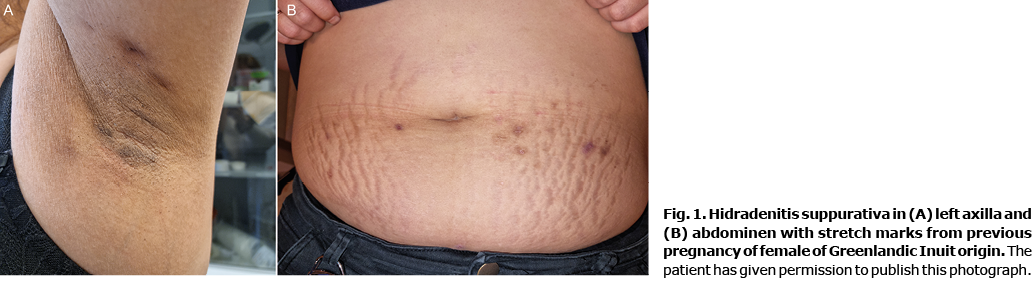
Hidradenitis suppurativa (HS) is an inflammatory skin disease characterized by recurrent or chronic painful suppurating lesions in the apocrine gland-bearing regions of the skin (Fig. 1). According to previous estimates HS affects approximately 0.05–4.10% of investigated populations (1). The reported prevalence of HS in Asia is rarer (2), while the prevalence in Greenland is unknown. HS is 3 times more common in women and often debuts after puberty. HS is associated with several comorbidities, such as arthritis, depression, diabetes, metabolic syndrome, obesity, and suicide. The all-cause mortality is also increased (1, 3). There are no curative treatments for HS. The current regimen consists of topical antiseptic and antibiotic treatment, followed by systemic antibiotic treatment and/or tumour necrosis factor (TNF)-alpha inhibitors (4). In severe cases, surgical treatment may become necessary. If untreated, the disease has a major negative impact on the patient’s quality of life (5). HS is relatively unknown by non-dermatologists and is often confused with infectious skin conditions, such as abscesses, carbuncles, and furuncles; hence the mean delay from symptoms to established diagnosis is 7.2 years (1).
A prerequisite to increasing our understanding of the pathogenesis and to strengthening the treatment efforts for HS is to determine the prevalence of the disease, and its characteristics. The aim of this study was to determine the physician-verified prevalence of HS among a standardized sample of the Greenlandic Inuit population in a primary care setting in Greenland. Greenland has a population of approximately 56,400 people, of which 18,800 people live in the capital Nuuk. Ninety percent of the population are of Greenlandic Inuit origin. The remaining 10% consists of immigrants from Denmark, Iceland, the Philippines, and Thailand. The official languages are Greenlandic Inuit language and Danish (6).
MATERIALS AND METHODS
The background population was obtained from Statistics Greenland (6), and included all people living in Nuuk on 1 January 2021 (n = 18,800).
All adults age 18 years or older who attended the Queen Ingrid’s Health Care Center in Nuuk from 1 November to 31 December 2021, were invited to complete a validated screening questionnaire developed by Vinding et al. (7; Appendix 1). The questionnaire was available in 3 languages: Danish, Greenlandic and English, translated by native speakers. If the questionnaire indicated symptoms of HS, clinical examination of the patient’s axillae and groins was performed to ascertain presence of the self-reported disease. Furthermore, 10% of the screen screen-negative participants were also examined to verify the outcome HS.
The study was approved by the Ethics Committee for Scientific Research in Greenland (KVUG 2021-15, case-number: 2021-12990) and the agency of Health and Prevention in Greenland.
Statistical analysis
Prevalence ratios (PR) were calculated to compare prevalence estimates and χ2 tests used to compare frequencies between groups. Diagnostic sensitivity data was calculated based on 2×2 tables, with the diagnosis of either HS or not HS used as the reference test, with HS as the target condition, and the questionnaire as the index test. Covariates were described with mean and/or standard deviation (SD) or with median and interquartile range (IQR). All estimates were calculated with 95% confidence intervals (95% CI) and/or range. p-values below 0.05 were considered significant. All statistical analyses were performed in using R (https://www.r-project.org/). Descriptive statistics was used to describe differences between the HS and non-HS group. All data remained anonymized.
