Darier disease and Hailey-Hailey disease are severe, monogenetic dermatological disorders with mutations affecting all cells, making them liable to exhibit extra- dermal symptoms. The aim of this study is to assess broad cognitive function in individuals with these diseases, using an experimental, case-control set-up comparing cognition in patients with that in healthy controls matched for age, sex and level of education. Cognition was assessed with the Cambridge Neuropsychological Test Automated Battery. Patients with Darier disease (n = 29) performed significantly poorer on 5 of the 10 key cognitive measurements, while patients with Hailey-Hailey disease (n = 25) did not perform differently from controls. The main conclusion is that patients with Darier disease exhibit significant impairment in cognitive function, which reinforces the view that Darier disease should be regarded as a disorder affecting multiple organs, and should therefore be given medical consideration, and possibly treatment, as such.
Key words: Darier disease; Hailey-Hailey disease; cognition; cognitive impairment; SERCA2; SPCA1.
Accepted Apr 29, 2021; Epub ahead of print Apr 30, 2021
Acta Derm Venereol 2021; 101: adv00476.
doi: 10.2340/00015555-3818
Corr: Jakob D. Wikström, Dermato-Venereology Clinic, Karolinska University Hospital, Eugeniavägen 3, SE-171 64 Stockholm, Sweden. E-mail: jakob.wikstrom@ki.se
SIGNIFICANCE
Darier disease and Hailey-Hailey disease are both severe skin diseases. Cognition in these diseases has been evaluated and compared with that of matched healthy individuals. Significant impairment in cognitive function was found in patients with Darier disease compared with controls, while no significant difference from controls was found in Hailey-Hailey disease. This adds to the growing body of evidence supporting the view that Darier disease is a disorder not just affecting the skin, and that patients might require special medical consideration and possibly targeted medication.
INTRODUCTION
Darier disease (DD) and Hailey-Hailey disease (HHD) are rare, hereditary and severe dermatological diseases with similar pathophysiology, and a similar estimated prevalence of approximately 1:50,000 individuals (1–4). DD and HHD are mapped to different chromosomal locations. DD presents with lifelong and widespread greasy hyperkeratotic papules in seborrhoeic regions, nail abnormalities, mucous membrane changes and malodorous plaques (1, 5) and HHD is characterized by blistering and painful erosive and erythematous plaques in the flexures and sites of friction (4, 6, 7). Both diseases are caused by heterozygote autosomal dominant mutations; for DD in the ATP2A2 gene, and for HHD in the ATP2C1 gene.
The ATP2A2 gene encodes a sarco/endoplasmic reticulum Ca2+-ATPase 2 (SERCA2), which transports calcium from the cytosol into the endoplasmic reticulum lumen. The protein encoded by the ATP2C1 gene is human secretory pathway Ca2+/Mn2+-APTase 1 (SPCA1), a calcium and manganese pump in the Golgi apparatus (8–12). SERCA2 and SPCA1 are ubiquitously expressed and of key importance for endoplasmic reticulum and Golgi function, sometimes referred to as “housekeeping” proteins (13–18). To date, there is a lack of feasible, targeted treatments for either disease.
Cognitive impairment is a hallmark feature of many psychiatric and neurodegenerative diseases, making it an important area of research within these fields. A recent review by Britzolaki et al. (19) summarizes the involvement of SERCA2 in neurobiology in general and its association with specific neuropsychiatric diseases and neurodegenerative disorders, supporting its role as an important factor in these areas. However, only loose implications can be drawn as to the contribution of SERCA2 in cognitive function per se. For SPCA1, there is evidence of its expression and activity in several types of neuronal cells (20), reports linking it to the fundamental neurobiological processes of neural differentiation (21) and neural tube closure (22), as well as data implicating its role in neurodegenerative disorders (23).
Only a few case reports of affective symptoms in patients with HHD have been reported (24–26), and there are no studies connecting HHD or SPCA1 with cognitive function or other psychiatric symptoms. Conversely, more evidence exists of an association between DD and several psychiatric diseases and intellectual impairments (1, 27–36), as well as an effect on overall cognition (37–39). However, these studies estimate statistical associations or are population-based in nature, and general cognition has not been tested experimentally at the individual patient level with a closely matched control group in either disease group. Cognitive function in itself is at the centre of not only several psychiatric and neurological disorders, but also has a pivotal influence on everyday life in general. Thus, the results of correct and relevant evaluation of cognition can yield information of great importance for both the patients themselves and the physicians treating them.
The aim of this study was to assess broad cognitive function in groups of patients with DD and with HHD and closely matched healthy control subjects. To the best of our knowledge, this is the first report experimentally investigating and comparing cognitive function in either disease group with a closely matched control group, having been previously examined mainly through register data and questionnaire surveys.
MATERIALS AND METHODS
Recruitment of participants
Patients were recruited through the dermatology department at Karolinska University Hospital (Stockholm, Sweden), as well as through family members of known patients. Healthy controls were recruited through advertisements in the dermatology clinic and through advertisements on the Karolinska Institutet (Stockholm, Sweden) website. Controls received symbolic monetary compensation for their time (200 SEK).
