QUIZ SECTION
Unique Lesions on the Dorsum of the Hands: A Quiz
Delin RAN, Shengli CHEN, Xianmei LU, Guizhi ZHOU and Zhaoxia ZHANG*
Department of Dermatology, Shandong Provincial Hospital for Skin Diseases & Shandong Provincial Institute of Dermatology and Venereology, Shandong First Medical University & Shandong Academy of Medical Sciences, 27397 Jingshi Road, Jinan, Shandong Province, China. *E-mail: zhangzhaoxia0911@126.com
Citation: Acta Derm Venereal 2023; 103: adv00885. DOI: https://doi.org/10.2340/actadv.v103.5358.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Mar 9, 2023
A 67-year-old male presented with multiple papules and nodules on the dorsum of his hands without pruritus or ache, which had been present for the past 1 year. Treatment with corticosteroid ointment was ineffective. He had a history of ulcerative colitis and had been taking oral mesalazine for 6 years. He had no other comorbidities and was not taking any other drugs, and no underlying cause was identified for his condition.
Physical examination showed generalized papules and nodules, ranging from 4 to 10 mm diameter on the back of both hands (Fig. 1A), with no ulceration or tenderness. Laboratory investigations revealed peripheral mild leukocytosis (10.65×109/L, reference range <10×109/L), higher levels of erythrocyte sedimentation rate (ESR) (33 mm/h, reference range 0–20 mm/h) and C-reaction protein (CRP) (23.8 mg/L, reference range 0–8 mg/L). The levels of complement and immunoglobulin were normal. Tuberculosis-Interferon gamma Release Assay (TB-IGRA) and PCR test results for mycobacteria were all negative.
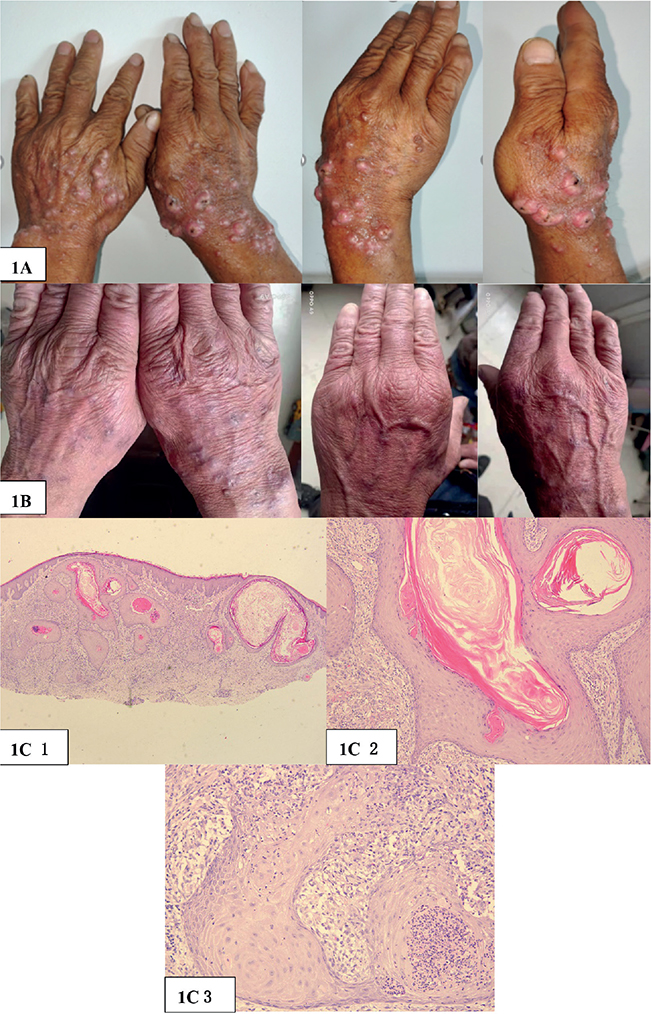
Fig. 1. (A) Before treatment: generalized papules and nodules, of rice grain to peanut size, on the back of both hands. (B) After treatment: the lesions subsided. (C) Histopathology revealed small neutrophil abscesses in the epidermis, infiltration of histiocytes, lymphocytes, multinucleated giant cells, and neutrophils were seen in superficial and deep layers of the dermis (1: haematoxylin and eosin (HE) 20×, 2: HE 100×, 3: HE 200×).
