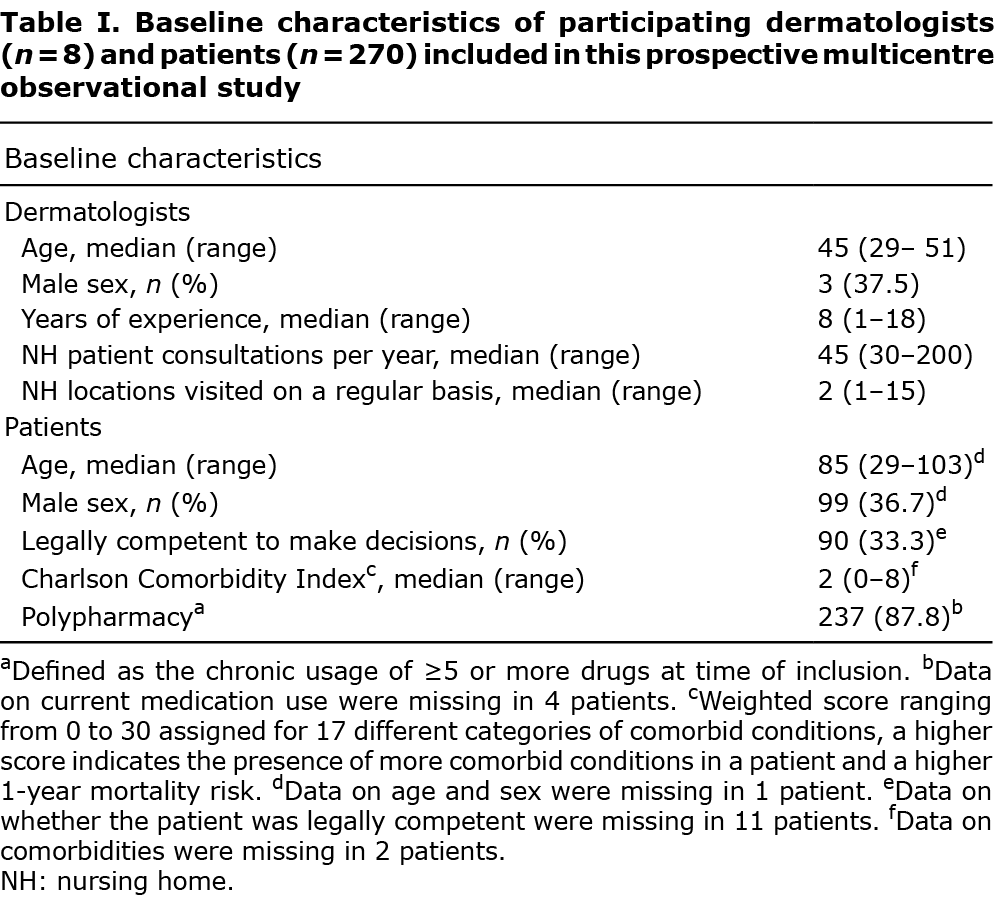
Considering the limited availability of dermatologists to perform live consultations in nursing homes, teledermatology could be used as a triage tool for selection of cases for which live consultations are considered to be of added value compared with teledermatology. This prospective, multicentre observational study aimed to determine the reasons for dermatology consultations in nursing homes and the estimated value of teledermatology as a triage tool, including potential predictors. Skin tumours were the most common reason (n = 161/270; 59.6%) for dermatology consultations in nursing homes. Dermatologists estimated that live consultations added value compared with teledermatology in 67.8% of cases (n = 183). Multivariable logistic regression showed that predictors for this added value of live consultations were: consultations because of a skin tumour; consultations during which a diagnostic or treatment procedure was performed; consultations during which a secondary diagnosis was made; and the dermatologist involved. These results indicate that using teledermatology as a triage tool potentially reduces the need for additional live consultations in one-third of patients, whereas live consultations are estimated to have added value over teledermatology in two-thirds of cases. To make optimal use of the limited capacity for live consultations by dermatologists, it could therefore be helpful if elderly care physicians use teledermatology more frequently.
Key words: elderly care; geriatric dermatology; nursing home; teledermatology; telemedicine.
Accepted Nov 1, 2022; Epub ahead of print Nov 1, 2022
Acta Derm Venereol 2022; 102: adv00827.
DOI: 10.2340/actadv.v102.4459
Corr: Satish F. K. Lubeek, Department of Dermatology, Radboud University Medical Center, Box 102, NL-6500 HB Nijmegen, The Netherlands. E-mail: Satish.Lubeek@radboudumc.nl
SIGNIFICANCE
Considering the limited availability of dermatologists to visit patients in nursing homes, teledermatology could serve as a triage tool to select those cases in which seeing a patient physically is considered necessary. In order to provide the most optimally organized and efficient dermatological care in nursing homes, teledermatology and live consultations go hand in hand. This study shows that using teledermatology as a triage tool could reduce the need for additional live consultations in one-third of patients, whereas live consultations are estimated to have added value over teledermatology in two-thirds of cases, especially in patients with skin tumours.