Study group
The study included 29 patients with DD, 25 patients with HHD, and matched healthy controls in a 1:1 ratio. Controls were matched for age, sex and level of education. Age was matched in ± 5-year intervals. Level of education was graded in 6 categories according to the highest level of education achieved and matched in ± 1-level intervals: (i) disrupted education before high school; (ii) disrupted high school; (iii) high school education; (iv) university education 3 years; (v) university education master’s degree; and (vi) PhD
Inclusion criteria were: typical skin lesions in combination with typical histopathology and/or family history. Exclusion criteria were: age < 18 years, significant ongoing psychiatric disorders, neurotropic or psychotropic medication, active substance abuse, dementia, acute illness during the past 4 weeks, and pregnancy.
Clinical assessment
Patients underwent careful history-taking and physical skin examination. Family history of either DD or HHD was defined as the presence of a first- or second-degree relative with the disease verified at a dermatology clinic. Weight and height were also measured.
Cognitive assessment
Cognitive assessment was performed with the Cambridge Neuropsychological Test Automated Battery (CANTAB Cognitive assessment software, Cambridge Cognition Ltd, Cambridge, UK) (40), consisting of a set of tests run on an iPad computer tablet; a valid and widespread software in the assessment of cognition (41, 42), CANTAB minimizes potential biases, such as cultural context, through the use of visually abstract components and non-verbal responses (40). It has been shown to have a test/re-test reliability of 0.75–0.80, which is considered as well within the acceptable range (43). The tests lasted approximately 30 min and were performed under standardized, undisturbed conditions in quiet rooms.
The test battery, called Core Cognition, consists of 5 sequential tests with a total of 10 key measurements: (i) motor screening test (MOT) (1 key measurement), (ii) paired associates learning (PAL), measuring episodic memory (2 key measurements), (iii) reaction time (RTI) (2 key measurements), (iv) spatial working memory (SWM), measuring assumptions, planning and strategy (2 key measurements), and (v) rapid visual information processing (RVP) (3 key measurements).
The tests evaluate sustained attention, processing speed, episodic memory and working memory, yielding a broad assessment of general cognition (44). In summary, the tests consist of abstract symbols, shapes and numbers appearing on the iPad screen, to be selected accurately under time- and precision-based circumstances.
Statistical analyses
Descriptive statistics was used to summarize study subject demographics with means and standard deviations (SD). Patients with DD and with HHD were compared with their respective matched healthy controls using Student’s unpaired t-test with 2-tailed p-values. p-values < 0.05 were considered statistically significant. A Benjamini-Hochberg approach was used for the correction for multiple comparisons, performed within each set of tests. Statistics were carried out in GraphPad Prism (GraphPad Software Inc., San Diego, CA, USA) and Excel (Microsoft).
Ethics approval
The study protocol was reviewed and approved by the regional Institutional Review Board, (approval #2019-01298).
RESULTS
Study group characteristics
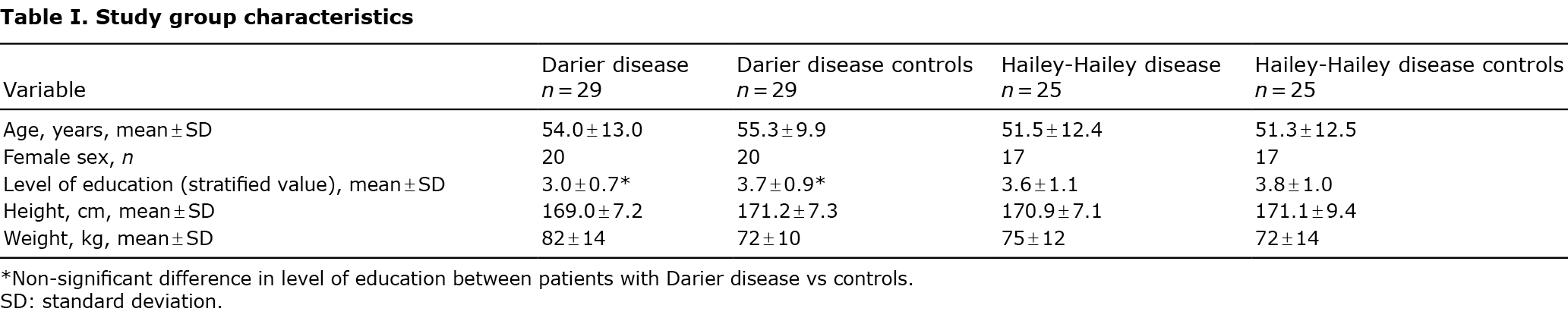
Successful matching was performed for age, sex and level of education as described in the Methods section. Most control subjects were matched with patients from both disease groups, in a ratio of 1:1. Study group characteristics are shown in Table I.
