SHORT COMMUNICATION
Dual Interleukin-4/Interleukin-13 Blocker-induced Arthralgia Treated Successfully with Upadacitinib in a Patient with Atopic Dermatitis
Takayuki TANJI, Daisuke WATABE*, Nobuyuki ARAKAWA, Hirofumi KAMADA and Hiroo AMANO
Department of Dermatology, Iwate Medical University School of Medicine, 2-1-1, Idaidori, Yahaba-cho, Shiwa-gun, Iwate 028-3695, Japan. *E-mail: dwatabe@iwate-med.ac.jp
Citation: Acta Derm Venereol 2023; 103: adv5326. DOI https://doi.org/10.2340/actadv.v103.5326.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Mar 28, 2023; Published: Apr 27, 2023
INTRODUCTION
Atopic dermatitis (AD) is a chronic inflammatory disease driven by type 2 inflammation. Recently, upadacitinib has been used for treatment of AD, and has also been approved for psoriatic arthritis. Upadacitinib specifically blocks the signal of several inflammatory cytokines (such as interleukin (IL)-31, IL-4, IL-13, and thymic stromal lymphopoietin, etc.), which play a central role in the pathophysiology of AD by inhibiting the Janus kinase 1 (JAK1) pathway.
We report here a case of arthralgia during treatment with a dual IL-4/IL-13 blocker (dupilumab), which was treated successfully with an oral JAK inhibitor (upadacitinib) in a Japanese female patient with a 10-year history of AD.
CASE REPORT
The patient began treatment with dupilumab because of refractory AD. Eczema Area and Severity Index (EASI), Investigator’s Global Assessment (IGA), and body surface area (BSA) were 21.4, 3, and 40%, respectively. Subsequently, her skin rash and itch improved markedly, but 2 months after the initiation of dupilumab, she complained of pains in her shoulders, fingers, and knee joints and was referred to our clinic. She had no history of musculoskeletal or rheumatic disease, and her serum C-reactive protein, rheumatoid factor, and anti-cyclic citrullinated peptide antibodies were negative. Matrix metalloproteinase-3 was within normal limits (40 ng/ml). X-ray examinations revealed inflammation in the distal interphalangeal (DIP) joints of the bilateral little toes (Fig. 1A) and ultrasound showed inflammation at the Achilles tendon attachment (Fig. 1B, C). The Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) at that time was 8.60. The patient was diagnosed as having arthralgia due to dupilumab, which was then discontinued and she was treated with oral steroids. However, these treatments were ineffective. Subsequently, the skin lesions and itching worsened, and the arthralgia worsened to such an extent that the patient was unable to raise her arms and grasp her own hands. Treatment with upadacitinib 15 mg daily was commenced. After the start of treatment, the itching and arthralgia improved dramatically and the BASDAI decreased to 0. The arthralgia was well controlled with upadacitinib and the skin lesions also disappeared.
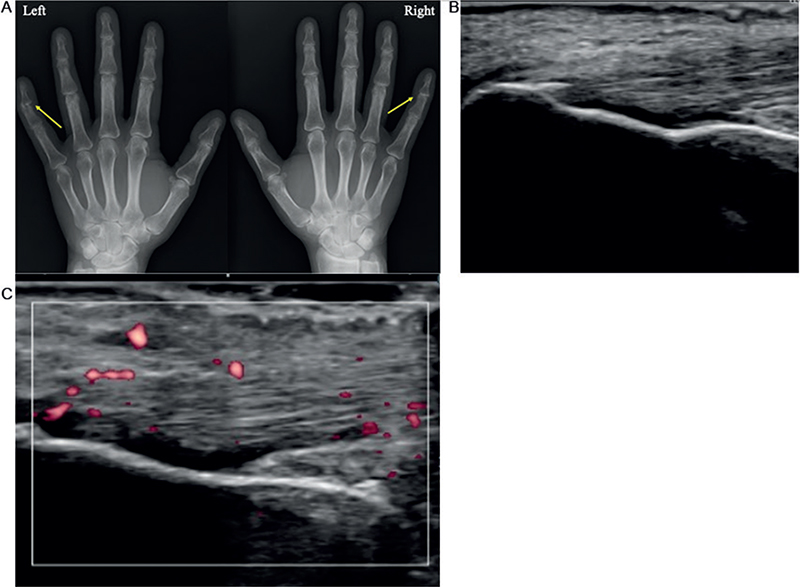
Fig. 1. (A) X-ray views show inflammation in the distal interphalangeal (DIP) joints of the bilateral little toes. (B, C) Ultrasound findings 2 months after dupilumab therapy. The Achilles tendon attachment enthesis. Longitudinal scan. The Achilles tendon attachment appears (B) hypoechoic and (C) thickened with Doppler signals at the enthesis.
