Facial Papules and Renal Carcinoma: A Quiz
Niccolò Capurro1, Silvia Riva1*, Mattia Fabio Molle1, Emanuele Cozzani1, Antonio Guadagno2 and Aurora Parodi1
1Section of Dermatology, DISSAL, San Martino-IST Polyclinic Hospital, University of Genoa, IT-16132 Genoa, and 2Pathology Unit IRCC Ospedale Policlinico “San Martino” Genoa, Italy. *E-mail: dr.silviariva@gmail.com
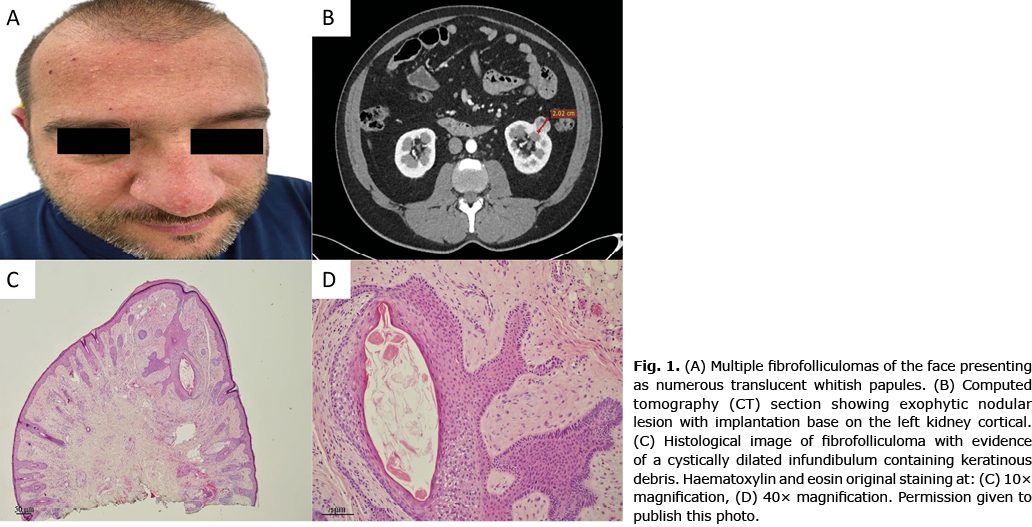
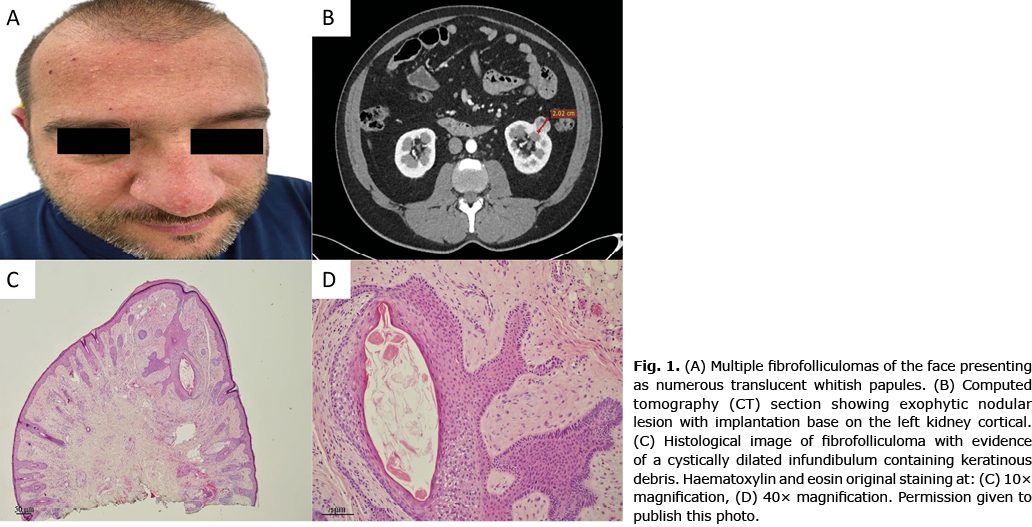
A 43-year-old white Caucasian patient presented to Clinica Dermatologia – IRCCS Ospedale Policlinico San Martino, Genova for a mole check-up. During the physical examination numerous translucent white, asymptomatic papules were noted, located mainly on the nose, cheeks and forehead (Fig. 1A). The patient reported their appearance and progressive increase in number and size over a period of approximately 15 years. The patient also referred the presence of similar lesions on his father’s face, who had died at the age of 68 years from renal carcinoma. Histological evaluation revealed a vertically oriented infundibulum-follicular structure, slightly dilated and mingled with corneocytes. An abundant stroma was present between the epithelial cords, composed of delicately fibrillar collagen mixed with mucin. Histopathology diagnosis was consistent with fibrofolliculoma (Fig. 1C). The molecular analysis of the FLCN gene has found the presence of the variant (class 5) c.91C>T; p. (Gln31Ter). Abdominal ultrasound was performed, showing a hyperechogenic exocortical nodular formation in the left kidney. Computed tomography (CT) confirmed the presence of a 2.02-cm solid renal lesion and showed numerous intrapulmonary emphysematous bullae (Fig. 1B).
