Nail apparatus melanoma (NAM) has a less favourable prognosis than other melanomas due to the difficulty of detecting lesions at an early stage (1–3). Although nail streaks (NS) are the most common clinical feature of early-stage NAM, the vast majority of NS encountered in the clinical setting are caused by benign diseases/conditions (4, 5). NAM-induced NS tend to be more varied in colour, which can be precisely determined using dermoscopy (6, 7). However, few standardized findings or indicators in dermoscopic practice for NS exist.
We recently developed a formula-based computer-aided automated evaluation programme for NAM detection. The programme calculated a melanoma discrimination index (MDI) score by analysing the colour diversity in dermoscopic images of NS (8). NAM-induced NS generally showed a higher MDI value than benign forms of NS, since they contained a wider variety of colours. To quantify the variety of RGB colour vectors in the region of interest more accurately, a function for standardizing the white balance was incorporated into the programme, and the formula for the MDI was revised based on the root mean square deviation of the latitude and longitudinal angles of RGB vectors (8) to that of RGB vector components, as demonstrated in the following formula:
We present here the diagnostic performance of the new MDI for differentiating NAM-induced NS from other benign NS in comparison with the results of dermatologists and non-dermatologist doctors according to the final diagnosis based on the results of biopsy and/or clinical follow-up.
MATERIALS AND METHODS
A dataset was created from patients seen at Shinshu University Hospital between 2007 and 2019 for benign NS and between 2007 and 2015 for NAM. Cases with the following features were excluded: highly damaged, lost or unpigmented nail plate, lesion onset earlier than 18 years of age, and dermoscopic images not containing the whole nail plate. The diagnosis of each case was confirmed by biopsy and/or clinical follow-up. A total of 100 dermoscopic images were randomly extracted from the dataset with adjustment to a benign:malignant ratio of 8:2 prior to testing.
Dermatologists and non-dermatologist doctors participated in this study as human readers who were expected to be users of the present programme in the dermatology and general clinical setting. Each reader was provided with the 100 dermoscopic images while blinded to all clinical information and was asked to give a decision regarding benignancy or malignancy (all readers) and immediate biopsy or not (dermatologists only).
The institutional review board of Shinshu University approved the study (number 4584). All human readers provided informed written consent. A waiver of patient consent was granted by the ethics board, since collecting dermoscopic images was retrospective and non-interventional.
After applying the same image pretreatment process as described in a previous report (8), the MDI of each test image was calculated using the programme installed on a laptop computer (Let’s note CF-SZ6; Panasonic Connect Co., Ltd, Tokyo, Japan) running Microsoft Windows 10 software. The MDI was calculated as the root mean square of RGB values over pixels contained in the region of interest (ROI) of a nail plate dermoscopic image to measure the variety of colour in the ROI.
The primary outcome measures were the area under the receiver operating characteristic curve (AUC) for the MDI. The MDI threshold was set as 40, at which Youden’s J index (sensitivity + specificity – 1) (9) reached its maximum value on the receiver operating characteristic curve. The sensitivity, specificity, and Youden’s J index at the threshold MDI were compared with those for malignancy detection (NAM-induced NS or benign NS) for dermatologists and non-dermatologist doctors and immediate biopsy decision for dermatologists only. In comparisons of the diagnostic performance between the MDI and human readers, unpaired t-tests were employed and the 95% confidence interval (95% CI) was calculated. A p-value <0.05 was considered statistically significant.
RESULTS
The test set included 80 benign NS cases from 62 patients and 20 NAM cases from 20 patients (Breslow’s tumour thickness: in situ, 11; ≤ 1.00 mm, 2; 1.01–2.00 mm, 1; 2.01–4.00 mm, 2; ≥ 4.01 mm, 3; unevaluated, 1) (Table SI and Fig. S1).
Representative test images and details on the devices that obtained the images are presented in Fig. S2 and Table SII. No remarkable discrepancies in MDI score were observed in dermoscopic images of the same lesion taken by different devices (data not shown). Twenty-nine dermatologists (clinical experience: ≤ 5 years, 0; 6–9 years, 1; ≥ 10 years, 28; 19 male and 10 female; 12 hospital doctors and 17 clinic doctors) and 8 non-dermatologists (clinical experience: ≤ 5 years, 2; ≥ 10 years, 6; 5 male and 3 female; 8 hospital doctors) participated in the study.
