QUIZ SECTION
Three Cephalic Plaques: A Quiz
Muslih ALZAHRANI1, Franck VITTE2 and François AUBIN1
1Department of Dermatology, University Hospital, 3 Bd Fleming, FR-25000 Besançon, and 2CYPATH, Department of Pathology, Dijon, France. E-mail: francois.aubin@univ-fcomte.fr
Citation: Acta Derm Venereol 2023; 103: adv5336. DOI https://doi.org/10.2340/actadv.v103.5336.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Apr 6, 2023
INTRODUCTION
A 74-year-old male presented with 3 infiltrated angiomatous plaques on his vertex and forehead for 6 months (Fig. 1), which were asymptomatic. He had a medical history of prostate cancer in 2016. He had controlled plaque psoriasis and gout, a drug rash following allopurinol introduction, but no other notable history. Clinically, the patient had neither other similar plaques nor adenopathy. Biopsy showed a neutrophilic and eosinophilic infiltration in the superficial and mid-dermis, a Grenz zone, rich vascularization and multiple capillaries, a minimal perivascular fibrosis and an intact epidermis (Fig. 2). Laboratory tests revealed no eosinophilia or any other anomalies.
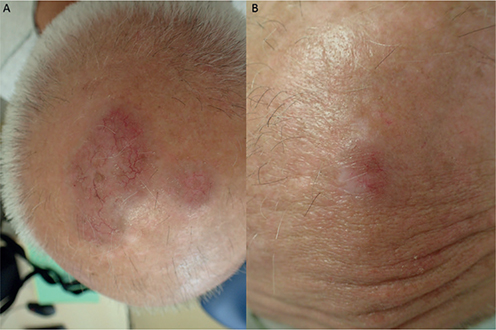
Fig. 1. (A) Two angiomatous plaques of the vertex. (B) Lesion of the forehead.
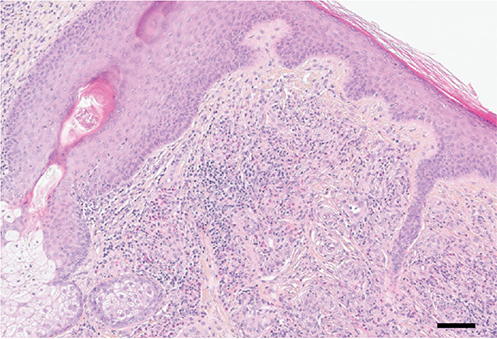
Fig. 2. Mixed dermal infiltrate formed by lymphocytes, histiocytes, plasma cells and neutrophils and a grenz zone (haematoxylin and eosin, original magnification ×400). Black bar; 100 µm.
What is your diagnosis? See next page for answer.
ANSWERS TO QUIZ
Three Cephalic Plaques: A Commentary
Diagnosis: Extrafacial granuloma faciale
Extrafacial granuloma faciale (GF) is a limited cutaneous disease of unknown aetiology (1). Middle-aged light-skinned men are commonly affected. GF is expressed by the presence of 1 or multiple plaque/nodule lesions of red-brown to violaceous colour with follicular accentuation and telangiectasia. Isolated facial presentation is commonly reported in the literature, but some patients also have associated extrafacial lesions. Approximately one-third of patients (31%) had isolated extrafacial lesions in a reported series of 32 patients (2). The trunk is usually the most frequently affected zone, followed by the upper extremities and the scalp (2). The pathophysiology of GF remains unknown, but it is probably related to sun exposure, as the lesions are generally found in photo-exposed areas. As diagnosis is based on histopathology, any well-demarcated infiltrated plaque should be biopsied (3). GF is frequently resistant to conventional therapy. Topical and injectable corticosteroids or tacrolimus and dapsone have been proposed, and combination with cryotherapy can also be used to obtain a better sustainable therapeutic response (2–4).
ACKNOWLEDGEMENTS
Ethics approval: The patient provided written informed consent for publication of his case details.
REFERENCES
- Deen J, Moloney TP, Muir J. Extrafacial granuloma faciale: a case report and brief review. Case Rep Dermatol 2017; 9: 79–85.
- Gupta L, Naik H, Kumar NM, Kar HK. Granuloma faciale with extrafacial involvement and response to tacrolimus. J Cutan Aesthet Surg 2012; 5: 150–152.
- De D, Kanwar AJ, Radotra BD, Gupta S. Extrafacial granuloma faciale: report of a case. J Eur Acad Dermatol Venereol 2007; 21: 1284–1286.
- Mookadam M, Mesinkovska N, Bridges AG. Evaluating the clinical and demographic features of extrafacial granuloma faciale. Cutis 2017; 100: E18–E22.