QUIZ SECTION
Plaques and Ulcers of Both Lower Limbs: A Quiz
Qianling ZHANG, Sha LU, Xiqing LI, Liangchun WANG and Jianchi MA*
Department of Dermatology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, 107 Yanjiang Rd W, Guangzhou 510120, China. *E-mail: 425740149@qq.com
Citation: Acta Derm Venereol 2025; 105: adv42510. DOI: https://doi.org/10.2340/actadv.v105.42510.
Copyright: © 2025 The Author(s). Published by MJS Publishing, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/).
Published: Feb 6, 2025.
A female patient, 58 years old, has a history of hypertension. She spent 14 years with ulcers and plaques on the lower limbs (Fig. 1). Initially, the right leg showed only asymptomatic, scattered erythema and plaques. Gradually, both legs developed huge penetrating red plaques with an uneven surface and hard character, as well as visible vascular dilatation and erosion above. Locally, multiple small ulcers and yellow scabs could be seen, the boundary was clear, the edge colour was deepened, and there were no apple-sauce secretion after pressure. Multiple dark red to brown patches were found on the back of the thighs, with clear boundaries, some of them were round, and no obvious scales were seen. There were no symptoms of pain or itching in either lower limb. Following many biopsies in different hospitals, pathology indicated lupus vulgaris and granulomatous alterations. The rash did not improve after immunosuppressant and hormone therapy. The patient had Enterobacter hormaechei infection, according to the results of a bacterial culture performed at our hospital; no abnormalities were found in the results of other regular laboratory tests.

Fig. 1. Plaques and ulcers on the lower legs in a 58-year-old women.
What is your diagnosis?
1. Necrobiosis lipoidica
2. Granuloma annulare
3. Annular sarcoidosis
4. Necrobiotic xanthogranuloma
See next page for answer.
ANSWERS TO QUIZ
Plaques and Ulcers of Both Lower Limbs: A Commentary
Diagnosis: Necrobiotic xanthogranuloma
The middle-aged female patient presented with skin lesions on both lower extremities. Laboratory assessments revealed normal glycosylated haemoglobin levels, and all immune-related tests, including those for lupus antibodies, vasculitis antibodies, and pemphigus antibodies, returned negative results. Histopathological analysis from 2 skin biopsies conducted at our hospital showed epidermal thickening, acanthosis, irregular descent of the epithelial rete ridges, and significant infiltration of multinucleated giant cells throughout the dermis. Additionally, cholesterol crystals (1) were identified within the middle and lower dermis (Fig. 2). Tissue cultures yielded negative results for acid-fast bacilli. Based on clinical findings, a diagnosis of necrobiotic xanthogranuloma (NXG) was established, and the patient underwent a comprehensive treatment regimen for over 11 months, which included tofacitinib at a dosage of 5 mg twice daily, calcitriol capsules at 0.25 mg once daily, and methotrexate at 10 mg weekly. The patient exhibited no new rash, and the pre-existing lesions gradually diminished after 3 months of treatment (Fig. 3). She is currently under ongoing follow-up in our department.
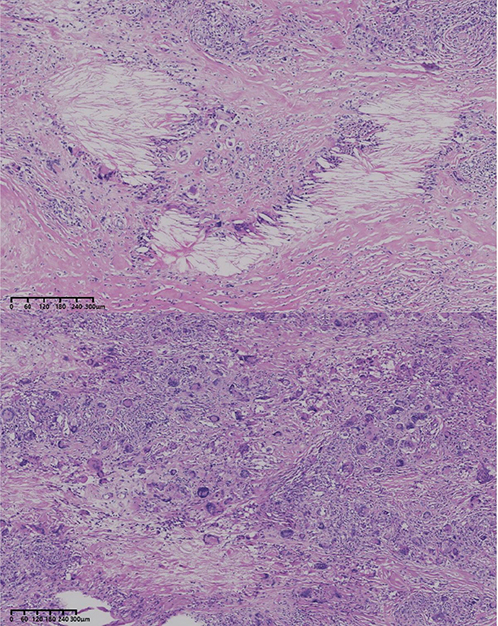
Fig. 2. Histopathological picture of haematoxylin and eosin (H&E) staining from skin biopsies. The picture showed significant infiltration of multinucleated giant cells and cholesterol crystals within the middle and lower dermis. Scale bar: 300 μm.

Fig. 3. Skin lesions after 11 months’ treatment.
NXG, a rare variant of non-Langerhans cell histiocytosis, is characterized by pathological findings that include a ground-glass appearance indicative of progressive necrosis in the dermis and subcutaneous tissues. The condition is distinguished by the infiltration of peripheral histiocytes, foam cells, Touton giant cells, and various other inflammatory cells. Additionally, the presence of cholesterol crystal clefts and lipid vacuoles is noted. Clinically, NXG predominantly affects the elderly population, with skin lesions typically manifesting around the orbital region (2) and, on occasion, on the trunk and extremities. These lesions are characterized by multiple irregular, dark-red plaques and nodules with a light-yellow centre, often exhibiting atrophy, scarring, and telangiectasia on the surface. NXG is frequently associated with multiple myeloma and paraproteinemia (1, 3).
