QUIZ SECTION
A Light-red Nodule on the Jaw: A Quiz
Aya NAKAGAWA and Kazunari SUGITA
Division of Dermatology, Department of Internal Medicine, Faculty of Medicine, Saga University, Nabeshima 5-1-1, Saga, Japan. E-mail: xxayaochi@ybb.ne.jp
Citation: Acta Derm Venereol 2023; 103: adv00873. DOI: https://doi.org/10.2340/actadv.v103.5305.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Feb 16, 2023
An 88-year-old woman was referred to our hospital with a painless, light-red nodule on her left jaw. She was living in a nursing home, and the staff had noticed a haemorrhage of the lesion 2 weeks before the first presentation to our hospital. She had no fever, pain or other symptoms. Physical examination revealed a light-red nodule on her left jaw; it was adhesive to the surrounding tissue and 10 mm in diameter (Fig. 1). She had a history of diabetes mellitus, hypertension, hyperlipidaemia, brain infarction, and osteoporosis. Histopathological examination of the nodule revealed tissue granulation and infiltration of inflammatory cells. No cancer cells were observed in any of the specimens (Fig. 2).

Fig. 1. A light-red nodule, 10 mm in diameter on the left jaw.

Fig. 2. (a) Skin biopsy shows granulation tissue and inflammatory cell infiltration. (b) High-power view of (a) shows mixed cellular infiltrate mainly consists of neutrophils, histiocytes, and plasma cells in the dermis. Haematoxylin-eosin, original magnification: (a) ×10; (b) ×20.
What is your diagnosis? See next page for answer.
ANSWERS TO QUIZ
A Light-red Nodule on the Jaw: A Commentary
Diagnosis: Bisphosphonate-related osteonecrosis of the jaw (BRONJ)
The patient had been taking alendronic acid for 27 months for osteoporosis before she was referred to our hospital. She had no history of radiation exposure to the jawbone, recent dental treatment, or cancer metastasis to the jawbone. Bisphosphonate-related osteonecrosis of the jaw (BRONJ) was suspected, but squamous cell carcinoma and external dental fistula were considered as differential diagnoses. Histopathological examination excluded the presence of cancer cells and squamous cell carcinoma; however, the possibility of an external dental fistula remained because of the presence of granulation tissue. Dental examination revealed an enlarged periodontal pocket of the second left lower molar and an oral fistula. During cleansing of the oral fistula, drainage from the skin side of the fistula was observed. Computed tomography revealed bone sclerosis and osteolytic changes in the mandible (Fig. 3). Based on these findings, a final diagnosis of BRONJ was made because the patient met all the diagnostic criteria for BRONJ, including an intraoral fistula, a history of oral bisphosphonate therapy, and no history of radiation therapy or cancer (1).
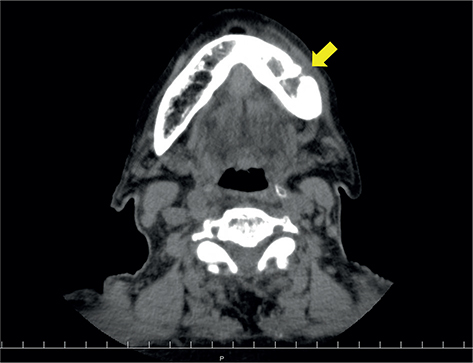
Fig. 3. Computed tomography of the mandible. Arrow indicates bone sclerosis and osteolytic change in the mandible.
BRONJ is included in the concept of medication-related osteonecrosis of the jaw (MRONJ). MRONJ is known to include anti-resorptive agent-related osteonecrosis of the jaw (ARONJ) and antiangiogenic agent-related osteonecrosis of the jaw (2). ARONJ is classified into BRONJ and denosumab-related osteonecrosis of the jaw (2). This case favoured the diagnosis of BRONJ because the patient had no history of denosumab use, but a history of bisphosphonate therapy.
Bisphosphonates are used to treat various conditions, such as hypercalcemia in patients with malignancies, and to prevent skeletal-related events in patients with multiple myeloma, and osteoporosis. Bisphosphonates have a strong affinity for hydroxyapatite; hence, 50% of the administered bisphosphonates accumulate in the bone matrix and remain there for a long time (3). After incorporation into the bone, bisphosphonates are acquired by osteoclasts and inhibit cellular function and survival (3).
The risk of BRONJ among osteoporosis patients treated with bisphosphonates varies between 0.02% and 0.05% (1). The mean duration of oral bisphosphonate therapy before the development of osteonecrosis of the jawbone is 42.6 months, and the most common trigger is dental extraction. However, in the current patient, the onset of osteonecrosis of the jaw was 15 months shorter than the mean duration after oral bisphosphonate therapy, even though the patient had no history of dental extraction. It has been reported that (4), risk factors for BRONJ include, for example, anticancer drugs, corticosteroid use, poor oral hygiene, and diabetes mellitus. Hence, in addition to bisphosphonates, the presence of diabetes mellitus and poor oral hygiene due to dentures may have contributed to the onset of osteonecrosis of the jawbone. According to the previous reports of BRONJ, orocutaneous fistulas or exposed bone can occur even in the absence of pain, as presented in the current case (5–7). Therefore, attention is required to both the bone exposure and the fistula and tumour formation on the skin side.
In conclusion, for patients presenting with a nodule in the jaw, the possibility of BRONJ should be considered, and the patient’s medical history and oral cavity should be examined.
REFERENCES
- Ruggiero SL, Dodson TB, Aghaloo T, Carlson ER, Ward BB, Kademani D. American Association of Oral and Maxillofacial Surgeons’ position paper on Medication-Related Osteonecrosis of the Jaws – 2022 update. J Oral Maxillofac Surg 2022; 80: 920–943.
- AlDhalaan NA, BaQais A, Al-Omar A. Medication-related osteonecrosis of the jaw: a review. Cureus 2020; 12: e6944.
- Shibahara T. Antiresorptive agent-related osteonecrosis of the Jaw (ARONJ): a twist of fate in the bone. Tohoku J Exp Med 2019; 247: 75–86.
- Shibahara T, Morikawa T, Yago K, Kishimoto H, Imai Y, Kurita K. National survey on bisphosphonate-related osteonecrosis of the Jaws in Japan. J Oral Maxillofac Surg 2018; 76: 2105-2112.
- Kang HS, Lee JW, Kim JS. Dental sinus tracts mimicking scrofuloderma: cutaneous presentation of underlying bisphosphonate-related osteonecrosis of the jaw. Clin Exp Dermatol 2011; 36: 624–627.
- Truong SV, Chang LC, Berger TG. Bisphosphonate-related osteonecrosis of the jaw presenting as a cutaneous dental sinus tract: A case report and review of the literature. J Am Acad Dermatol 2010; 62: 672–676.
- McCusker S, May C. A cutaneous presentation of bisphosphonate-related osteonecrosis of the jaw. Clin Exp Dermatol 2020; 45: 932–934.