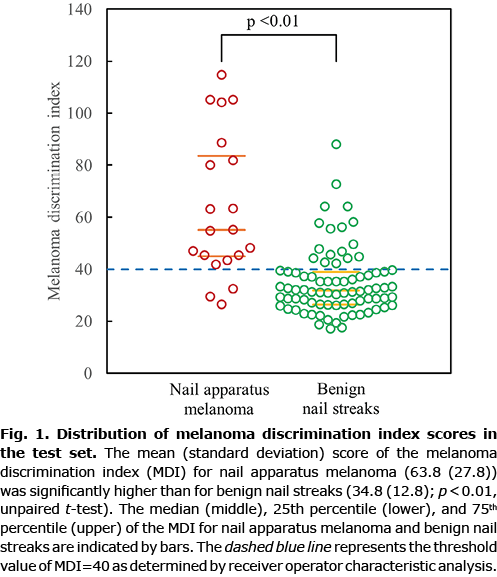
The diagnostic performance of the MDI and human readers is shown in Figs 1 and 2 and Table I. The AUC of the revised programme for detecting NAM was 0.85. When setting a threshold of ≥ 40 for malignancy detection, the sensitivity of the MDI (0.85) was significantly higher than the respective mean values of the dermatologists (0.58) and non-dermatologists (0.46) (both p < 0.01). The specificity of the MDI did not reach the respective mean values of the dermatologists or non-dermatologists. In calculations of Youden’s J index for measuring the performance of correctly diagnosing NAM and benign NS, however, that of the MDI (0.64) was considerably higher than those of the dermatologists (0.53) and non-dermatologists (0.43).
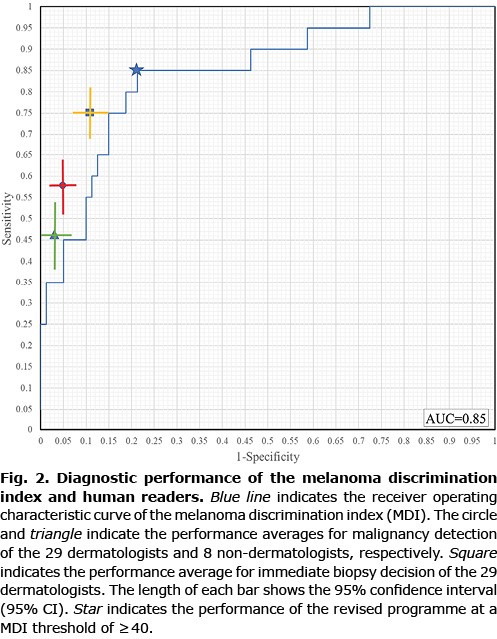
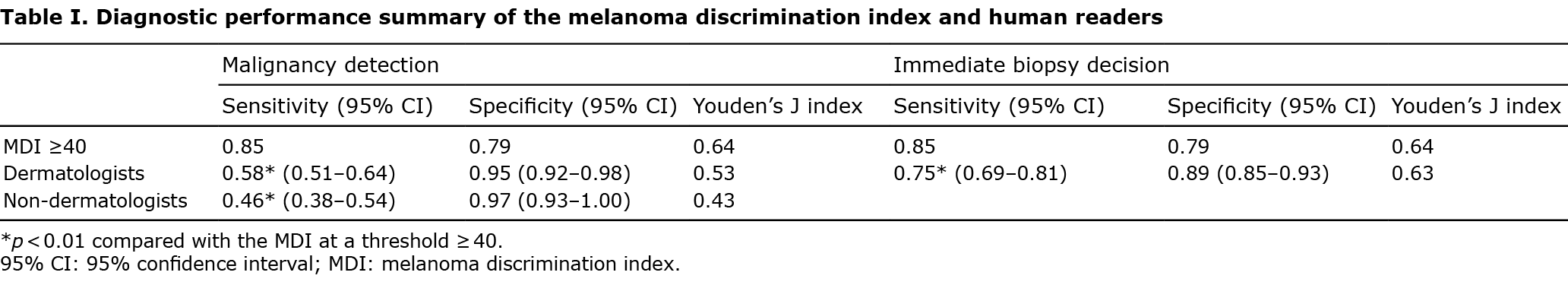
With respect to immediate biopsy decision, the sensitivity of the MDI (0.85) was significantly higher than that of the dermatologists (0.75) (p < 0.01), with comparable specificity and Youden’s J index (Table I).