DISCUSSION
JAK inhibitors exert immunosuppressive and antiproliferative effects by inhibiting a conserved signalling pathway, the JAK–signal transducer and activator of transcription (STAT) pathway. The JAKs comprise a group of 4 receptor-associated kinases (JAK1, JAK2, JAK3, and tyrosine kinase 2) that mediate cytokine-stimulated transcriptional changes by phosphorylation of the STAT family of transcription factors (1). Upadacitinib is an oral drug designed to inhibit JAK1 more selectively.
One of the adverse events of dupilumab is arthralgia (2). Although this is relatively rare, once it occurs the arthralgia is difficult to treat and currently no established treatment is available. It is not known why most patients with AD treated with IL-4/13 monoclonal antibody do not develop arthritis, as this would presumably upset the Th1/Th2 balance and cause a shift toward Th1 inflammation. Recent findings suggest that IL-4 and IL-13 may play an important role in downregulating the inflammatory processes underlying the pathogenesis of rheumatoid arthritis and may beneficially regulate the course of the disease. IL-4/IL-13 cytokines play a role in reducing the production of proinflammatory cytokines (IL-1β, IL-6, IL-8, TNF) and metalloproteinases in inflammatory arthritis (3). Neutralization of IL-4 leads to upregulation of a number of genes linked to Th1 trafficking. Moreover, IL-4 neutralization leads to an early increase in Th1 cell recruitment to inflamed tissue (4). Based on the above findings, we consider that inhibition of IL-4/13 by dupilumab contributes to the development of arthritis by increasing the expression of proinflammatory cytokines, including Th1 cytokines. So far, non-steroidal anti-inflammatory drugs (NSAIDs), prednisolone and/or methotrexate have been tried for management for the arthralgia. To date, only 7 reports, including the current one, have mentioned joint symptoms (5–8) (Table I). Among treatment interventions, prednisolone and methotrexate were administered in some cases in addition to analgesics (patients 1 and 5). Only the current case was treated with upadacitinib.
