Psoriasis is a chronic, systemic inflammatory disease that affects the skin, with a high impact on patients’ quality of life. The aim of this study was to identify and determine the relative importance of unmet needs in the management of moderate-to-severe psoriasis in Spain, from a multi-stakeholder perspective. A mixed method-approach was used to collect information, design a questionnaire and a discrete-choice exercise, and elicit the unmet needs through a multidisciplinary committee composed of 12 experts. A total of 65 unmet needs were identified and categorized into 4 areas: clinical, patient-related, decision-making process, and social. Decision-making process unmet needs were perceived as the most pressing ones, followed by social, clinical and patient-related. Individually, the need to incorporate outcomes that are important to the patients and to have treatments that achieve total clearance with a rapid onset of action and long-term persistence were the most important unmet needs.
Key words: psoriasis; moderate-to-severe; biologics; unmet needs; discrete choice.
Accepted Mar 21, 2022: Epub ahead of print Mar 21, 2022
Acta Derm Venereol 2022; 102: adv00678.
DOI: 10.2340/actadv.v102.583
Corr: Néboa Zozaya, Department of Health Economics, Weber, Calle Moreto, 17, 5º Dcha., ES-28014, Madrid, Spain. E-mail: neboa.zozaya@weber.org.es
SIGNIFICANCE
Previous studies have mainly evaluated the unmet needs of psoriasis from the perspective of patients and clinicians. This study identified and determined the relative importance of unmet needs in the management of moderate-to-severe psoriasis in Spain, from a multi-stakeholder perspective. Sixty-five unmet needs were identified, highlighting a wide scope of areas for improvement. Regarding clinical unmet needs, treatments that focus on persistence, rapidity, and level of clearance should be favoured over treatments that aim at cost containment. A combined action is needed to better control the disease and its complications, improve patients’ quality of life, and counter stigma and ignorance.
INTRODUCTION
Psoriasis is a chronic, systemic immune-mediated disease that affects the skin and may be associated with other inflammatory conditions and comorbidities, such as psoriatic arthritis (1). It is a disabling disease with a significant negative impact on patients’ quality of life, affecting many areas of their life, including physical symptoms, emotions, daily activities, social life, and working sphere (2). Psoriasis is also associated with a substantial economic burden, borne by the healthcare system, the patients and their families, or by society (labour productivity losses) (3). The impact is higher for moderate-to-severe cases, which account for approximately one-third of patients with psoriasis in Spain (4).
Biologic therapy is a well-established strategy for managing moderate and severe psoriasis, which has evolved considerably during the last 2 decades. The first biologics approved for this indication by the European Medicines Agency (EMA) were tumour necrosis factor (TNF) inhibitors (infliximab, etanercept, and adalimumab). Since then, another TNF inhibitor (certolizumab pegol) and different interleukin (IL) inhibitors have been approved, targeting IL12/23 (ustekinumab), IL-17A (secukinumab, ixekizumab), IL-17 receptor (brodalumab), IL-17A/IL-17F (bimekizumab), and IL-23p19 (guselkumab, tildrakizumab, and risankizumab) (5). Firstly restricted to cases of failure, intolerance or contraindication of conventional systemics/ultraviolet (UV) therapy, the use of these drugs is rapidly increasing, and may account for approximately 20% of systemic treatments (6).
Despite the demonstrated clinical benefits of biologics over conventional systemic agents, patients with moderate-to-severe psoriasis still face unmet needs (7). First, there is still no cure for the disease (8). Between 40% and 60% of patients do not achieve complete or almost complete skin clearance after 1 year of treatment (6, 9). Regarding the onset of action, in 50% of patients who obtain total clearance with current treatments, it takes from 3 to 8 months after the start of treatment (10). At the very best, only 1 in 2 patients continue their treatment with biologics after 4 years, with most discontinuations due to lack of efficacy (11). Furthermore, results from clinical trials do not fully represent outcomes in clinical practice, given that patients may have different comorbidities and concomitant medication than subjects enrolled in such trials, originating higher rates of adverse events, combined with lower rates of reduction in Psoriasis Area and Severity Index (PASI) (12). Moreover, clinical trials are often not able to capture long-term persistence (13).
From a wider perspective, other unmet needs regarding the management of those patients can be highlighted, related to inadequate treatment or undertreatment (6, 14), patient dissatisfaction with adverse effects of biologicals (15), and many patients still reporting experiencing emotional distress and physical symptoms that affect their daily life (9, 16–18). Furthermore, itching and pruritus are often considered as the most troublesome and unpleasant symptoms of psoriasis, and there is a lack of effective antipruritic treatment for those patients (19). Moreover, other challenges remain, such as the need to (re)define treatment goals beyond skin manifestations (20), improve the route of administration, as well as aspects related to the wide variations in frequency and number of doses of administration, depending on the drug. In addition, the lack of homogeneity across different regions in terms of disease management and equal access to treatments (16), and the variability in list prices across treatments also represent further unmet needs (8, 21, 22). Finally, although alternative payment models that link payment to real outcomes have proved beneficial in allowing a more rapid introduction of innovative psoriasis treatments (23), the evidence regarding its implementation in Spain is very scarce.