INTRODUCTION
With the rapidly ageing world population and increasing prevalence of multimorbidity, increasing numbers of people are in need of institutionalized long-term healthcare, as provided in nursing homes (NHs) (1–4). Among older adults living in NHs, skin diseases form a major health problem (with prevalences of the most common skin disorders ranging from 1% to 44%) and could have a significant impact on quality of life (5–8). The most common skin diseases in this patient group are eczema, fungal infections, (pressure) ulcers, and both benign and (pre)malignant skin tumors (9–13). Therefore, in this vulnerable patient group, consultation with a dermatologist is often desirable (14, 15). However, attending a dermatology clinic may not be feasible due to severe functional or cognitive impairment and/or logistical limitations.
Previous studies in different countries have indicated that current dermatological care in NHs might be improved in several ways, mainly by using teledermatology (TD) more frequently and by enabling dermatologists to visit NHs (14–21). Store-and-forward (SAF)-TD is the most commonly used type of TD, and includes the use of asynchronous still digital image technology for communication (17). Multiple studies demonstrated that SAF-TD is a cost-effective and easy-to-use consultation method, which was shown to be of significant value in daily dermatological practice, especially in patients who are not that easily able to attend a dermatological practice (18). On the other hand, SAF-TD is currently only used by a minority of elderly care physicians in the Netherlands and has several practical limitations (e.g. limited diagnostic accurary in pigmented skin lesions) (16–18, 22). Obviously, additional live consultation (LC) with a dermatologist might be needed in case of diagnostic doubt and/or when a dermatologist is needed to perform a diagnostic or therapeutic intervention.
Although the majority of dermatologists in the Netherlands are willing to visit patients in NHs when indicated, a lack of time, daily practice efficacy, and financial compensation are mentioned as important thresholds (16). A nationwide survey study in the Netherlands in 2014 indicated that only 30% of the responding dermatologists had ever visited a NH for LCs (16). Due to this limited availability and capacity of LCs with dermatologists in NHs, TD could serve as an important triage tool to select those cases in which additional LC by a dermatologist might be of added value and thereby enable optimal efficacy of dermatological care in NHs. However, little is currently known regarding the added value of LC vs TD in this population. The aims of this study were therefore to determine: (i) the reasons for NH consultations by dermatologists; and (ii) the estimated value of SAF-TD as a triage tool, including potential predictors.
MATERIALS AND METHODS
Study design and participants
In this prospective multicentre observational study data from live NH consultations were prospectively collected between 18 February 2015 and 11 February 2021. Dermatologists (or dermatology residents supervised by a dermatologist) who regularly visited patients in different NHs in the Netherlands and were experienced in using SAF-TD were asked to participate. Patients were chronologically included in 20 different NHs throughout the Netherlands. The indication for a live dermatologist consultation in the NH was estimated by the patients’ treating elderly care physician during regular daily clinical practice. Patients were then pre-registered for a consultation using a regular referral procedure including a standardized referral letter. None of the participating elderly care physicians used dermoscopy during the study period. Each patient could only be included in the study once. In case patients were visited multiple times for several dermatological problems during the study period, only the first visit including the first-mentioned dermatological problem was included. The need for a full-body examination by the consulting dermatologist was determined on a case-by-case basis.
Study outcomes and data collection
The participating physicians prospectively collected data using a predefined data-sheet based on multiple data sources (e.g. standardized referral letters, patient charts, findings during the NH consultations, pathology results). The pre-defined data-sheet, which is partially available in Appendix S1, was developed during a multidisciplinary brainstorming session by physicians in dermatology and NH care, and was pre-tested in 10 physicians to ensure optimal feasibility, comprehensibility and completeness of the questions, instructions and response options. The pre-defined data-sheet included sections on patient, disease and referral characteristics, consultation outcomes (including final diagnosis, applied diagnostic procedures and treatment) and consultation evaluation. Furthermore, baseline characteristics regarding every participating dermatologist (e.g. on years of experience, number of NH visits per year) were also collected.