It is common to differentiate NXG from necrobiosis lipoidica (4), actinic granulomas, annular granulomas, and rheumatoid nodules. The clinical manifestations of necrobiosis lipoidica may be confused with the lesions of NXG, particularly when the lesions of the latter are located in the pretibial region. However, histopathological examination of necrobiosis lipoidica typically reveals only necrobiosis, xanthogranulomatous changes, lymphoid follicles, or cholesterol clefts, these being rare. Furthermore, medical history, clinical symptoms of skin lesions, pathological findings, and haematological evaluations can all serve as valuable tools for differentiation.
The pathogenesis of the disease remains poorly understood; however, it has been proposed that elevated serum immunoglobulin levels and lipid accumulation in the dermis and subcutaneous tissue lead to the formation of immune complexes and distinctive inflammatory patterns. A significant correlation exists between NXG and macroglobulinemia (5, 6), with the majority of cases presenting complications associated with this condition. The IgG-κ type is the most prevalent among these cases. Furthermore, NXG is frequently associated with various plasma cell and lymphoproliferative disorders, with some cases potentially progressing to multiple myeloma.
The progression of NXG is typically chronic and may extend over several years; however, certain cases can result in mortality. The prognosis is influenced by the extent of subcutaneous tissue involvement, the presence of visceral malignancies, and the adequacy of wound care in cases where ulceration occurs. Therapies reported both domestically and internationally for the management of NXG include the systemic administration of glucocorticoids, high-dose intravenous immunoglobulin (6–8) (IVIG), antimetabolites (such as methotrexate), alkylating agents (including chlorambucil or thalidomide), and Janus kinase inhibitors (JAKi), all of which have demonstrated varying degrees of efficacy (8–10).
We report a case of NXG affecting both lower limbs. Following 11 months of treatment with methotrexate and tofacitinib, the size and hardness of the plaques significantly decreased. Additionally, the overall appearance of the skin improved, evidenced by a decrease in erythema and atrophy. This case offers valuable insights for the clinical management of the disease.
REFERENCES
- Wood AJ, Wagner MVU, Abbott JJ, Gibson LE. Necrobiotic xanthogranuloma: a review of 17 cases with emphasis on clinical and pathologic correlation. Arch Dermatol 2009; 145: 279–284. https://doi.org/10.1001/archdermatol.2008.583
- Fernández-Herrera J, Pedraz J. Necrobiotic xanthogranuloma. Semin Cutan Med Surg 2007; 26: 108–113. https://doi.org/10.1016/j.sder.2007.02.008
- Nelson CA, Zhong CS, Hashemi DA, Ashchyan HJ, Brown-Joel Z, Noe MH, et al. A multicenter cross-sectional study and systematic review of necrobiotic xanthogranuloma with proposed diagnostic criteria. JAMA Dermatol 2020; 156: 270–279. https://doi.org/10.1001/jamadermatol.2019.4221
- Steinhelfer L, Kühnel T, Jägle H, Mayer S, Karrer S, Haubner F, et al. Systemic therapy of necrobiotic xanthogranuloma: a systematic review. Orphanet J Rare Dis 2022; 17: 132. https://doi.org/10.1186/s13023-022-02291-z
- Sood S, Heung M, Georgakopoulos JR, Mufti A, Prajapati VH, Yeung J. Use of Janus kinase inhibitors for granulomatous dermatoses: a systematic review. J Am Acad Dermatol 2023; 89: 357–359. https://doi.org/10.1016/j.jaad.2023.03.024
- Bijlsma WR, Van Den Bosch WA, Van Daele PLA, Paridaens D. Azathioprine and prednisone combination treatment for adult periocular and orbital xanthogranulomatous disease. Acta Ophthalmol (Copenh) 2011; 89: 278–282. https://doi.org/10.1111/j.1755-3768.2009.01726.x
- Shahriari N. Intravenous immunoglobulin-refractory necrobiotic xanthogranuloma successfully treated with tofacitinib 2% cream. JAAD Case Rep 2022; 32: 41–43. https://doi.org/10.1016/j.jdcr.2022.12.002
- Miguel D, Lukacs J, Illing T, Elsner P. Treatment of necrobiotic xanthogranuloma: a systematic review. J Eur Acad Dermatol Venereol 2017; 31: 221–235. https://doi.org/10.1111/jdv.13786
- Szalat R, Pirault J, Fermand J-P, Carrié A, Saint-Charles F, Olivier M, et al. Physiopathology of necrobiotic xanthogranuloma with monoclonal gammopathy. J Intern Med 2014; 276: 269–284. https://doi.org/10.1111/joim.12195
- Geoloaica LG, Patrascu V, Ciurea RN. Necrobiotic xanthogranuloma: case report and literature review. Curr Health Sci J 2021; 47: 126–131.