Atopic eczema (AE) is an IgE-sensitized chronic relapsing inflammatory skin disease with eczematous dermatitis and severe pruritus as the principal features (1). Whereas chronic eczema (CE) is exemplified by lichenified plaques and fibrotic papules, AE is commonly characterized by intensely pruritic and erythematous papules, vesicles with excoriations, and serous exudate (1). Emollients, topical corticosteroids, calcineurin inhibitors, and phototherapy are currently the main treatments for AE (2). Acupuncture is a common alternative treatment for patients with AE or CE (3). However, a previous meta-analysis of the use of acupuncture for AE included only a few studies, resulting in limited analyses and conclusions (3). More recently, well-designed randomized controlled trials (RCTs) have been published in this field (4, 5). The aim of this study was to perform an updated systematic review and meta-analysis to further explore the efficacy of acupuncture for treatment of AE and CE, including detailed subgroup analyses.
MATERIALS AND METHODS
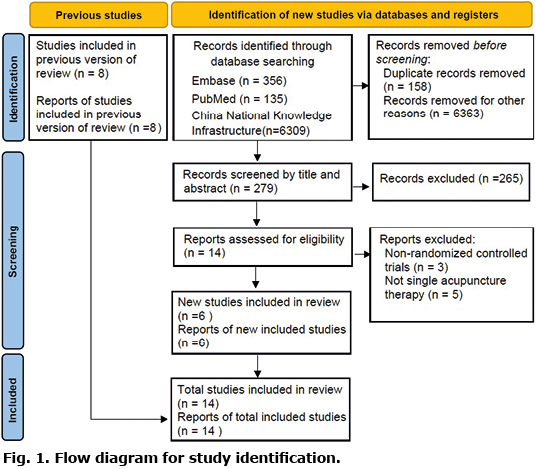
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement 2020 was used to perform the meta-analysis (http://www.prisma-statement.org/).
Databases, including PubMed, EMBASE, and China National Knowledge Infrastructure, were searched from inception to 31 May 2022. The search focused on clinical studies involving humans published in any language. The key words “atopic dermatitis,” “AE,” or “eczema,” combined with “acupuncture” in free text were used for the literature search.
The inclusion criteria for this study were: (i) RCTs, (ii) patients with AE or CE, and (iii) intervention group involving single acupuncture therapy and control group involving no treatment, sham, or conventional therapies. Studies involving moxibustion, laser acupuncture, cupping, pricking, blood-letting, or any acupuncture therapy combined with Chinese herbs were excluded.
The revised Cochrane Risk of Bias 2 (RoB 2) tool was used to assess the quality of the included studies. The following parameters were extracted: country, inclusion criteria, sample size, type, frequency, acupuncture acupoints, treatment of control groups, and outcome assessment (Table SI). Changes in disease severity and quality of life (QoL) scores were also extracted, along with the proportion of patients with more than 60% global symptom improvement and adverse events (Tables SII and SIII).
Pooled estimates for improvement in disease severity and QoL were calculated for patients who received acupuncture vs patients in control groups. Patients with AE and patients with CE were analysed separately. Subgroup analyses were performed in patients with CE to compare acupuncture with the different individual conventional therapies. Dichotomous analyses were performed using risk ratio (RR), and continuous data were analysed using standardized mean difference (SMD) with 95% confidence intervals (CI). The I2 test was performed for heterogeneity testing. A random effects model was adopted. Publication bias was tested when more than 10 studies were included for analysis. The software Comprehensive Meta-Analysis Version 3 (Biostat, Inc., Englewood, NJ, USA) was used to perform all analyses. The Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) tool was used to evaluate the certainty of evidence. Detailed Materials and Methods are given in Appendix S1.
RESULTS
A total of 14 studies with 874 patients met the inclusion criteria, consisting of 6 new studies and 8 studies in previous meta-analysis (3) out of the 279 potentially relevant publications identified through the online database searches (Fig. 1). Characteristics of included studies are summarized in Table SI. The detailed data of the clinical responses to treatments are shown in Table SII. Three out of the 14 studies (4–6) included patients with AE, and the other 11 studies included patients with CE. The acupuncture type included manual acupuncture (MA) and fire needling (FN). All studies on AE involved MA in the treatment group and either no treatment (6) or sham (4, 5) in the control group. All studies on CE involved FN in the treatment group, except for 1 study that combined FN and MA (7), while the control group received conventional therapies (topical corticosteroid or oral antihistamines). No serious adverse events were reported.
RoB 2 assessment is shown in Fig. S1. The lack of blinding in the study participants, assessors, or acupuncturists in most of the studies on CE resulted in high risk of bias in the measurement of outcomes.
