QUIZ SECTION
Violaceous Papules and Plaques on the Fingers during COVID-19: A Quiz
Michelangelo LA PLACA1, Lorenzo FUCCIO2, Alba GUGLIELMO1, Cosimo MISCIALI1 and Marco MONTAGNANI2
1Division of Dermatology, Department of Experimental, Diagnostic and Specialty Medicine and 2Gastroenterology and Endoscopy Unit, IRCCS Sant’Orsola Policlinic, University of Bologna, via Massarenti 1, IT-40138 Bologna, Italy. E-mail: michelangelo.laplaca@unibo.it.
Citation: Acta Derm Venereol 2023; 103: adv00863. DOI https://doi.org/10.2340/actadv.v103.5342.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Feb 7, 2023
INTRODUCTION
A 74-year-old Caucasian woman was admitted via emergency services with a 10-day history of intermittent fever (maximum 38.8°C), chills and fatigue. She reported a dry cough, dyspnoea, palpitations and chest pains. Her medical history revealed hypertension, and hysterectomy for endometrial cancer 7 years previously. Chest X-ray showed increased marking on the right basal site. Nasal swab for COVID-19 screening was performed and the patient was hospitalized on suspicion of COVID-19 infection. The nasal swab resulted positive for COVID-19. A further chest high-resolution computed tomography did not show interstitial pneumonitis. Sudden occurrence of cutaneous lesions on her hands was noted during hospitalization. A close-up view revealed well-defined, erythematous-violaceous papules and plaques on both dorsal hands and on the 2nd, 3rd and 4th left fingers (Fig. 1). A 4-mm punch biopsy from a lesion on her 2nd right finger revealed collections of epithelioid histiocytes and multinucleated giant cells (Fig. 2). Other routine blood tests, including angiotensin-converting enzyme, calcium, vitamin D, and hepatic parameters were within normal values. Her febrile symptoms resolved slowly, and a second nasal swab after 10 days was negative for COVID-19.

Fig. 1. Erythematous to purplish papules and plaques on (A) dorsal hands and (B) first and second left finger.
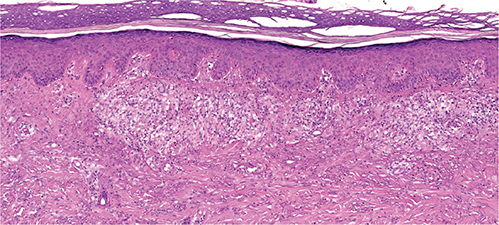
Fig. 2. Histological view showing collection of epithelioid histiocytes with sparse inflammatory infiltrate of lymphocytes in the superficial and mid-dermis. Basket woven and compact orthokeratosis are evident in the epidermis (haematoxylin and eosin (H&E) 10×).
What is your diagnosis? See next page for answer.
ANSWERS TO QUIZ
Violaceous Papules and Plaques on the Fingers during COVID-19: A Commentary
Diagnosis: Cutaneous sarcoidosis
Sarcoidosis is a multisystemic granulomatous disorder of unknown aetiology, characterized by the histological demonstration of a non-caseating granuloma and specific radiological features (1). Cutaneous involvement occurs in approximately 25% of cases, with the maculopapular form being the most common specific manifestation. However, a heterogeneous variety of clinical presentations, including psoriasiform, lichenoid, ichthyosiform or verrucous variants has been described. Nevertheless, the presence of pigmentation, ulceration, or atrophy, alone, or in the presence of these manifestations, has been referred to as the “great imitator” (2, 3).
Lupus pernio is one of the most typical clinical findings of cutaneous sarcoidosis, and is more commonly seen in black women with long-standing disease. Lupus pernio is characterized by indolent, red-purplish, or violaceous nodules and plaques with a typical appearance, primarily developing in areas affected by cold, including the nose, cheeks, and ears. It may at times affect the dorsal hands, finger, and toes, with lytic and cystic bone lesions on radiography. This form of cutaneous sarcoidosis may be recalcitrant to systemic corticosteroids and, in the most severe manifestations, can have disfiguring and mutilating consequences (1).