Previous studies have evaluated the unmet needs of psoriasis from 2 different stakeholder perspectives: clinicians or patients (7, 15, 24–27). However, to our knowledge, no study to date has addressed the unmet needs in the management of moderate-to-severe psoriasis from a wide multi-stakeholder perspective. This approach may shed a more thorough light on those areas in need of improvement.
The aim of this study was to identify and determine the relative importance of unmet needs in the management of moderate-to-severe plaque psoriasis in Spain, from a multi-stakeholder view, in order to reach a more comprehensive understanding of the true challenges faced by patients, clinical professionals, and other decision-makers involved in the process.
MATERIALS AND METHODS
A mixed-method approach, including a literature review and 2 online meetings with stakeholders (1 with a multidisciplinary expert committee (MEC) and the other with a patient focus group) held via a teleconferencing platform (Zoom, Zoom Video Communications, Inc., San Jose, CA, USA) were used to collect information, to design a questionnaire and a discrete-choice exercise, and to elicit unmet needs regarding moderate-to-severe psoriasis in Spain.
Identification of unmet needs in the management of moderate-to-severe psoriasis
An initial scoping literature review was conducted to identify and summarize previously published unmet needs in psoriasis, using PubMed, Medline, and grey literature as sources of information. This information was included in a pre-read document, which was sent by email to each member of the MEC and the patient focus group.
The MEC comprised 12 experts with different perspectives in the assessment of unmet needs in moderate-to-severe psoriasis, including 3 dermatologists, 1 nurse with expertise in patients with psoriasis, 1 psychologist with expertise in patients with psoriasis, 1 hospital pharmacist, 1 hospital manager, 1 regional healthcare manager, 1 politician with expertise in public health, 1 health economist, and 2 patient representatives (1 of whom also participated in the patient focus group). Experts were chosen according to their professional profile and experience in the management and decision-making of moderate-to-severe psoriasis in Spain, aiming to achieve a balanced geographical representation (6 autonomous regions). The MEC attended a virtual meeting (Zoom, Zoom Video Communications, Inc.) in which they discussed and identified current unmet needs regarding the management of moderate-to-severe psoriasis in Spain from a multi-stakeholder approach. In addition, the MEC was asked to complete and validate a comprehensive list of potential unmet needs, which were included in a questionnaire to determine the relative importance of each unmet need in the opinion of each expert.
The participants in the patient focus group (n=6) were invited by Acción Psoriasis, Spain’s largest psoriasis patient association, and were recruited according to the following inclusion criteria: adult patients diagnosed with moderate or severe psoriasis, belonging to different locations across Spain, currently receiving biological treatment. The patients discussed how the disease affected the different spheres of their life since their diagnosis and shared their opinions on the most pressing unmet needs regarding the general management of the disease in Spain and the biologic treatments currently available in the country. This information was used to complement the unmet needs identified by the MEC.
Quantification of the relative importance of unmet needs in the management of moderate-to-severe psoriasis
Based on the information obtained at both meetings, an electronically formatted questionnaire (Surveymonkey Inc., San Mateo, CA, USA, www.surveymonkey.com) was designed to elicit the relative importance of each identified unmet need, on a scale ranging from 0 (no unmet need, i.e. no room for improvement) to 10 (largely unmet need, i.e. much room for improvement), which also included a “don’t know/no answer” option. The questionnaire was responded online by the members of the MEC (1 round of answers).
A descriptive analysis was performed to compute means, medians and standard deviations (SD) of the responses, both in general terms and by type of respondent: dermatologists, other healthcare professionals (including the psychologist, the hospital pharmacist, and the nurse), decision-makers (including the hospital manager, the regional healthcare manager, the politician, and the health economist), and patients. Kruskal–Wallis equality of populations rank tests were used to explore median’s heterogeneity across subgroups of experts, for each of the 65 identified unmet needs. p-values < 0.05 were considered significant. The statistical analyses were carried out through software Stata 14.0 (StataCorp LLC, College Station, TX, USA).
Identification of unmet needs regarding biological treatments for moderate-to-severe psoriasis
In addition, an online-administered pairwise discrete choice exercise was developed (PAPRIKA method (28), a method for multi-criteria decision making or conjoint analysis), using the software 1000minds (1000Minds Ltd, Dunedin, New Zealand) (29), to be answered by both professional experts (excluding patient representatives, n = 10) and patients (including the patients in the focus group and the patients in the MEC, n = 7), so that both perspectives could be compared.