Primary outcomes in this study were: (i) reasons for NH consultations and (ii) the estimated value of SAF-TD as a triage tool, including potential predicting characteristics on the latter. The reason for live NH consultation was defined as the final diagnosis made by the dermatologist. A histopathological diagnosis was used as the final diagnosis, when available. In case of no histopathological diagnosis, the clinical diagnosis made by the dermatologist was used. The reasons for NH consultations were collected using an open-ended question, and further categorized using the following disease groups: benign tumour, premalignant tumour, malignant tumour, eczema, (pressure) ulcers, skin infection, and other. To evaluate the estimated value of SAF-TD as triage tool the dermatologists were asked to complete an “added value score”, which was a 5-point-Likert scale on the estimated added value of LC compared with SAF-TD (ranging from 0: “no added value” to 5: “a lot of added value”), followed by an open-ended question for further explanation and comments. Also, a multiple choice question was used where the dermatologists had to estimate whether they would have advised the same policy if they had only been approached by SAF-TD (“yes”, “no” or “not sure”). It was hypothesized that potential predicting characteristics for added value of a LC compared with SAF-TD might be the skin disease that was diagnosed, comorbidities, polypharmacy, whether a diagnostic or treatment procedure was perfomed, whether a secondary diagnosis was noted, or if the patient was legally competent to make medical decisions. Data on comorbidity were used to calculate the Charlson Comorbidity Index (International Classification of Diseases 10th revision; ICD-10 version), which is the most commonly used comorbidity index. This index results in a weighted score ranging from 0 to 30 assigned for 17 different categories of comorbid conditions, based on the 1-year relative mortality risk (a higher score indicates the presence of more comorbid conditions in a patient and a higher mortality risk) (23). Polypharmacy was defined as the chronic usage of ≥ 5 drugs at time of inclusion (24). The study was performed according to Dutch legislation (the “Medical Research Involving Human Subjects Act” (Wet medisch-wetenschappelijk onderzoek met mensen; WMO)). Due to the design and nature of this study the medical ethics committee waived the need for formal approval and written informed consent according to Dutch legislation.
Statistical analysis
First, baseline characteristics of dermatologists and patients were described and a univariate analysis was performed to study the relationship between potential predicting characteristics and the added value score.
For further analyses, the added value score provided by the dermatologists were categorized into 2 groups: “no added value” (Likert scores 1–3) and “added value” (Likert scores 4–5). Potential predicting characteristics included in the analysis were: disease group, Charlson Comorbidity Index, polypharmacy, whether a diagnostic procedure was performed during the NH consultation, whether a secondary diagnosis was noted during the NH consultation, whether a treatment procedure was performed during the NH consultation, the dermatologist who visited the NH patient and rated the consultation (hereafter noted as “the rating dermatologist”) and whether the patient was legally competent to make medical decisions. Continuous data were expressed as median and range. Categorical data were expressed as number and percentage. For univariate analysis, categorical data were compared using a χ2 test (or Fisher’s exact test in case any of the cells had an expected count of less than 5).
Subsequently, multivariable logistic regression analysis was performed to further study the influence of the characteristics, which showed a statistically significant outcome in the univariate analysis on the added value score (“no added value” vs “added value”). The selection and inclusion of variables in this regression model were based on the rule of thumb that for multivariable logistic regression at least 10 observations per variable in the model are required on the least prevalent of the 2 outcomes. Based on a first analysis we chose to further simplify the model by reducing the number of variables described here. Because adding a categorical variable with K categories adds K–1 dummy variables to the model, categorical variables have to be handled with care. Hence, the variable “disease group”, which originally contained 4 categories in the first model (eczema, benign-, premalignant- and malignant skin tumour) was simplified to a dichotomous variable (eczema vs no eczema). “Rating dermatologist” is a categorical variable with 8 categories. This would also be too demanding for the data available. Therefore, observations made by the 4 dermatologists with 10 observations or fewer were excluded, reducing the number of cases available by 16, but reducing the number of variables in the model by 4. To further reduce the number of variables in the model we chose to combine 2 variables into 1 (diagnostic and treatment procedure performed). The results of both models are described below.
In all analyses, p-value < 0.05 was considered statistically significant. Data were analysed using Statistical Package for Social Sciences (SPPS) Statistics for Windows, version 25.0 (IBM, Armonk, NY, USA).
RESULTS
Baseline characteristics
Data on 270 consecutive NH consultations with 270 unique patients were collected by the participating dermatologists (n = 8), visiting 20 different NHs between 18 February 2015 and 11 February 2021. None of the NHs used SAF-TD during the inclusion period. Baseline characteristics of the dermatologists and patients are summarized in Table I. In 39.4% (n = 106) of the live NH consultations 1 or more diagnostic procedures were performed by the dermatologists. Dermoscopy was used most frequently; namely in 65 (24.1%) of the consultations, followed by punch biopsy (n = 48; 17.8%). In 19.3% (n = 52) of the live NH consultations a secondary diagnosis was made. The most common secondary diagnoses were: premalignant tumours (n = 20; 37.7%); followed by malignant tumours (n = 11; 20.8%) and skin infections (n = 6; 11.3%). In 71.9% (n = 194) of the cases, the visit resulted in a therapeutic intervention (e.g. cryotherapy (shave) excision). A full overview of the consultation characteristics is shown in Table II.
