QUIZ SECTION
A Five-year-old Boy with a Thin Black Band on his Toenail: A Quiz
Bei LI, Lin MA and Ya-Bin ZHOU*
Department of Dermatology, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, No. 56 Nan Lishi Rd, Xicheng District, Beijing 100045, China. *E-mail: chouyabin@163.com
Citation: Acta Derm Venereol 2023; 103: adv5576. DOI: https://doi.org/10.2340/actadv.v103.5576.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Apr 19, 2023
Competing interests and funding: The authors have no conflicts of interest to declare.
A 5-year-old boy presented with a thin black band on one toenail, which had been noticed 7 days previously. He denied any history of preceding injury, but reported having had a haircut at home 10 days prior to presentation. Physical examination revealed a thin black band approximately 3 mm long on the second toenail of his left foot, visible both clinically and on dermoscopy (Fig. 1).
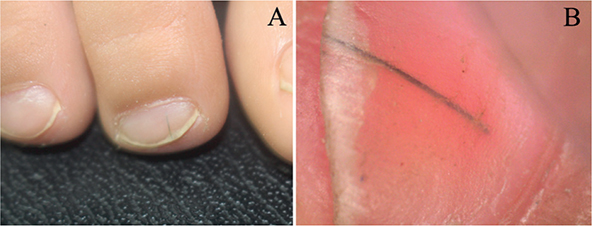
Fig. 1. (A) A thin black band approximately 3 mm long on the second toenail of the left foot. (B) A thin black band was observed under the toenail plate using dermoscopy.
What is your diagnosis? See next page for answer.
ANSWERS TO QUIZ
A Five-year-old Boy with a Thin Black Band on his Toenail: A Commentary
Diagnosis: Longitudinal melanonychia due to cutaneous pili migrans
A black hair was extracted from under the nail using sterile forceps after a manicure (Fig. 2A). Light microscopy revealed that it was a naked hair shaft without a follicle (Fig. 2B). After hair shaft removal, the longitudinal black band disappeared immediately. A diagnosis of longitudinal melanonychia due to cutaneous pili migrans was made. No recurrence was reported at 2-month follow-up.
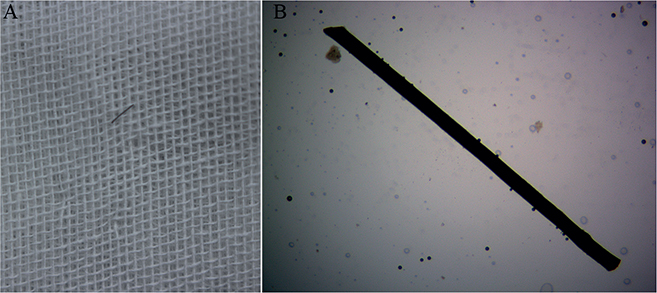
Fig. 2. (A) A black hair was extracted using sterile forceps. (B) The hair was found to be a naked hair shaft without a follicle under a light microscope (potassium hydroxide staining, original magnification ×400).
Longitudinal melanonychia is a relatively common nail finding that describes longitudinal pigmentation of the nail plate, which may be due to different colouring substances of exogenous and endogenous origin (1). Cutaneous pili migrans is a rare dermatosis characterized by a hair shaft or fragment embedded in the superficial skin following an injury or, occasionally, for unknown reasons (2). It usually affects frictional body sites, such as the ankle, sole, toe, breast, cheek, neck, jaw and abdomen (3). However, cutaneous pili migrans occurring in the nail, presenting as longitudinal melanonychia, has not been reported previously. To our knowledge, this is the first published case of longitudinal melanonychia due to cutaneous pili migrans.
The aetiology of longitudinal melanonychia varies according to the patient’s age at diagnosis. In paediatric cases, junctional naevus is the most frequent diagnosis, and melanoma is extremely rare (4). In contrast, melanoma is much more common in adults compared with in children (4). Because the pigment does not seem to reach the distal lunula, it is unlikely to be a junctional naevus. Dermoscopy demonstrated that the hair was located beneath the nail plate, which helped confirm the diagnosis.
The aetiology of cutaneous pili migrans is still unknown. It is considered to be an acquired condition due to a hair shaft embedded in the skin, which is a sharp material rubbing against a moving body part (3). Asian hair has the largest cross-sectional area and the highest tensile strength among all ethnic groups, which may explain why a larger number of cases are reported in East Asia (2). The abdomen is the most commonly involved body site of cutaneous pili migrans (5). The extracted hair shaft in this patient differed from his parents’ hair. Given his recent haircut, the condition may have been caused by barefoot walking at home afterwards.
The differential diagnosis in this patient should be for another aetiology of longitudinal melanonychia due to the unusual location. Cutaneous pili migrans is very easy to treat, and simple removal is sufficient to heal the lesion (5). In the current case, the hair shaft was easily removed after manicure due to its location.
In summary, we have reported the first case of cutaneous pili migrans presenting as longitudinal melanonychia. This can be considered a novel aetiology of longitudinal melanonychia. Dermoscopy can help to distinguish this condition from other causes of longitudinal melanonychia.
ACKNOWLEDGEMENTS
This work was supported by the Special Fund of the Pediatric Medical Coordinated Development Center of Beijing Municipal Administration No. XTZD20180502.
REFERENCES
- Haneke E, Baran R. Longitudinal melanonychia. Dermatol Surg 2001; 27: 580–584.
- Xie H, Zhang RZ, Zhu WY. A new site of cutaneous pili migrans in a 6-month-old infant. Indian J Dermatol Venereol Leprol 2012; 78: 498–499.
- Khare S, Sengar SS. Cutaneous pili migrans: a creeping eruption like condition easy to diagnose and cure. Med J Armed Forces India 2016; 72: 97–98.
- Tseng YT, Liang CW, Liau JY, Chang K, Tseng YH, Chen JS, et al. Longitudinal melanonychia: differences in etiology are associated with patient age at diagnosis. Dermatology 2017; 233: 446–455.
- Luo DQ, Liu JH, Huang YB, He DY, Zhang HY. Cutaneous pili migrans: a case report and review of the literature. Int J Dermatol 2009; 48: 947–950.