The exercise was designed to elicit the attributes of treatments, which, in the opinion of the respondents, are currently in most need of improvement in Spain, from the following 5: degree of clearance; onset of action; persistence of clearance; rapidity-persistence of clearance; and annual treatment cost per patient, each 1 presented in 2 levels (high and low). Each question consisted on choosing the currently most needed treatment in Spain, amongst 2 hypothetical treatments defined by 2 attributes at a time and involving a trade-off, so that implicit preferences could be extracted. The sequence in which the 32 pairs of options were presented to each respondent was random in order to avoid systematic bias from the question sequence. If the respondent considered both hypothetical treatments to be equally needed, an “equally needed” answer was available.
RESULTS
Unmet needs in the management of moderate-to-severe psoriasis
Together, the members of the MEC and the patient focus group identified a total of 65 potential unmet needs regarding management of moderate-to-severe psoriasis. All unmet needs identified by the MEC were validated in the patient focus group. The patient focus group identified 3 unmet needs: route of administration of treatment, site where the treatment is dispensed (currently, in Spain, biologic treatments and apremilast are dispensed by hospital pharmacies), and frequency of administration. All patients agreed that both intravenous and subcutaneous treatments are inconvenient in terms of route of administration (compared with oral administration routes). There was also vast agreement on the need to decrease the frequency of administration and to dispense treatments closer to the patient’s residence (e.g. community pharmacies or courier delivery).
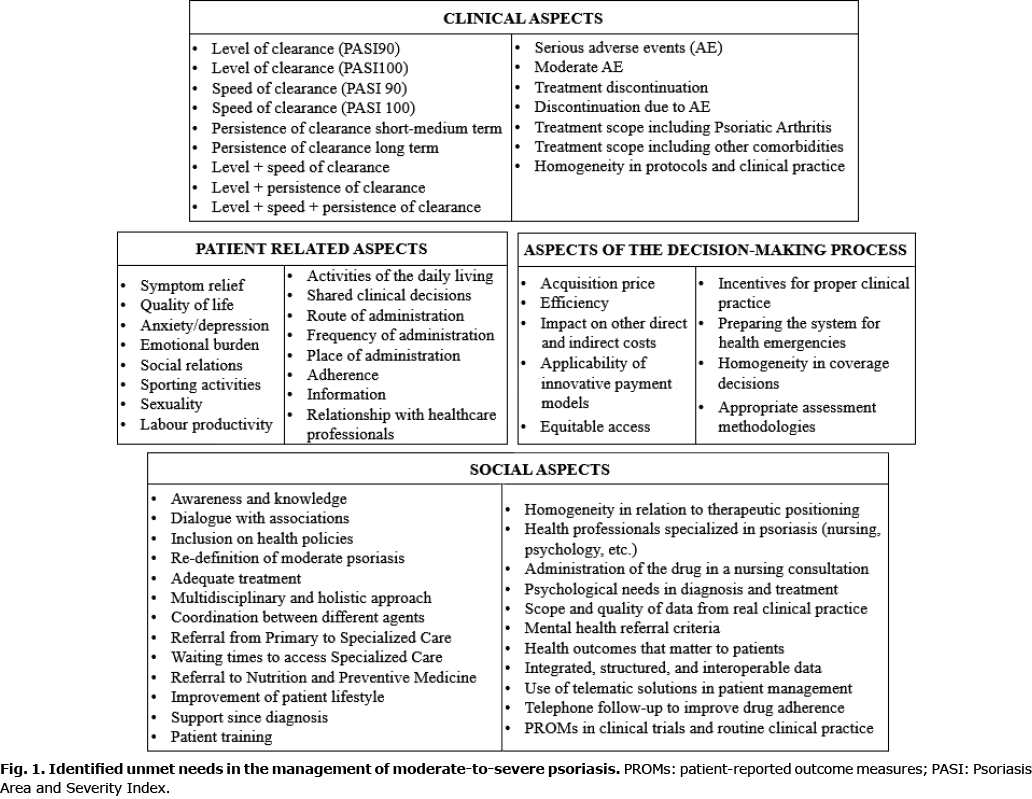
The 65 identified unmet needs were categorized into 4 areas: clinical, patient-related, decision-making process, and social, which included the following aspects, amongst others: (i) clinical: efficacy (level of clearance, rapidity and persistence), safety/tolerability and the management of comorbidities; (ii) patient-related: impact of the disease (physical, emotional, social, activities of daily living), convenience, adherence, information, communication and joint decision-making; (iii) decision-making: resource management (price/efficiency), impact of biologicals on other system costs, financing models, equitable access, incentives to clinical practice, readiness and flexibility of the system regarding the management of moderate-to-severe psoriasis in the face of health emergencies (e.g. COVID-19), adequacy of evaluation methods; (iv) social: awareness, coordination, multidisciplinary approach, waiting times, referral criteria, use of patient-reported outcome measures (PROMs), etc. (Fig. 1).