RESULTS
A total of 506 participants completed the questionnaire, corresponding to 2.7% of the population in Nuuk and 0.9% of the total Greenlandic population.
Table I shows the prevalence and characteristics of the participants. The prevalence of HS in the study group was 3.2% (16 patients). None of the 10% examined screen-negative participants had HS. Among the 16 identified patients with HS, 87.5% were females and 93.8% were of Greenlandic Inuit origin. The majority of the patients with HS: 93.6% were daily smokers. Furthermore, the mean BMI of the patients with HS was 29.1 kg/m2, and the mean age was 40.5 years. For further details, see Table I.
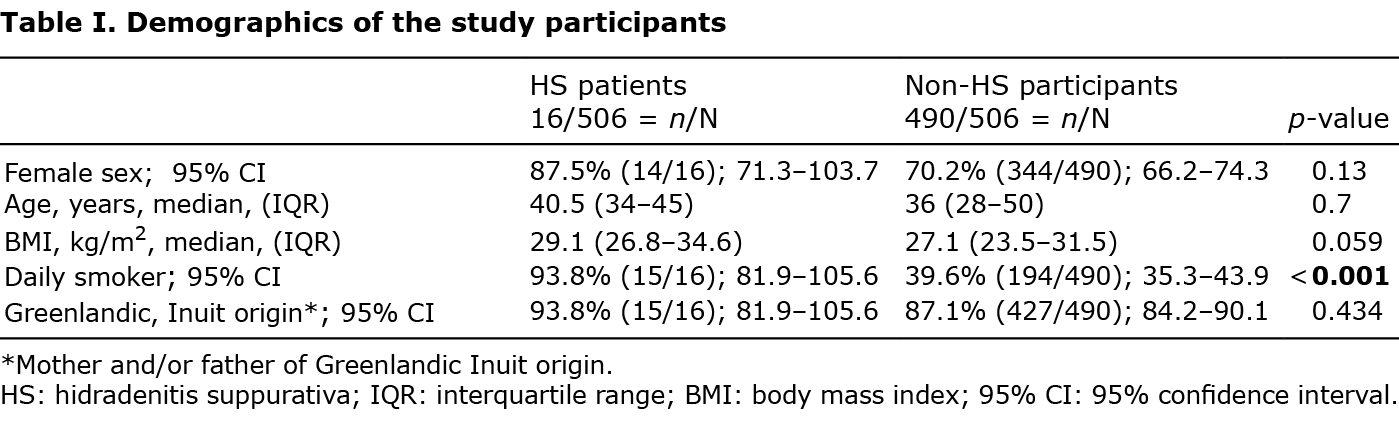
Among the 490 non-HS participants, 70.0% were females, 87.1% of Greenlandic Inuit origin, and 39.5% daily smokers. The mean BMI of the non-HS participants were 27.1 kg/m2 and the mean age was 36 years. There was no statistically significant difference between the HS-group compared with the non-HS participants in terms of age, sex, BMI, or origin. There were significantly more daily smokers among the patients with HS compared with the non-HS participants (p < 0.001).