What is your diagnosis? See next page for answer.
Facial Papules and Renal Carcinoma: A Commentary
Acta Derm Venereol 2022; 102: adv00824.
DOI: 10.2340/actadv.v102.4575
Diagnosis: Birt-Hogg-Dubé syndrome
Birt-Hogg-Dubé syndrome (BHDS) is a rare, autosomal, dominant inherited monogenic disorder characterized by the development of skin lesions (fibrofolliculomas, trichodiscomas and acrochordons) pulmonary emphysematous bullae leading to early spontaneous pneumothorax, and a predisposition to renal cell carcinoma. BHDS is caused by mutations in the folliculin gene (FLCN) located on the short arm of chromosome 17 (17p11.2) (1).
The worldwide prevalence of BHDS is 2 cases per million, and as of 2016, 612 affected families have been described globally, including 15 in Italy. However, BHDS is believed to be an underdiagnosed entity, primarily because of physicians’ unfamiliarity with this syndrome (2). In particular, dermatologists must be aware of the existence of BHDS because skin lesions are present in almost all patients and are the earliest clinical sign, becoming evident at approximately 20 years of age (3).
Therefore, it is important to emphasize that the presence of multiple papular skin lesions, especially on the face, even if asymptomatic and underestimated by the patient, should always be included in in-depth diagnostic investigations as possible signs of syndromic pictures, including BHDS, especially if present in more individuals of the same family.
In case of multiple whitish papules on the face and nose, the differential diagnosis should also encompass other genodermatoses, including Cowden syndrome, which is characterized by trichilemmomas of the face, Brooke-Spiegler syndrome, which is associated with facial trichoepitheliomas, and tuberous sclerosis complex or multiple endocrine neoplasia type 1 (MEN1), both of these being related to angiofibromas of the face (4).
Early diagnosis is of BHDS paramount importance to minimize the risk of developing advanced renal neoplasia, as happened to the current patient, who underwent early partial nephrectomy with histological diagnosis of clear cell renal cell carcinoma.
Investigations should be extended to the patient’s offspring, who have a 50% risk of inheriting the syndrome regardless of sex. However, the American Society of Clinical Oncology (ASCO) recommends delaying genetic testing in at-risk individuals until they reach the age of 18 years and are able to make informed decisions about genetic testing (5).
At 6 months after surgery, the patient is in excellent health and undergoes regular follow-up monitoring.
This case demonstrates how dermatologists can prove critical not only to detect skin cancers at an early stage, but also to be supportive in the diagnosis of complex, systemic or genetic diseases that often have concomitant skin manifestations.
The authors have no conflicts of interest to declare.
REFERENCES
- Sattler EC, Steinlein OK. Birt-Hogg-Dubé Syndrome. 2006 Feb 27 [updated 2020 Jan 30]. In: Adam MP, Everman DB, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, editors. GeneReviews®. Seattle (WA): University of Washington, Seattle; 1993–2022.
- Muller ME, Daccord C, Taffé P, Lazor R. Prevalence of Birt-Hogg-Dubé syndrome determined through epidemiological data on spontaneous pneumothorax and Bayes Theorem. Front Med 2021; 8: 631168.
- Menko FH, van Steensel MA, Giraud S, Friis-Hansen L, Richard S, Ungari S, et al. Birt-Hogg-Dubé syndrome: diagnosis and management. Lancet Oncol 2009; 10: 1199–1206.
- Schierbeck J, Vestergaard T, Bygum A. Skin cancer associated genodermatoses: a literature review. Acta Derm Venereol 2019; 99: 360–369.
- Furuya M, Hasumi H, Yao M, Nagashima Y. Birt-Hogg-Dubé syndrome-associated renal cell carcinoma: histopathological features and diagnostic conundrum. Cancer Sci 2020; 111: 15–22.