Relative importance of unmet needs in the management of moderate-to-severe psoriasis
As a whole, unmet needs identified in the “decision-making process” category received the highest score (mean 7.1 (median 7.0), compared with 7.0 for social unmet needs (median 7.3), 6.5 for clinical unmet needs (median 7.0), and 6.0 for patient-related unmet needs (median 6.5), and was therefore perceived as the most pressing in the opinion of the members of the MEC.
Individually, the need to incorporate health outcomes that are important to the patients into clinical and general disease management decisions within the social category received the highest average score (mean 8.3; median 8.0; SD 1.0), closely followed by the need to have treatments that achieve a total clearance with high rapidity and long-term persistence within the clinical category (mean 8.2; median 8.0; SD 1.5).
Within the clinical category, the second most important unmet need was to achieve total clearance in combination with long-term persistence of clearance (mean 7.7; median 8.0; SD 1.8), followed by the need to have treatments that include an adequate management of psoriatic arthritis as a comorbidity (mean 7.5; median 8.0; SD 1.8). Scores by type of respondent are shown in Table I. Statistically different medians were found between dermatologists and decision-makers for the unmet need related to the frequency of serious adverse events, and between decision-makers and patients for the proportion of patients discontinuing treatment due to moderate or mild adverse events.

Within the patient-related category, the most relevant unmet needs were to improve anxiety and/or depression (mean 7.2; median 8.0; SD 2.7), and to improve the overall emotional burden (mean 7.2; median 7.5; SD 2.6). Dermatologists scored highest the need to enhance the patient’s relationship with the different healthcare professionals; decision-makers gave the highest scores to improving the patient’s quality of life; and patients gave the greatest importance to improving emotional aspects and symptom relief, improving the route of administration of treatments, and participating in joint decision-making with their doctor (Table II). Significant differences in medians between all subgroups were found for relief of symptoms and improvement in the ability to perform sporting activities.

The decision-making process category showed the greatest heterogeneity of opinions. On average, the categories with the highest scores were the need to incorporate health outcomes that matter to the patient into the decisions and the need to use adequate referral criteria from primary to specialized healthcare. Dermatologists scored highest the need to create incentives for proper clinical practice and evaluation methodology; other healthcare professionals (including the psychologist, the nurse, and the hospital pharmacists) considered that the greatest challenges lie in the purchase price of available drugs and in achieving equity of access. Decision-makers (the managers, the health economist, and the politician) considered the need to improve the applicability of innovative contracting models as their highest priority. The 2 most important unmet needs in this category in the patients’ opinion were improving equity in access and preparing the system for future health emergencies. Healthcare professionals, decision-makers and patients showed statistically significant differences in the unmet need related to appropriate cost and efficiency evaluation methods (Table III).

Finally, within the social category, the need to incorporate health outcomes that matter to the patient into the assessment of the social value of treatments was given the highest score (mean 8.3; median 8.0; SD 1.0). This view was shared by the dermatologists and the decision-makers. Other healthcare professionals rated highest the need for improvement in a multidisciplinary and holistic approach to the management of psoriasis. Patients gave highest priority to improving referral criteria, improving waiting times to access specialized care, and increasing the importance attributed to the patients’ psychological needs at the time of diagnosis and treatment (Table IV).