Reasons for dermatology consultations in nursing homes
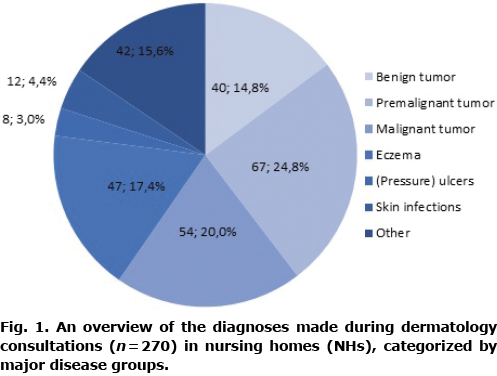
Fig. 1 provides an overview of the reasons for dermatology consultations in NHs. Skin tumours (both benign and (pre)malignant) accounted for 59.6% (n = 161) of the reasons for NH consultations. Of the malignant skin tumours, 70.9% (n = 39) were histopathologically confirmed. In the group “other”, diagnoses were clustered, such as psoriasis (n = 9; 3.3%), pruritus sine materia (n = 3; 1.1%), and bullous skin diseases (n = 5; 1.9%).
Value of live consultations in nursing homes compared with store-and-forward teledermatology
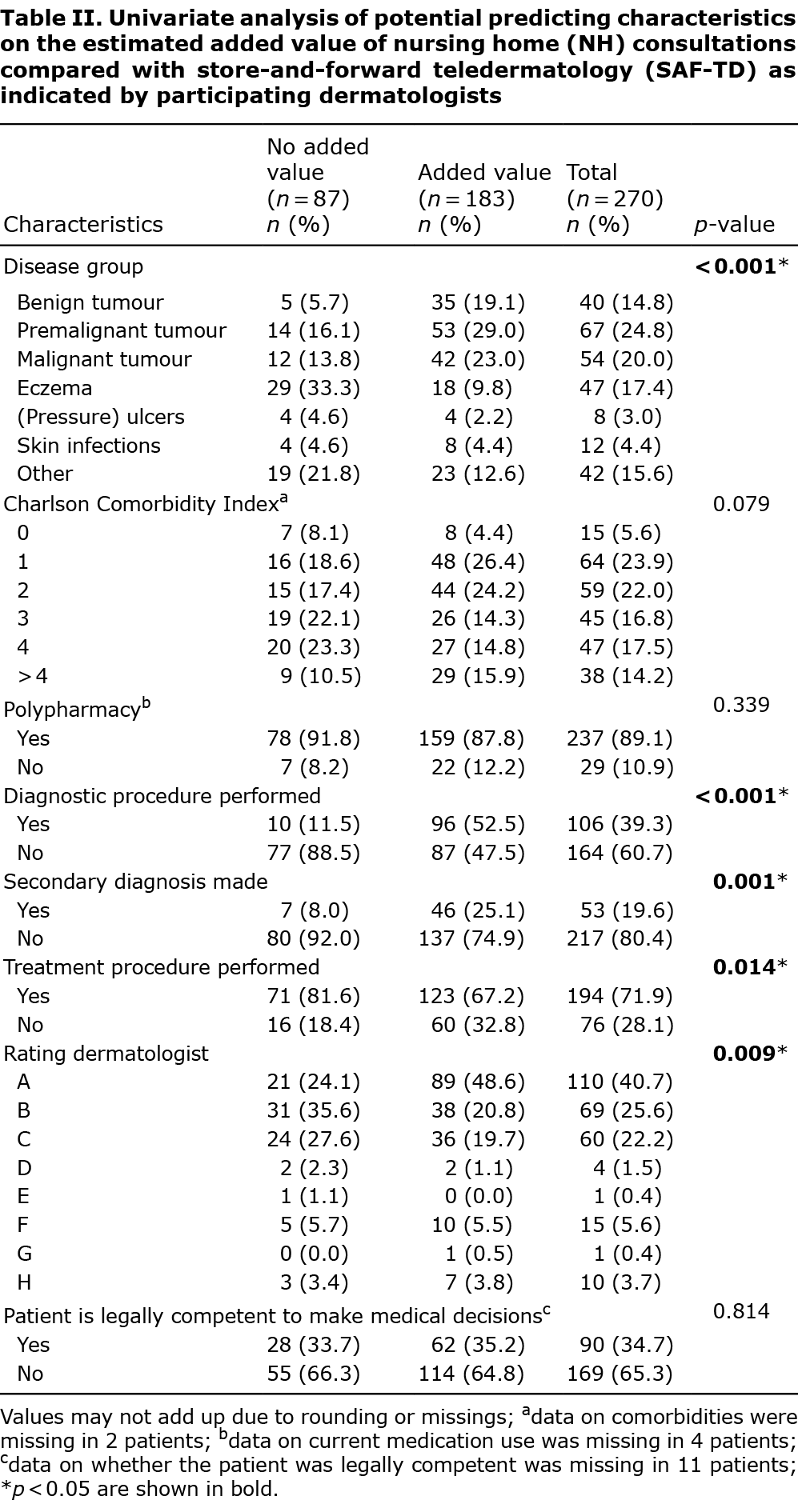
When the participating dermatologists indicated the estimated value of live NH consultations compared with SAF-TD on the Likert scale the median score was 4 (range 1–5). After categorizing the scores into 2 groups (“no added value” and “added value”), 183 NH visits (67.8%) were scored to be of “added value” and 87 (32.2%) visits were scored to have “no added value” (Table II).