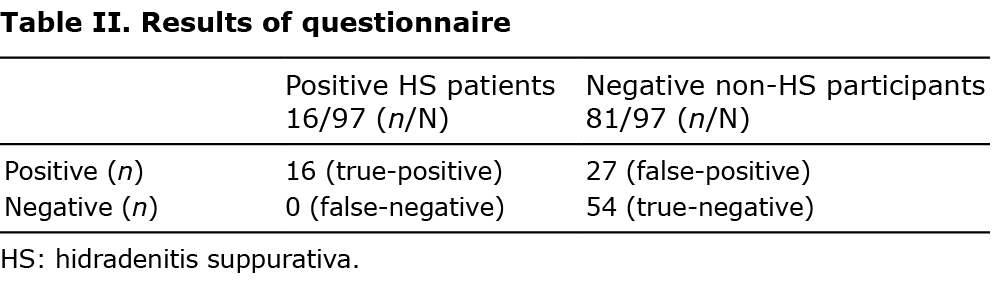
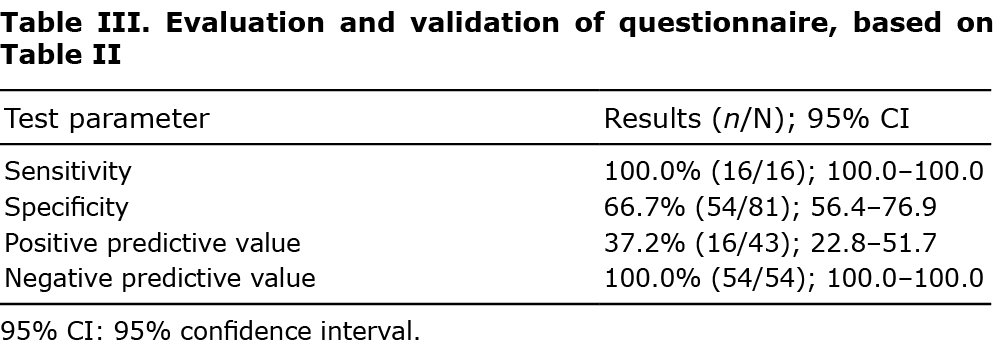
Tables II and III show the results and validation of the HS questionnaire. The sensitivity of the HS questionnaire was 100.0%, specificity 66.7%, positive predictive value 37.2% and negative predictive value 100.0%.
DISCUSSION
This study found a prevalence of HS of 3.2% among the adult population in Nuuk, Greenland, with a vast majority of female and overweight patients. When investigating the race-specific prevalence, the prevalence was higher; 3.4% (15/422) among the participants of Greenlandic Inuit origin, and lower; 1.6% (1/64) among participants of other origin. The understanding of race-specific prevalence of HS is currently limited. US registry data have suggested that HS may be more common in the Black population than in Caucasians, while studies in Africa have suggested comparable prevalence rates to those previously found in predominantly white Australian population samples (8, 9). Burden of disease and participation in pharmacological studies also appear to be unevenly distributed between the various races (10, 11). To the best of our knowledge, no trials in HS have hitherto been conducted in Greenland, and no information exists on the prevalence of HS in the Arctic region. Additional studies are therefore needed to explore which extrinsic and intrinsic factors may help explain this exceptionally high observation of HS.
Previous studies of HS in other populations have indicated a female to male ratio of 3:1 in Caucasian populations, but not in African or Asian populations (12, 13). This was also the case in the current study group.
There was no statistically significant difference between the HS group and the non-HS participants in terms of age, sex, BMI, or origin. This is most likely a consequence of the low statistical power associated with the modest sample size, as there were “only” 16 patients with HS in this study. There were significantly more daily smokers among the patients with HS compared with the non-HS participants. This is in line with previous studies, suggesting an association between smoking and HS (14). Smoking is very common among the general population in Greenland: approximately 60% of the population are smokers (15).
The sensitivity of the validated HS questionnaire was 100.0%, and the specificity was 66.7%. However, there were many false-positive participants who had other skin conditions, such as acne, folliculitis and eczema, revealed by clinical examination. Hence, this study supports the importance of clinical examination of all patients with self-reported clinical symptoms of HS to ascertain a correct diagnosis.
The current study supports that genetics, climate, and environmental factors might play an important role in the aetiology and development of HS. Thus, the results contribute to an increased awareness of HS. Further research is necessary to improve diagnostics and treatment of HS in Greenland. Finally, this study contributed to the Global Hidradenitis Suppurativa Atlas (GHiSA), a worldwide collaboration on the prevalence of HS across more than 50 countries distributed among 6 continents (https://ghisa.org/).
ACKNOWLEDGEMENTS
The study was supported by the Greenlandic Research Foundation for Medical Doctors in Greenland. We would especially like to thank our Greenlandic colleagues Aviannguaq Kreutzmann and Trine Pedersen Abelsen for their indispensable contribution to this study. This study could not have been conducted without their translations and knowledge of the Greenlandic Inuit language. We would also like to thank all the patients, who let us examine them and take clinical photographs of their skin conditions.