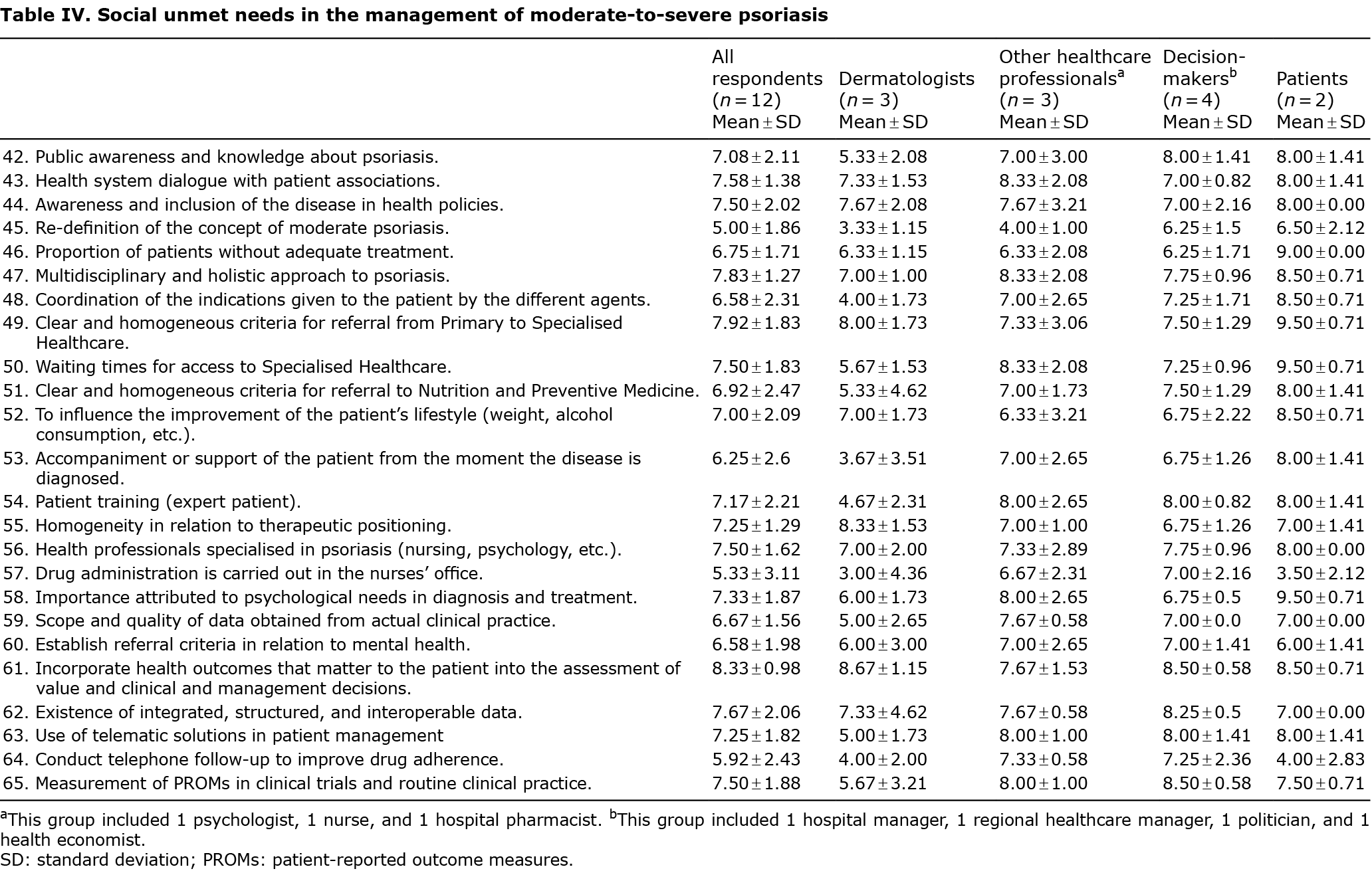
Fig. 2 provides a graphic comparison of the mean scores of unmet needs within each of the 4 categories, by type of respondent.

Unmet needs regarding current biological treatments for moderate-to-severe psoriasis
The results obtained from the pairwise choice exercise showed that, according to respondents, the combination of treatment persistence and rapidity of onset of action were the first (for patients) or second (for healthcare professionals and decision-makers) clinical attribute with the greatest need for improvement. Persistence or durability of clearance and level of clearance were also relevant in terms of unmet needs. The attribute with the least need for improvement was the cost of biologics for both patients and professionals (Fig. 3).

DISCUSSION
This study has identified 65 unmet needs in the management of moderate-to-severe psoriasis, revealing that the decision-making and social areas are the most pressing ones, whilst individually, the key unmet needs refer to incorporating relevant patient-reported outcomes (PROs), and to have treatments that combine clearance, rapidity and persistence.
To our knowledge, this is the first study to consider the perspective of the different stakeholders involved in the management of moderate-to-severe psoriasis within the Spanish healthcare system. It has also introduced a new approach to assess treatment effectiveness in moderate-to-severe psoriasis, carrying out a combined analysis of persistence, rapidity, and degree of clearance.
Unmet needs associated with the management of moderate-to-severe psoriasis in Spain are still numerous and reveal the importance of addressing not only clinical effectiveness, but also patient-related unmet needs, aspects related to the decision-making process, and social factors.
Overall, patients gave higher scores to all unmet needs, with the exception of persistence of clearance. Patients had significantly different perceptions to those of dermatologists as to the urgency of addressing patient needs, such as symptom relief, increased quality of life, improvement in sex life, information provided to relatives and caregivers, and the convenience of treatment route and frequency of administration. These differences in perception shed light on the need to improve communication and joint decision-making between patients and their physicians. The need to increase the involvement of the patient in decision-making has been previously suggested as an unmet need (24). Some of the most pressing social unmet needs were incorporating health outcomes that are important to the patients into clinical decisions and measuring PROMs in clinical trials and real-world practice, in line with the preferences reported by dermatologists in the USA, Canada, and Europe (7, 30, 31). In this sense, it is worth mentioning that the principles of chronomedicine are being used in order to improve outcomes that are relevant to patients, through the restructuring of drug administration timings, amongst other strategies (32, 33).
In Spain, the national healthcare system provides universal free coverage to all patients. As such, the cost of therapies plays no role among patient preferences or their consumption of healthcare resources. Hence, it is not surprising that patients rated costs as the attribute with the least need for improvement. However, cost is an element that is taken into account to decide hospital purchases and therefore may define access to treatments. It is therefore interesting that cost was also the least important unmet need in the view of decision-makers and healthcare professionals, when compared with clinical unmet needs, such as persistence, rapidity, and level of clearance. Therefore, stakeholders place more value on the latter clinical attributes than on cost containment.