When asked whether they would have advised the same policy if they had only been approached by SAF-TD (“yes”, “no” or “not sure”) instead of the LC in the NH, in 35.6% (n = 96) of the cases the dermatologists stated that they would not have advised the same policy. In 30 LC in NHs (11.1%) the dermatologists indicated they were not sure and in 144 (53.3%) of the LC they stated they would still have advised the same policy.
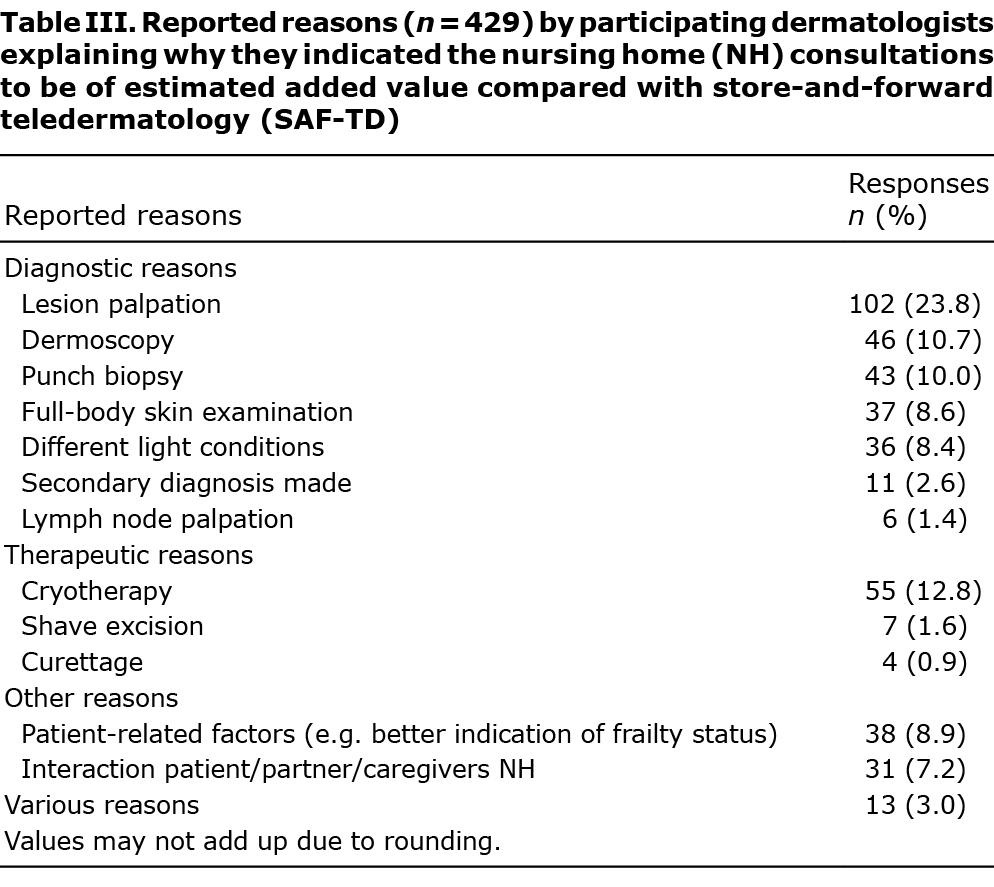
In total, 429 reasons for added value were provided in the open-ended question regarding the consultation evaluation. These reasons were further categorized as shown in Table III. Most stated reasons were the possibility of lesion palpation (n = 102; 23.8%), using cryotherapy (n = 55; 12.8%), using dermoscopy (n = 46; 10.7%), and taking a punch biopsy (n = 43; 10.0%) during the LC in the NH. Other reasons accounted for 19.1% (n = 82) of the reasons for added value, including contextual patient aspects.
Univariate analysis. Table II provides an overview of the univariate analysis of the different characteristics further stratified for the added value score. In 5 characteristics a significant difference was found between the “no added value” and “added value” groups: disease group (p < 0.001), whether a diagnostic procedure was performed (p < 0.001), whether a secondary diagnosis was made (p = 0.001), whether a treatment procedure was performed (p = 0.014), and the rating dermatologist (p = 0.009). There was no significant difference between the added value groups for the other characteristics (Charlson Comorbidity Index, polypharmacy, or whether the patient was legally competent to make medical decisions).