Results of meta-analyses and GRADE evaluation are shown in Table I. Pooled analysis of patients with AE showed that patients who received MA had significantly better improvement in SCORAD compared with patients in the control groups (SMD −1.335; 95% CI −2.024–−0.646) (Fig. S2). The changes in Eczema Area and Severity Index (EASI), Patient Oriented Eczema Measure (POEM), itch intensity by visual analogue scale (VAS), and QoL score (Figs S3–S6) were not significantly different between treatment and control groups in patients with AE. The pooled estimates in patients with CE showed higher proportion of more than 60% global symptom improvement in patients receiving FN than in patients receiving conventional therapies (SCORAD RR 1.539; 95% CI 1.299–1.824) (Fig. S7). The improvement in EASI score (SMD −0.415; 95% CI −0.792 to −0.038) and VAS score (SMD −1.062; 95% CI −1.961 to −0.163) was significantly more in patients receiving FN than in patients receiving conventional therapies. The change in QoL score was similar in the 2 groups (Figs S8–10). In subgroup analyses of individual conventional therapies, patients with CE who received FN showed higher proportions of global symptom improvement compared with both topical corticosteroids and oral antihistamine (Fig. S7) However, significant improvements in EASI, VAS, and QoL score were only noted when comparing FN with oral antihistamine (and not topical corticosteroids) in patients with CE. (Figs S8–10).
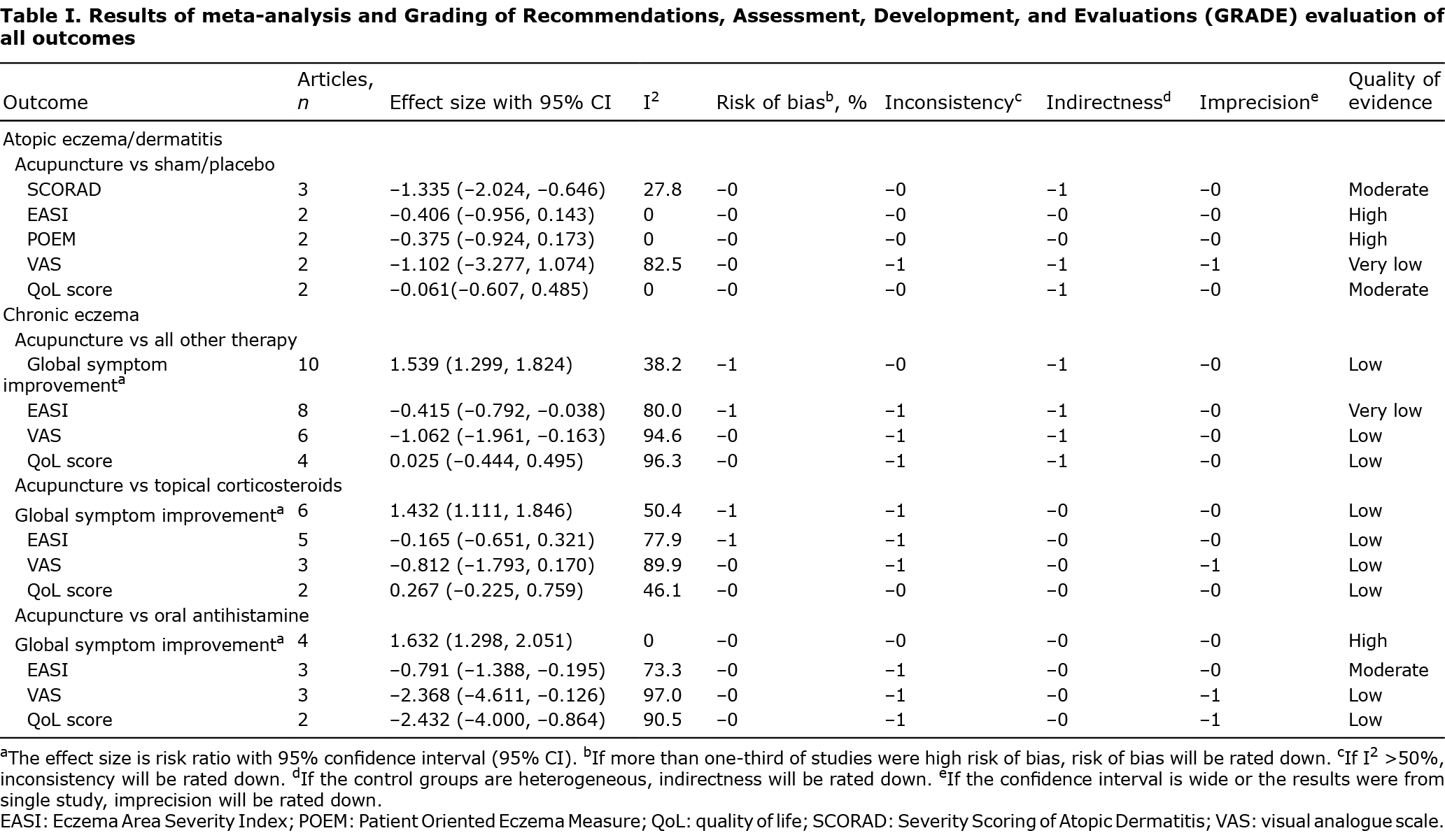
Publication bias was noted when performing pooled estimates of global symptom improvement. However, after adding 3 studies to the left in the trim-and-fill test, the proportion of patients was still higher in patients receiving FN than in patients receiving conventional therapies (Fig. S11). Most of the results regarding AE were of moderate quality based on the GRADE evidence rating scale. However, most of the results regarding CE were of low quality owing to the high risk of bias and inconsistency in included studies.