Unmet needs related to current therapies for psoriasis have been studied in other countries (7, 14, 15, 34). One of the most notable examples gathered information on physician perspectives in North America and Europe regarding the impact of psoriasis, psoriatic arthritis, and their treatment on patients’ daily lives (7). Physicians acknowledged unmet treatment needs largely concerning long-term safety/tolerability and efficacy of currently available therapies. In addition, results suggested undertreatment of psoriasis among dermatologists. Contrary to Van de Kerkhof’s findings, the results of the current study did not include concerns over long-term safety of current treatments among clinicians or concerns regarding undertreatment of psoriasis.
In a recent study, Carretero et al. (35) analysed the social aspects that would benefit the management of psoriasis within the Spanish healthcare system, including a holistic approach. They estimated that, for every euro invested, a social benefit of 5.04 euros would be obtained.
Discrete choice experiments have been previously carried out to elicit psoriasis treatment preferences (25, 26, 30), but never to better understand unmet needs. The results obtained from the discrete choice exercise are quite consistent with those related to clinical unmet needs obtained from the questionnaire. Level of clearance, persistence alone, and persistence combined with rapidity of action were perceived as the most urgent unmet needs and should therefore be the main areas of focus. Rapidity of clearance and the need to contain the costs of biologics were perceived as the least urgent unmet needs by healthcare professionals and decision-makers when performing the pairwise exercise. Even if these were also the least urgent unmet needs from the patients’ perspective, they perceived rapidity of clearance as a much more pressing matter than did professionals, while they perceived costs as a less pressing matter.
Furthermore, some developments have been made with regards to the use of precision medicine and nanotechnology in order to optimize current available treatments. Conic et al. (36) have observed that a sustained response to therapy was associated with a decrease in distribution widths of red cells and that this marker in conjunction with the measurement of mean platelet volume may be a cost-effective manner to identify patients with psoriasis and psoriatic arthritis at risk of developing major adverse cardiac events. On the other hand, Damiani et al. (37) provided several examples of how nanodermatology-based solutions, built on specific dysregulated biomarkers, can assist and enhance different steps of the process of healthcare delivery (from diagnosis to therapeutics).
Different actions could be carried out to counter the impact of some of the identified unmet needs. These include efforts by governments and policy-makers to increase access to comprehensive and individually adapted medical treatment, in a patient-centred and integrated health services model. Health professionals also play a key role, through the proper management of psoriasis, its symptoms and comorbidities, as well as creating a multidisciplinary environment, seeking for consensus on classification and standardization topics, as well as to progressively developing guidelines adapted to real practice. Patients’ organizations are also an important piece in this context, as they should continue to advocate the rights of individuals, support people with the disease, and encourage awareness campaigns and training activities.
The current study is not exempt from certain limitations. First, the small sample size impedes generalization of the results to all stakeholders involved in the management of psoriasis, as well as carrying out a robust subgroup analysis by type of respondent. Moreover, the perception of unmet needs may vary, not only by type of stakeholder, but also with their socio-demographic characteristics, geographical origin, and working status, as previous studies have found (25, 38). Secondly, this study focused on the Spanish context, which may differ from that of other European countries. Furthermore, the results might not be generalizable to all patients with psoriasis, and specifically, to the non-Spanish ones. Thirdly, as the focus of this study was on moderate-to-severe psoriasis, which is managed in a specialized care setting in Spain, the results did not take into account the perception of primary care experts.
In conclusion, the unmet needs associated with management of moderate-to-severe psoriasis in Spain are still numerous, and they include a large social and patient-related component. PROMs data should be collected in trials involving moderate-to-severe psoriasis and inform therapeutic decisions. Improvement of patient–physician communication regarding the decision-making process in treatment selection is crucial to ensure that patient preferences and physician perceptions are in concordance. With regards to clinical unmet needs, treatments that focus on persistence, rapidity, and level of clearance should be favoured over treatments that aim at cost containment. This understanding is fundamental to help make informed decisions aimed at improving efficiency and equity in the allocation of public resources for the management of this chronic disease.
As outlined in the WHO global strategy, optimum treatment of psoriasis, and its comorbidities, require shifting to a model of people-centred and integrated health services (2). A combined action by governments, policy-makers, scientists, health professionals, patients’ organizations, civil society and the media is required to control the disease and its complications, improve patients’ quality of life, and fight stigma and ignorance.
Continued research is needed to develop efficient treatments for psoriasis with convenient administration routes as well as regimens that will address issues of low treatment satisfaction among patients. There is also a need to carry out further multi-stakeholder research on unmet needs with a larger representative sample of clinicians, decision-makers, and patients.