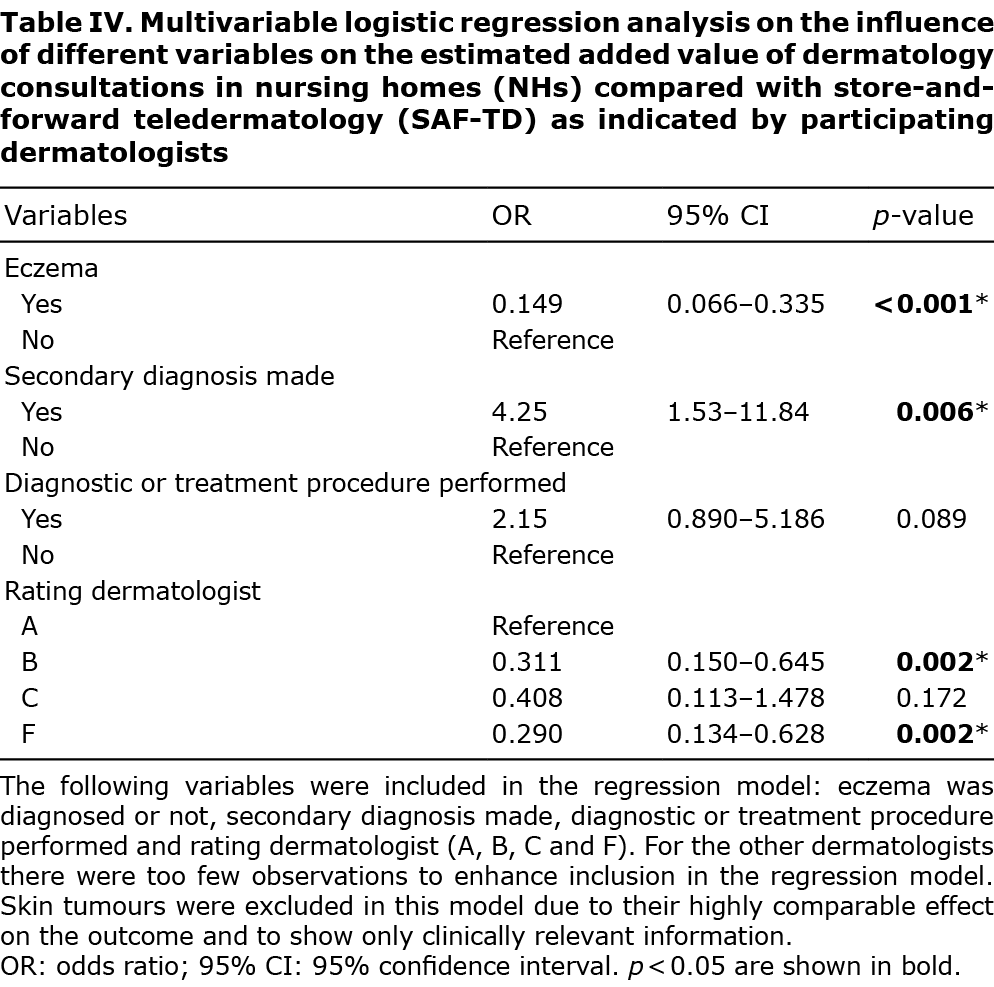
Multivariable analysis. Subsequently, a multivariable logistic regression analysis was performed to study the characteristics of significant influence on the added value score (“no added value” vs “added value”) as identified in the univariate analysis in more detail. Two multivariable regression models were constructed, as described above.
The first model showed that the diagnosis skin tumour (benign: odds ratio (OR) 27.6; 95% confidence interval (95% CI) 7.3–104.3, premalignant: OR 12.2; 95% CI 4.1–36.0 and malignant: OR 10.1; 95% CI 3.3–30.5) is a strong predictor for the outcome “added value” compared with the diagnosis of eczema. Furthermore, performing a diagnostic or treatment procedure during the consultation also predicted an added value of the LC as estimated by the dermatologist (OR 3.3; 95% CI 1.1–9.3). The effect of a secondary diagnosis during the consultation shows no statistical significant influence on the outcome (OR 2.6; 95% CI 0.9–7.9).
The second model (presented in more detail in Table IV) showed that, when simplifying the model by reducing the number of variables, the effect on the added value estimated by the dermatologist of performing a diagnostic or treatment procedure during the consultation was weakened (OR 2.1; 95% CI 0.9–5.2). In contrast, the effect of a secondary diagnosis became more relevant (OR 4.3; 95% CI 1.5–11.8 vs in the first model: OR 2.6; 95% CI 0.9–7.9). However, the diagnosis eczema is a predictor for no added value of a LC (OR 0.1; 95% CI 0.1–0.3). Both models show a comparable impact on the outcome by the rating dermatologists (Table IV).
DISCUSSION
The results of this study show that skin tumours (both benign and (pre)malignant) (n = 161; 59.6%) followed by eczema (n = 47; 17.4%) are the major reasons for dermatologists to visit a NH for LC. In 67.8% (n = 183) of LCs, the dermatologists reported that the LC was estimated to be of added value compared with SAF-TD.