Conflicts of interest: DB: UCB Nordic has paid for EADV congress participation. RKA: Eli Lilly has paid for NCDV 2022 congress participation. SFT has been a speaker or advisor for Sanofi, AbbVie, LEO Pharma, Pfizer, Eli Lilly, Novartis, UCB Pharma, Almirall, Union Therapeutics, and Janssen Pharmaceuticals; and has received research support from Sanofi, AbbVie, LEO Pharma, Novartis, UCB Pharma, and Janssen Pharmaceuticals, outside the submitted work. DMS received honoraria as a consultant for advisory board meetings by AbbVie, Janssen, Sanofi, LeoPharma and as a speaker and/or received grants from the following companies: Abbvie, Janssen, Novartis, Sanofi and Leo Pharma during the last 3 years. GBEJ has received research funding and/or honoraria from Abbvie, InflRx, Janssen-Cilag, Leo Pharma, Novartis, ChemoCentryx, Regeneron and Serono. The other authors have no conflicts of interest to declare.
REFERENCES
- Saunte DML, Jemec GBE. Hidradenitis suppurativa: advances in diagnosis and treatment. JAMA 2017; 318: 2019–2032.
- Kamil MAA, Chandran NS, Sulistyaningrum K, Rajagopalan M, Tahiliani S, Hsiao J, et al. The Asia Pacific Hidradenitis Suppurativa (APHiS) foundation: promoting hidradenitis suppurativa research in the Asia Pacific HHS Public Access. Int J Dermatol 2020; 59: 289–290.
- Jemec GBE. Clinical practice. Hidradenitis suppurativa. New Engl J Med 2012; 366: 158–164.
- Zouboulis CC, Desai N, Emtestam L, Hunger RE, Ioannides D, Juhász I, et al. European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa. J Eur Acad Dermatol Venereol 2015; 29: 619–644.
- Krajewski PK, Matusiak Ł, von Stebut E, Schultheis M, Kirschner U, Nikolakis G, et al. Quality-of-life impairment among patients with hidradenitis suppurativa: a cross-sectional study of 1795 patients. Life 2021; 11: 34.
- [Statistics G. Greenland in Numbers 2021; 3rd Edition][cited 2022 Jun 20]. Available from: www.stat.gl.
- Vinding GR, Miller IM, Zarchi K, Ibler KS, Ellervik C, Jemec GBE. The prevalence of inverse recurrent suppuration: a population-based study of possible hidradenitis suppurativa. Br J Dermatol 2014; 170: 884–889.
- Sachdeva M, Shah M, Alavi A. Race-specific prevalence of hidradenitis suppurativa. J Cutan Med Surg 2021; 25: 177–187.
- Hagan PG, Bouazzi D, Nyarko G, Dartey ES, Nunoo-Ghartey KB, Nkum D, et al. Prevalence of hidradenitis suppurativa in Berekum, Ghana. Br J Dermatol 2022; 187: 586–587.
- Price KN, Hsiao JL, Shi VY. Race and ethnicity gaps in global hidradenitis suppurativa clinical trials. Dermatology 2021; 237: 97–102.
- Lee DE, Clark AK, Shi VY. Hidradenitis suppurativa: disease burden and etiology in skin of color. Dermatology 2017; 233: 456–461.
- Ahmad Kamil MA, Mohd Affandi A. Hidradenitis suppurativa in Kuala Lumpur, Malaysia: a 7-year retrospective review. Dermatol Res Pract 2018; 2018: 2017959.
- Yang JH, Moon J, Kye YC, Kim KJ, Kim MN, Ro YS, et al. Demographic and clinical features of hidradenitis suppurativa in Korea. J Dermatol 2018; 45: 1389–1395.
- Dauden E, Lazaro P, Aguilar MD, Blasco AJ, Suarez C, Marin I, et al. Recommendations for the management of comorbidity in hidradenitis suppurativa. J Eur Acad Dermatol Venereol 2018; 32: 129–144.
- Bjerregaard P, Larsen CVL. Three lifestyle-related issues of major significance for public health among the Inuit in contemporary Greenland: a review of adverse childhood conditions, obesity, and smoking in a period of social transition. Public Health Rev 2018; 39: 5.