ACKNOWLEDGEMENTS
The authors thank the patients from Acción Psoriasis who participated in the focus group: Bárbara Ojeda Esquerdo, Elena Cortés Soler, Fátima Rodríguez Moreda, Jaume Aixala Oriola and Mireia Pérez Ortiz. Apart from those patients, the other 2 patients who participated in the focus group have authorship in the current study, as they participated in both the MEC and focus group.
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request
This project was funded by UCB Pharma S.A. Their participation was limited to sponsoring the project. They had no involvement in the online meetings held with the experts committee, nor in the writing of the manuscript or in the data analysis.
The authors have no conflicts of interest to declare.
REFERENCES
- Menter A, Strober BE, Kaplan DH, Kivelevitch D, Prater EF, Stoff B, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J Am Acad Dermatol 2019; 80: 1029–1072.
- World Health Organization. Global report on psoriasis. WHO (Internet) 2016 (cited 2021 May 31). Available from: https://apps.who.int/iris/handle/10665/204417.
- Burgos-Pol R, Martínez-Sesmero JM, Ventura-Cerdá JM, Elías I, Caloto MT, Casado MÁ. The cost of psoriasis and psoriatic arthritis in 5 European countries: a systematic review. Actas Dermosifiliogr (Engl Ed) 2016; 107: 577–590.
- Carrascosa J, Pujol R, Daudén E, Hernanz-Hermosa J, Bordas X, Smandia J, et al. A prospective evaluation of the cost of psoriasis in Spain (EPIDERMA project: Phase II). J Eur Acad Dermatol Venereol 2006; 20: 840–845.
- Reid C, Griffiths CEM. Psoriasis and treatment: past, present and future aspects. Acta Derm Venereol 2020; 100: adv00032.
- Association of Psoriasis Patients, Psoriatic Arthritis Patients and their Relatives. Survey “NEXT” on current needs and future expectations in psoriasis in Spain: report of results. Acción Psoriasis 2020. [cited 2021 Apr 29] Available from: https://www.accionpsoriasis.org/recursos/publicaciones/otras-publicaciones.html.
- Kerkhof PCM, Reich K, Kavanaugh A, Bachelez H, Barker J, Girolomoni G, et al. Physician perspectives in the management of psoriasis and psoriatic arthritis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis survey. J Eur Acad Dermatol Venereol 2015; 29: 2002–2010.
- Sbidian E, Chaimani A, Garcia-Doval I, Doney L, Dressler C, Hua C, et al. Systemic pharmacological treatments for chronic plaque psoriasis: a network meta-analysis. Cochrane Database Syst Rev 2021.[cited 2021 Apr 20] Available from: https: //www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011535.pub4/full.
- Armstrong AW, Soliman AM, Betts KA, Wang Y, Gao Y, Puig L, et al. Comparative efficacy and relative ranking of biologics and oral therapies for moderate-to-severe plaque psoriasis: a network meta-analysis. Dermatol Ther (Heidelb) 2021; 11: 885–905.
- Egeberg A, Andersen YMF, Halling-Overgaard A-S, Alignahi F, Thyssen JP, Burge R, et al. Systematic review on rapidity of onset of action for interleukin-17 and interleukin-23 inhibitors for psoriasis. J Eur Acad Dermatol Venereol 2020; 34: 39–46.
- Lin P-T, Wang S-H, Chi C-C. Drug survival of biologics in treating psoriasis: a meta-analysis of real-world evidence. Sci Rep 2018; 8: 16068.
- Mason KJ, Barker JNWN, Smith CH, Hampton PJ, Lunt M, McElhone K, et al. Comparison of drug discontinuation, effectiveness, and safety between clinical trial eligible and ineligible patients in BADBIR. JAMA Dermatol 2018; 154: 581–588.
- Puig L, Carrascosa J-M, Daudén E, Sulleiro S, Guisado C. Drug survival of conventional systemic and biologic therapies for moderate-to-severe psoriasis in clinical practice in Spain: prospective results from the SAHARA study. J Dermatolog Treat 2020; 31: 344–351.
- Lebwohl MG, Bachelez H, Barker J, Girolomoni G, Kavanaugh A, Langley RG, et al. Patient perspectives in the management of psoriasis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis Survey. J Am Acad Dermatol 2014; 70: 871–881.
- Christophers E, Griffiths CEM, Gaitanis G, van de Kerkhof P. The unmet treatment need for moderate to severe psoriasis: results of a survey and chart review. J Eur Acad Dermatol Venereol 2006; 20: 921–925.
- Association of Psoriasis Patients, Psoriatic Arthritis Patients and their Relatives. IMPAS Survey Summary - Impact of Psoriasis and Associated Comorbidities. Acción Psoriasis (Internet) 2016. [cited 2021 May 5] Available from: https: //issuu.com/accionpsoriasis/docs/anexo_encuesta_impas_-_d__a_mundial.
- González-Parra S, Daudén E. Psoriasis and depression: the role of inflammation. Actas Dermosifiliogr 2019; 110: 12–19.
