Vasavada AR. DOPA and DHN pathway orchestrate melanin synthesis in Aspergillus species. Med Mycol 2014; 52: 10–18. https://doi.org/10.3109/13693786.2013.826879
- Figueiredo-Carvalho MH, dos Santos FB, Nosanchuk JD, Zancope-Oliveira RM, Almeida-Paes R. L-dihydroxyphenylalanine induces melanin production by members of the genus trichosporon. FEMS Yeast Res 2014; 14: 988–991. https://doi.org/10.1111/1567-1364.12174
- de Andrade IB, Araújo GRS, Brito-Santos F, Figueiredo-Carvalho MHG, Zancopé-Oliveira RM, Frases S, et al. Comparative biophysical and ultrastructural analysis of melanins produced by clinical strains of different species from the trichosporonaceae family. Front Microbiol 2022; 13: 876611. https://doi.org/10.3389/fmicb.2022.876611
- Serret CA, Wang S, Marsch A, Hernandez C. Pigmented squamous cell carcinoma presenting as longitudinal melanonychia in a transplant recipient. Cutis 2018; 101: 375–377.