These findings generally correspond to the prevalences of different skin diseases found in previous studies (7, 9–13). However, a higher prevalence of skin cancer and a lower prevalence of skin infections was found in the current study. A possible explanation is that the threshold for referral to a dermatologist for skin lesions suspicious for skin cancer, is lower compared with skin infections, because elderly care physicians feel less experienced in diagnosing and treating skin cancer and that there is also often a lack of facilities to do so (14, 15). For elderly care physicians it might also be relevant to consult a dermatologist to further estimate the impact of a suspicious skin lesion on the quality of life of a patient.
This study found that the estimated added value of LC compared with SAF-TD by dermatologists is higher for skin tumours compared with eczema. Regression analysis indicates that the possibility of using direct diagnostics (e.g. palpation, dermoscopy, punch biopsy) or treatment (e.g. cryotherapy) are factors increasing the added value score in this study. This might be explained by several factors. Direct diagnostics or treatment are more often used in case of a (pre)malignant skin lesion compared with eczema. Furthermore, it was shown that SAF-TD has very limited applicability in case of skin tumours, possibly due to the lack of palpation, and the difficulty of diagnosing pigmented tumours from SAF-TD (17, 22)
Noting a secondary diagnosis during LC was also shown to increase the added value, especially when a (pre)malignant tumour was noted, which accounted for 58.8% (n = 31) of the secondary diagnoses (n = 52). Regression analysis revealed that the outcome is also influenced by the rating dermatologists, which seems to be partially explained by the extent of diagnostic and treatment procedures performed by the dermatologists during the NH consultations (e.g. some participating dermatologists never perform punch biopsies during their consultations). Other influential factors (e.g. skills of elderly care physicians, treating facilities in the NH) and contextual aspects of the patients have not been taking into account in this analysis and might reduce the effect found in the current study.
As shown by the results of this study, it it noteworthy that not only the technical aspects (e.g. facilities to treat and diagnose) of a LC are considered important, but also the contextual aspects of the patient. In the frail NH population, a patient-centered and holistic approach is considered to be of vital importance to provide the most appropriate healthcare. Therefore, interaction with the patient, their relatives and/or healthcare professionals is important, to properly identify relevant contextual factors, and estimate the possibility and feasibility of certain medical decisions. These aspects have an impact on management decisions, which was also indicated by the finding that 35.6% (n = 96) of the dermatologists estimated that they would not have advised the same policy when they had only been approached by SAF-TD.
Based on the results of this study we suggest using TD as a triage tool for all NH patients where dermatological consultation is desired. In this scenario LC of low added value could possibly be reduced by 32,2% (n = 87). Through innovations such as teledermoscopy or artificial intelligence (AI) the value of SAF-TD for skin tumours could be further improved, which could further reduce consultations of low added value. Considering 59.6% of the LCs were due to skin tumours for which (tele)dermoscopy is an essential diagnostic tool, (tele)dermoscopy could potentially substantially reduce the need for LC. In this context the value of realtime-TD (e.g. using smart glasses) to further assist in patient-centered care should also be assessed. Furthermore, a direct (randomized) comparison of LC vs TD could be beneficial to gain more insight into potential advantages and optimal triage.
Study limitations
Potential limitations to this study are the possible misinterpretation of some questions, and the self-assessing character of the questionnaire. To prevent misinterpretation, the questionnaire was pre-tested as described and, in addition, every participating dermatologist received comprehensive instructions on how to use the questionnaire. Another limitation is that, based on the specific population characteristics in this study (e.g. skin type distribution, healthcare system, dermatologist’s experience visiting NHs, or availability of (tele)dermoscopy), the generalizability and validity of the results will vary.
Conclusion
To provide the most optimally organized and efficient dermatological care in NHs, TD and LCs go hand in hand. LCs are estimated to have added value over SAF-TD in two-thirds of cases, especially in patients with skin tumours. Based on the results of this study, using SAF-TD as a triage tool potentially reduces the need for additional LC in one-third of patients. Therefore, TD as a triage tool could help enable more efficient dermatological healthcare provision and it could be helpful if elderly care physicians use SAF-TD more frequently. Future research on the (cost)effectiveness of SAF-TD as a triage tool and implementation in teledermoscopy and real-time TD is recommended.
ACKNOWLEDGEMENTS
The authors are grateful to all the participating patients and physicians.
Due to the design and nature of this study the medical ethics committee (Arnhem-Nijmegen, the Netherlands) waived the need for formal approval.
The authors have no conflicts of interest to declare.
REFERENCES
- United Nations. World population prospects 2019: highlights. New York: Department of Economic and Social Affairs, Population Division; 2019.
- World Health Organization (WHO). Multimorbidity. Geneva: WHO; 2016.