In Italy the coronavirus disease 2019 (COVID-19) pandemic reached its first epidemiological peak in March and April 2020. During that period, various cutaneous patterns, including maculopapular or urticarial rash, vesicular lesions, and pernio-like manifestations, were seen in people with high temperatures and respiratory symptoms (4, 5). The sudden occurrence of purplish plaques on the fingers and toes, resembling chilblains, has also been reported as a typical indicator, especially in children (6).
There are many reports of specific vasculitic findings, including chilblain-like acral pattern, livedo reticularis-like pattern, and purpuric “vasculitis” pattern (4–6). In particular, the occurrence of erythematous or purplish macules limited to the feet and/or hands of children or adolescents, with mild temperatures or without respiratory symptoms, has been referred to as a new correlated entity, termed “chilblain-COVID” (4–6). However, due to quarantine restrictions, testing for COVID-19 infection was not performed in most of these cases; hence a possible aetiological role for the virus has not been confirmed.
In addition, more recent, studies have failed to demonstrate this correlation: they conclude that a direct link between the cutaneous features resembling pernio-like lesions (or chilblain-like pattern) and COVID-19 cannot be confirmed (7, 8).
Classic chilblains (perniosis) consist of erythematous and oedematous lesions, sometimes ulcerated, which occur during cold or damp periods on the hands or feet and may be associated with connective tissue disease or haematological disorders (9).
We had a high level of suspicion that the cutaneous manifestations in our patient, positive for COVID-19, were chilblains. Only the demonstration of “naked” non-caseating granuloma on pathology specimens led to the final diagnosis of cutaneous sarcoidosis.
Lupus pernio, especially when the face is not involved, is an important differential diagnosis in patients evaluated for chilblain-like eruptions, and we suggest performing a biopsy in patients with sarcoidosis with unusual presentations.
REFERENCES
- Randhawa KS, Lee BW, Micali G, Benson BE, Schwartz RA. Cutaneous sarcoidosis: lupus pernio and more. Ital J Dermatol Venereol 2022; 157: 220–227.
- Maña J, Marcoval J. Skin manifestations of sarcoidosis. Presse Med 2012; 41: e355-e374.
- Barisani A, Negosanti M, La Placa M, Infusino SD, Misciali C, Sorci M, Patrizi A. Erythematous patches and pretibial ulcers: an uncommon presentation of cutaneous sarcoidosis. J Dtsch Dermatol Ges 2016; 14: 295–297.
- Marzano AV, Cassano N, Genovese G, Moltrasio C, Vena GA. Cutaneous manifestations in patients with COVID-19: a preliminary review of an emerging issue. Br J Dermatol 2020; 183: 431–442.
- Freeman EE, McMahon DE, Lipoff JB, Rosenbach M, Kovarik C, Desai SR, et al. The spectrum of Covid-19-associated dermatologic manifestations: an international registry of 716 patients from 31 countries. J Am Acad Dermatol 2020; 83: 1118–1129.
- Colonna C, Genovese G, Monzani NA, Picca M, Boggio F, Gianotti R, et al. Outbreak of chilblain-like acral lesions in children in the metropolitan area of Milan, Italy, during the COVID-19 pandemic. J Am Acad Dermatol 2020; 83: 965–969.
- Baeck M, Herman A. COVID toes: where do we stand with the current evidence? Int J Infect Dis 2021; 102: 53–55.
- Herman A, Peeters C, Verroken A, Tromme I, Tennstedt D, Marot L, et al. Evaluation of chilblains as a manifestation of the COVID-19 pandemic. JAMA Dermatology 2020; 156: 998–1003.
- Lambertini M, Vincenzi C, Dika E, La Placa M. chilblain lupus with nail involvement: a case report and a brief overview. Skin Appendage Disord 2018; 5: 42–45.