DISCUSSION
Studies have shown that acupuncture reduces basophil activation and type I hypersensitivity reactions in patients with atopic disease (8). Increased interleukin (IL)-4 signalling has been found to be closely related to the development of pruritus with AE, by activating peripheral sensory nerves and inducing chronic itch (8). Recent research shows that acupuncture ameliorates AE-like skin inflammation through the blockade of 5-HT receptors, which decreases histamine-induced acute itching (8, 9). Acupuncture also reduces serum levels of IL-2 and IL-4 and increases the level of interferon-γ in patients with CE (8).
The current study had several limitations. First, patient sample size was limited in the analysis of AE. Secondly, the lack of blinding in the study participants, assessors, or acupuncturists in most of the studies led to inevitable performance bias, which resulted in lower quality of evidence in CE. Thirdly, there was inter-study variability resulting from acupuncture characteristics (different types, frequency, and especially acupuncture acupoints) and different control groups, although subgroup analyses were performed to minimize heterogeneity. Finally, a majority of the trials consisted of only short-term follow-ups, which hindered the ability to determine the long-term effect of acupuncture on patients with AE.
In conclusion, this meta-analysis demonstrated that patients with AE who underwent acupuncture had reduced severity of the condition compared with the control group. Acupuncture reduces the severity of disease scores and improves the QoL of patients with CE compared with treatment with oral antihistamine. However, further research is needed to elucidate the underlying mechanisms and assess the efficacy of acupuncture in treating AE and CE.
The authors have no conflicts of interest to declare.
REFERENCES
- Boguniewicz M, Leung DY. 10. Atopic dermatitis. J Allergy Clin Immunol 2006; 117: S475–S480.
- Abramovits W. Atopic dermatitis. J Am Acad Dermatol 2005; 53: S86–S93.
- Jiao R, Yang Z, Wang Y, Zhou J, Zeng Y, Liu Z. The effectiveness and safety of acupuncture for patients with atopic eczema: a systematic review and meta-analysis. Acupunct Med 2020; 38: 3–14.
- Kang S, Kim YK, Yeom M, Lee H, Jang H, Park HJ, et al. Acupuncture improves symptoms in patients with mild-to-moderate atopic dermatitis: a randomized, sham-controlled preliminary trial. Complement Ther Med 2018; 41: 90–98.
- Park JG, Lee H, Yeom M, Chae Y, Park HJ, Kim K. Effect of acupuncture treatment in patients with mild to moderate atopic dermatitis: a randomized, participant- and assessor-blind sham-controlled trial. BMC Complement Med Ther 2021; 21: 132.
- Pfab F, Athanasiadis GI, Huss-Marp J, Fuqin J, Heuser B, Cifuentes L, et al. Effect of acupuncture on allergen-induced basophil activation in patients with atopic eczema: a pilot trial. J Altern Complement Med 2011; 17: 309–314.
- Liu K. Clinical research on superficial insertion of filiform-fire needle combined with acupuncture on chronic eczema. Guangzhou, China: Guangzhou University of Chinese Medicine. 2017 (in Chinese).
- Tang Y, Cheng S, Wang J, Jin Y, Yang H, Lin Q, et al. Acupuncture for the treatment of itch: Peripheral and Central Mechanisms. Front Neurosci 2022; 15: 786892.
- Park HJ, Ahn S, Lee H, Hahm DH, Kim K, Yeom M. Acupuncture ameliorates not only atopic dermatitis-like skin inflammation but also acute and chronic serotonergic itch possibly through blockade of 5-HT2 and 5-HT7 receptors in mice. Brain Behav Immun 2021; 93: 399–408.