- Association of Psoriasis Patients, Psoriatic Arthritis Patients and their Relatives. Psoriasis “NEXT” survey: report of results. Acción Psoriasis 201. [cited 2021 May 5] Available from: https: //issuu.com/accionpsoriasis/docs/next.
- Jaworecka K, Muda-Urban J, Rzepko M, Reich A. Molecular aspects of pruritus pathogenesis in Psoriasis. Int J Mol Sci 2021; 22: 858.
- Boehncke W-H, Brembilla NC. Unmet needs in the field of psoriasis: pathogenesis and treatment. Clin Rev Allergy Immunol 2018; 55: 295–311.
- General Council of Pharmaceutical Associations. Drug Database – Laboratory Selling Price (PVL). BotPlus 2020. [cited 2021 Apr 25] Available from: https://botplusweb.portalfarma.com/.
- Epstein D, Espín J. Evaluation of new medicines in Spain and comparison with other European countries. Gac Sanit 2020; 34: 133–140.
- Norlin JM, Althin R, Schmitt-Egenolf M, Persson U. An outcome-based payment model for biologic agents in psoriasis: a report from the Swedish Institute for Health Economics. IHE (Internet) 2018. [Cited 2021 Mar 3] Available from: https://ihe.se/wp-content/uploads/2018/07/IHE-Report-2018_2_.pdf.
- Feldman, S, Goffe, B, Rice, G, Mitchell, M. The challenge of managing psoriasis: unmet medical needs and stakeholder perspectives. Am Health Drug Benefits 2016. [cited 2017 May 29] Available from: http://www.ahdbonline.com/components/com_mams/dl.php?dlid=1615.
- Kromer C, Schaarschmidt M-L, Schmieder A, Herr R, Goerdt S, Peitsch WK. Patient preferences for treatment of psoriasis with biologicals: a discrete choice experiment. PLoS ONE 2015; 10: e0129120.
- Ashcroft DM, Seston E, Griffiths CEM. Trade-offs between the benefits and risks of drug treatment for psoriasis: a discrete choice experiment with U.K. dermatologists. Br J Dermatol 2006; 155: 1236–1241.
- Puig, L, Dobao P de la C, Linares M, Suárez J, Pastor MV, Vidal A, et al. Psoriasis expert report: opinion of Spanish dermatologists on the management of moderate-to-severe psoriasis with biologic agents in adult patients. Actas Dermosifiliogr 2013; 104: 400–408.
- 1000 Minds. PAPRIKA method. 1000minds 2021. [cited 2021 Jul 14] Available from: https: //www.1000minds.com/about/paprika.
- 1000minds. Decision-making and conjoint analysis software. 1000minds 2019. [cited 2019 Dec 19] Available from: https://www.1000minds.com/.
- Feldman SR, Regnier SA, Chirilov A, Hey F, Gilloteau I, Cella D. Patient-reported outcomes are important elements of psoriasis treatment decision making: a discrete choice experiment survey of dermatologists in the United States. J Am Acad Dermatol 2019; 80: 1650–1657.
- Tan J, Stacey D, Fung K, Barankin B, Bissonnette R, Gulliver W, et al. Treatment decision needs of psoriasis patients: cross-sectional survey. J Cutan Med Surg 2010; 14: 233–239.
- Damiani G, Bragazzi NL, Garbarino S, Chattu VK, Shapiro CM, Pacifico A, et al. Psoriatic and psoriatic arthritis patients with and without jet-lag: does it matter for disease severity scores? Insights and implications from a pilot, prospective study. Chronobiol Int 2019; 36: 1733–1740.
- Damiani G, Watad A, Bridgewood C, Pigatto PDM, Pacifico A, Malagoli P, et al. The impact of ramadan fasting on the reduction of PASI score, in moderate-to-severe psoriatic patients: a real-life multicenter study. Nutrients 2019; 11: 277.
- Kragballe K, van de Kerkhof PC, Gordon KB. Unmet needs in the treatment of psoriasis. Eur J Dermatol 2014; 24: 523–532.
- Carretero G, Moreno D, González Domínguez A, Trigos D, Ledesma A, Sarquella E, et al. Multidisciplinary approach to psoriasis in the Spanish National Health System: a social return on investment study. Glob Reg Health Technol Assess 2020; 7: 50–56.
- Conic RR, Damiani G, Schrom KP, Ramser AE, Zheng C, Xu R, et al. Psoriasis and psoriatic arthritis cardiovascular disease endotypes identified by red blood cell distribution width and mean platelet volume. J Clin Med 2020; 9: 186.
- Damiani G, Pacifico A, Linder DM, Pigatto PDM, Conic R, Grada A, et al. Nanodermatology-based solutions for psoriasis: state-of-the art and future prospects. Dermatol Ther 2019; 32: e13113.
- Bolt T, Kobayashi H, Mahlich J. Patient and physician preferences for therapy characteristics for psoriasis: a discrete choice experiment in Japan. Pharmacoecon Open 2019; 3: 255–264.