- Statistics Netherlands (CBS). Prognose bevolking; kerncijfers (Population forecast; key figures), 2017-2060. 2017. In Dutch. Available from: https://www.cbs.nl/nl-nl/cijfers/detail/83783NED.
- National Institute for Public Health and the Environment (RIVM). Aandoeningen, welke aandoeningen hebben we in de toekomst? Trendscenario. 2017. In Dutch. Available from: https://www.vtv2018.nl/aandoeningen.
- Kottner J, Rahn Y, Blume-Peytavi U, Lahmann N. Skin care practice in German nursing homes: a German-wide cross-sectional study. J Dtsch Dermatol Ges 2013; 11: 329–336.
- Kim EK, Kim HO, Park YM, Park CJ, Yu DS, Lee JY. Prevalence and risk factors of depression in geriatric patients with dermatological diseases. Ann Dermatol 2013; 25: 278–284.
- Hahnel E, Blume-Peytavi U, Trojahn C, Dobos G, Jahnke I, Kanti V, et al. Prevalence and associated factors of skin diseases in aged nursing home residents: a multicentre prevalence study. BMJ Open 2017; 7: e018283.
- Lubeek SFK. Geriatric dermatology: optimising care in frail older adults. Nigmegen: Radboud University Medical Center; 2017.
- Roodsari-Rahmati M, Malekzad F. The prevalence of skin diseases among nursing-home patients in North Tehran. Clin Dermatol 2008; 24: 43–46.
- Chan S. Prevalence of skin problems in elderly homes residents in Hong Kong. Hong Kong J Dermatol Venereol 2006; 14: 66–70.
- Smith DR, Leggat PA. Prevalence of skin disease among the elderly in different clinical environments. Australas J Ageing 2005; 24: 71–76.
- Akdeniz M, Hahnel E, Ulrich C, Blume-Peytavi U, Kottner J. Prevalence and associated factors of skin cancer in aged nursing home residents: a multicenter prevalence study. PLoS One 2019; 14: e0215379.
- Kilic A, Gul U, Aslan E, Soylu S. Dermatological findings in the senior population of nursing homes in Turkey. Arch Gerontol Geriatr 2008; 47: 93–98.
- Lubeek SF, van der Geer ER, van Gelder MM, Koopmans RT, van de Kerkhof PC, Gerritsen MJ. Current dermatologic care in Dutch nursing homes and possible improvements: a nationwide survey. J Am Med Dir Assoc 2015; 16: 714.e711–716.
- Lubeek SF, van Gelder MM, van der Geer ER, van de Kerkhof PC, Gerritsen MJ. Skin cancer care in institutionalized elderly in the Netherlands: a nationwide study on the role of nursing home physicians. J Eur Acad Dermatol Venereol 2016; 30: e236–e237.
- Lubeek SF, Van Der Geer ER, Van Gelder MM, Van De Kerkhof PC, Gerritsen MJ. Dermatologic care of institutionalized elderly patients: a survey among dermatologists in the Netherlands. Eur J Dermatol 2015; 25: 606–612.
- Warshaw EM, Hillman YJ, Greer NL, Hagel EM, MacDonald R, Rutks IR, et al. Teledermatology for diagnosis and management of skin conditions: a systematic review. J Am Acad Dermatol 2011; 64: 759–772.
- Lubeek SF, Mommers RJ, van der Geer ER, van de Kerkhof PC, Gerritsen MJ. [Teledermatology within Dutch nursing homes]. Tijdschr Gerontol Geriatr 2016; 47: 117–123 (in Dutch).
- Schröder AK, Fassmer AM, Allers K, Hoffmann F. Needs and availability of medical specialists’ and allied health professionals’ visits in German nursing homes: a cross-sectional study of nursing home staff. BMC Health Serv Res 2020; 20: 332.
- Yong AMY, Leung AJ, Chandran NS. A dermatology health services study of nursing homes in Singapore. Singapore Med J 2020; 61: 661–664.
- von Stuelpnagel CC, Petersen J, Augustin M, Sommer R. [Dermatologische Versorgung von älteren Menschen mit Psoriasis vor und nach Eintritt in ein Pflegeheim. Eine qualitative Analyse aus Sicht von medizinischen Versorgern]. Dermatologie (Heidelb) 2022; 73: 627–633.
- Finnane A, Dallest K, Janda M, Soyer HP. Teledermatology for the diagnosis and management of skin cancer: a systematic review. JAMA Dermatol 2017; 153: 319–327.
- Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol 2004; 57: 1288–1294.
- Dutch College of General Practitioners (NHG), Nederlandse Vereniging voor Klinische Geriatrie, Orde van Medisch Specialisten. Multidisciplinary Guideline Polypharmacy in elderly. Utrecht: Dutch College of General Practitioners, 2012. In Dutch. Available from: https://www.nhg.org/sites/default/files/content/nhg_org/uploads/polyfarmacie_bij_ouderen.pdf.