| Patient 1 (5) | Patient 2 (6) | Patient 3 (6) | Patient 4 (6) | Patient 5 (7) | Patient 6 (8) | Our case | |
| Age, Sex | 38, F | 40, M | 48, M | 68, F | 54, M | 55, M | 55, F |
| Area with arthralgia | Ankles, knees, hips, elbows | Generalized (knees, ankles, right shoulder, hands, wrists, achilles) | Bilateral achilles, left thumb, ankles, knees, left wrist, metacar-popha-langeal joint | Generalized | Distal and proximal interphalangeal, elbows, knees, left shoulder, ankles | Shoulders, knees | Hands, achilles tendon attachment |
| Radiological findings | X-ray: swollen tissue, without erosions or osteoarthritis of the right ankle | US: bilateral synovitis of the wrists | US: left achilles peritendinitis MRI: left achilles tendinopathy | US: bilateral lateral epicondylitis | US: enthesitis at the lateral epicondyle of the bilateral humeri and the patellar tendons | US: not detected | X-ray: inflammation in the DIP joints of his bilateral little toes US: inflammation at the achilles tendon attachment |
| Dupilumab | Discontinuation | Discontinuation | Continuation | Discontinuation | Continuation | Discontinuation →Resumption |
Discontinuation |
| Treatment |
|
Naproxen | Celecoxib | - |
|
- | Upadacitinib |
| Response | Improvement | Poor | Partial improvement | Unchanged | Partial improvement | Improvement | Improvement |
| Onset after dupilumab initiation | A few days | 16 weeks | 6 weeks | 6 weeks | 2 months | A few days | 2 months |
| M: male; F: female; US: ultrasound; MRI: magnetic resonance imaging. | |||||||
Upadacitinib is a selective JAK1 inhibitor that was recently approved in Japan for treatment of AD. The pathogenesis of AD is believed to be, in part, a consequence of increased Th2 immunity driven by activation of JAK-mediated signalling pathways (9, 10). Recently, upadacitinib has been used for AD, and has also been approved for psoriatic arthritis. In addition to IL-4/13, inflammatory cytokines, such as IL-6 and interferon (IFN), are also mediated by JAK1 (1). In the current case, we speculated that the joint pain improved because upadacitinib suppressed these inflammatory cytokines.
In conclusion, this is the first case report of arthralgia in an AD patient during treatment with a dual IL-4/IL-13 blocker that was treated successfully with an oral JAK inhibitor (upadacitinib). Considering the pathology of AD, upadacitinib may be an effective treatment option for arthritis in patients with AD.
REFERENCES
- Cotter DG, Schairer D, Eichenfield L. Emerging therapies for atopic dermatitis: JAK inhibitors. J Am Acad Dermatol 2018; 78: 53–62.
- Thaçi D, Simpson EL, Deleuran M, Kataoka Y, Chen Z, Gadkari A, et al. Efficacy and safety of dupilumab monotherapy in adults with moderate-to-severe atopic dermatitis: a pooled analysis of two phase 3 randomized trials (LIBERTY AD SOLO 1 and LIBERTY AD SOLO 2). J Dermatol Sci 2019; 94: 266–275.
- Iwaszko M, Bialy S, Bogunia-Kubik K. Significance of interleukin (IL)-4 and IL-13 in inflammatory arthritis. Cells 2021; 10: 3000.
- Lazarski CA, Ford J, Katzman SD, Rosenberg AF, Fowell DJ. IL-4 attenuates Th1-associated chemokine expression and Th1 trafficking to inflamed tissues and limits pathogen clearance. PLoS One 2013; 8: e71949.
- de Wijs LEM, van der Waa JD, de Jong PHP, Hijnen DJ. Acute arthritis and arthralgia as an adverse drug reaction to dupilumab. Clin Exp Dermatol 2020; 45: 262–263.
- Willsmore ZN, Woolf RT, Hughes C, Menon B, Kirkham B, Smith CH, Pink AE. Development of inflammatory arthritis and enthesitis in patients on dupilumab: a case series. Br J Dermatol 2019; 181: 1068–1070.
- Ishibashi M, Honda T, Tabuchi Y, Kabashima K. Polyenthesitis during treatment with dupilumab for atopic dermatitis. J Eur Acad Dermatol Venereol 2020; 34: e319–e321.
- Arakawa N, Inoue T, Tanji T, Amano H. Development of arthralgia during treatment with dupilumab in a patient with atopic dermatitis. J Dermatol 2021; 48: e397–e398.
- Leung DY, Guttman-Yassky E. Deciphering the complexities of atopic dermatitis: shifting paradigms in treat-ment approaches. J Allergy Clin Immunol 2014; 134: 769–779.
- Damsky W, King BA. JAK inhibitors in dermatology: the promise of a new drug class. J Am Acad Dermatol 2017; 76: 736–744.