Skin biopsies were performed on the dorsum of each hand, and histopathology revealed hyperkeratosis together with pseudoepitheliomatous hyperplasia, small neutrophil abscesses in the epidermis, infiltration of histiocytes, lymphocytes, multinucleated giant cells, and neutrophils were seen in superficial and deep layers of the dermis (Fig. 1C). Periodic acid-Schiff (PAS) and acid-fast staining did not identify any microorganisms. In addition, tissue cultures for bacteria, fungus, and mycobacteria were all negative.
What is your diagnosis? See next page for answer
ANSWERS TO QUIZ
Unique Lesions on the Dorsum of the Hands: A Commentary
Diagnosis: Multiple keratoacanthoma
The patient was started on oral acitretin, 30 mg/day, and the lesions subsided gradually after 20 days of treatment. Acitretin was then tapered to 20 mg/day, and the cutaneous lesions resolved completely over a 3-month treatment (Fig. 1 B). He had no further recurrence of symptoms after 9 months’ follow‑up.
Keratoacanthoma (KA) is a special type of skin tumour, which occurs mainly in middle-aged and elderly people. Skin lesions are prone to occur in the sun-exposed areas, such as the face and the hands, with a rapid benign growth progress and self-healing tendency (1). Clinically, KA is divided into 3 types, including solitary, multiple and eruptive KA, solitary KA is the most common form, multiple KA may assume several clinical forms. The typical clinical manifestations were round or round-like papule nodules with a raised surface, the boundary was clear and necrosis was found in the centre (2).
Clinically, KA can be easily misdiagnosed with cutaneous squamous cell carcinoma or verruca vulgaris. Histopathological examination can help to make a differential diagnosis; however, it can sometimes be difficult to differentiate KA from squamous cell carcinoma. The typical pathological features of KA show a typical “crater”-like changes, keratin-filled crater with acanthosis and liplike or arch-like extensions in the depression of the epidermis (3). Surgical excision is recommended for single lesions, and the prognosis is fine. When KA are multiple or eruptive, surgical excision is unsuitable, and acitretin has been reported to be successful in treating KA because of its modulation of terminal differentiation of epidermal cells (4).
The current case has some unusual features. First, the tumours developed during a period of 1 year; this is atypical for a KA, which usually grow rapidly. Secondly, the clinical symptoms were not typical; there were papules and nodules without corneous material and necrosis in the lesions of the central, which could easily be misdiagnosed as several other skin disorders, such as nodular prurigo and infectious granuloma. Finally, pathological manifestations were rare, typical “crater”-like changes, keratin-filled craters with acanthosis or liplike or arch-like extensions in the depression of the epidermis were not shown. Although the pathological features were unusual, inflammatory cells infiltrating the dermis could also be present in KA, and the good reaction to acitretin supports the diagnosis of KA.
The patient was kept under long-term follow-up, since there is currently debate regarding KA; some researchers claim that KA is a benign tumour, while others argue that it is a subtype of squamous cell carcinoma that can regress (5). This case highlights this rare form of multiple KA with unusual clinical and pathological findings.
REFERENCES
- Mitri F, Hartschuh W, Toberer F. Multiple keratoacanthomas after a recent tattoo: a case report. Case Rep Dermatol 2021; 13: 23–27.
- Gleeson D, Cliff S, Das M. Eruptive keratoacanthomas associated with dupilumab therapy. Br J Dermatol 2022; 186: 376–377.
- Zhang SY, Han DW, Wang T, Liu YH. Multiple keratoacanthoma and oral lichen planus successfully treated with systemic retinoids and review of multiple keratoacanthoma associated with lichen planus. Int J Dermatol 2018; 57: 1125–1127.
- Mascitti H, Masson AD, Brunet-Possenti F, Bouaziz JD, Laly P, Mourad N, et al. Successful treatment of generalized eruptive keratoacanthoma of grzybowski with acitretin. Dermatol Ther (Heidelb) 2019; 9: 383–388.
- Zhu PQ, Wang Y. Multiple keratoacanthomas in a patient with myelodysplastic syndrome. Lancet Haematol 2021; 8: e94.