DISCUSSION
This study revealed a significantly higher sensitivity for the MDI at an AUC-determined threshold ≥ 40 for detecting NAM in dermoscopic NS images compared with dermatologists and non-dermatologist doctors. Since half of the NAM images in the test set were of in situ lesions, the utility of the revised programme might also extend to include early NAM cases.
Recently, computer-aided programmes using deep learning convolutional neural networks have demonstrated high performance for recognizing melanoma in dermoscopic images, with NAM as a notable exception (10). A lack of training data due to the rarity of NAM is one possibility, and the particularity of NS image analysing, which focuses more on colour variation than on shape, may also be related. Our programme analyses the variation of RGB values in the ROI using a mathematical formula and represents it as an MDI score. One of the strengths of the programme over deep learning convolutional neural networks is the non-necessity of training data to refine diagnostic accuracy. Another advantage is the formula’s decision-making transparency as an objective indicator for dermoscopic images.
A considerable gap was observed between the sensitivity and specificity values of the human readers for malignancy detection, especially among non-dermatologists, in whom specificity exceeded 0.9, but sensitivity was below 0.5. This finding indicated that, while the human readers were screening benign NS with high sensitivity, their confidence for NAM-induced NS might have been low. Due to the rarity of NAM as well as the lack of standard criteria in dermoscopic practice for NS, it appears difficult even for dermatologists to differentiate between NAM-induced NS and other benign forms of NS. The Youden’s J index values of the MDI for malignancy detection were superior to those of the dermatologists and non-dermatologist doctors, suggesting that the MDI might serve as a useful tool to enhance the ability of detecting NAM while minimizing unnecessary biopsy procedures for benign NS. To the best of our knowledge, the MDI is among the first numericized indicators of colour in dermoscopic practice.
This study has several limitations. The study was conducted at a single centre using a limited number of images. In addition, the test image subjects and human readers were uniformly Japanese.
In conclusion, the higher performance of the revised MDI at a threshold ≥ 40 over dermatologists for detecting NAM demonstrated the potential utility of this objective indicator in dermoscopic practice for NS.
ACKNOWLEDGEMENTS
This study was supported by AMED under grant number JP22hk0102074h0002.
The authors have no conflicts of interest to declare.
REFERENCES
- Banfield CC, Redburn JC, Dawber RP. The incidence and prognosis of nail apparatus melanoma. A retrospective study of 105 patients in four English regions. Br J Dermatol 1998; 139: 276–279.
- O’Leary JA, Berend KR, Johnson JL, Levin LS, Seigler HF. Subungual melanoma. A review of 93 cases with identification of prognostic variables. Clin Orthop Relat Res 2000; 378: 206–212.
- Durbec F, Martin L, Derancourt C, Grange F. Melanoma of the hand and foot: epidemiological, prognostic and genetic features. A systematic review. Br J Dermatol 2012; 166: 727–739.
- Braun RP, Baran R, Le Gal FA, Dalle S, Ronger S, Pandolfi R, et al. Diagnosis and management of nail pigmentations. J Am Acad Dermatol 2007; 56: 835–847.
- Koga H, Saida T, Uhara H. Key point in dermoscopic differentiation between early nail apparatus melanoma and benign longitudinal melanonychia. J Dermatol 2011; 38: 45–52.
- Ronger S, Touzet S, Ligeron C, Balme B, Viallard AM, Barrut D, et al. Dermoscopic examination of nail pigmentation. Arch Dermatol 2002; 138: 1327–1333.
- Braun RP, Baran R, Le Gal FA, Dalle S, Ronger S, Pandolfi R, et al. Diagnosis and management of nail pigmentations. J Am Acad Dermatol 2007; 56: 835–847.
- Koga H, Yoshikawa S, Sekiguchi A, Fujii J, Saida T, Sota T. Automated evaluation system of dermoscopic images of longitudinal melanonychia: proposition of a discrimination index for detecting early nail apparatus melanoma. J Dermatol 2014; 41: 867–871.
- Youden WJ. Index for rating diagnostic tests. Cancer 1950; 3: 32–35.
- Winkler JK, Sies K, Fink C, Toberer F, Enk A, Deinlein T, et al. Melanoma recognition by a deep learning convolutional neural network – performance in different melanoma subtypes and localisations. Eur J Cancer 2020; 127: 21–29.