Cognitive assessment
The outcome of the cognitive assessment for all 10 key measurements of the 5 tests are summarized in Table II and the individual tests and the areas of cognitive function they assess are described in more detail in Table III. The DD vs controls group showed a statistically significant impairment in 5 out of 10 individual key measurements, namely both measurements for Reaction time and all 3 measurements for Rapid visual information processing. In the HHD vs controls group, no statistically significant differences were found.


DISCUSSION
This study is the first to experimentally assess cognition in patients with DD and with HHD compared with matched healthy controls and, consequently, the impact of SERCA2 and SPCA1 on cognitive function in humans. There was a statistically significant impairment in cognitive function in patients with DD, but not in patients with HHD. Interestingly, all 5 impaired individual results in the DD patient group were found to be in the Reaction time (RTI) and Rapid visual information processing (RVP) tests, while the Motor screening (MOT), Paired associates learning (PAL) and Spatial working memory (SWM) tests were statistically non-significant for all 5 remaining measurements within these 3 sets of tests. However, regarding the actual values for these 5 non-significant measurements, patients with DD performed poorer than controls on every measurement.
Cognitive impairment
Primarily in early literature, dating back to the late 1950s, there are reports of patients with DD being referred to as “mentally retarded” or “mentally subnormal”; descriptions that in essence refer to a cognitive disability (37, 45). These reports included no experimental assessment of cognition or control groups, have limited scientific value, and the nomenclature would be deemed unethical today. Although impaired cognition may be considered a sensitive subject, we believe it is an important topic to study, since patients with DD may be in need of systemic medication that targets the brain, and other affected organs, in addition to the skin.
The data from the current study are consistent with a previous Swedish nationwide, register-based study, with diagnoses defined according to International Classification of Diseases (ICD) codes that found patients with DD (n = 770) to have a 6-fold increase in the risk of being diagnosed with intellectual disability (38). Perhaps most interesting, in congruence with the current results, is conscription data from a subset of male patients with DD (n = 114) in the study without a diagnosis of intellectual disability showing a highly significantly reduced mean score on an IQ test in comparison with matched comparison subjects (n = 885) randomly selected from the Swedish Total Population Register (38).
The authors identified only one previous study that conducted an experimental assessment of cognition on patients with DD (n = 19) (39). Researchers found significant differences mainly on reading and reading-related measures, something that carries the potential for biases deriving from factors such as cultural interpretation and level of education. The study is also limited by the fact that the control group consisted of “skilled learners”, that no close matching was done between patients and controls, and that the statistics did not include any correction for multiple comparisons for the large number of p-values (n = 20) (39). Close matching is particularly important for rare, chronic diseases, such as DD. Meanwhile, studies establishing a link between DD and psychiatric symptoms/disorders have mostly been estimating statistical associations, being descriptive and non-experimental, utilizing psychiatric questionnaires and register data (1, 27–36). Nevertheless, all these data are in line with our results of a significant cognitive impairment in patients with DD.
To our knowledge, there are no reports in the published literature linking HHD with cognitive impairment or disability, and, for the realm of psychiatric disorders, only a few case reports establishing an association with affective symptoms (24–26). The results of the current study support that subjects with HHD have normal cognition, which is also the authors’ clinical experience. This suggests that there are cellular mechanisms that are able to correct for SPCA1 dysfunction, but not for SERCA2 dysfunction, leading to the significant negative impact on cognitive function shown here.
Systemic disease
Both SERCA2 and SPCA1 are ubiquitously expressed “housekeeping” proteins, where the disease phenotypes of DD and HHD, respectively, are caused by haploinsufficiency, meaning that 1 allele is incapable of producing adequate protein levels for normal function (8, 13–18, 46). There is, therefore, reason to suspect and investigate whether either disease might be associated with other symptoms and diseases apart from the skin. In medical literature, HHD has not been found to be associated with extradermal symptoms, while, as previously noted, there is strong evidence for a direct link between DD and psychiatric and intellectual disabilities. Our group has recently published reports shedding further light on DD as a multi-organ disease, showing associations with type 1 diabetes and pancreatic beta-cell dysfunction, as well as heart failure (47–49).
There is ample evidence suggesting the direct importance of SERCA2 in the pathophysiology of psychiatric and neurodegenerative disorders. Both experimental and large associative studies have identified SERCA2 and ATP2A2 as important actors in schizophrenia and bipolar disorder (50–52), as well as in Parkinson’s disease (53, 54) and Alzheimer’s disease (55–57). These and other studies illustrate the importance of SERCA2 in brain physiology and brain-related disease (19, 58). Importantly, patients with DD and with HHD provide the unique possibility of direct evaluation of SERCA2 and SPCA1 in human subjects, something not previously done for the assessment of cognitive function in a tightly matched fashion. As shown here, the cognitive impairment seen in patients with DD, by extension, adds to the growing body of evidence for the role of SERCA2 in brain physiology and function.
Clinical implications
The clinical implications of a cognitive impairment in patients with DD are potentially wide-reaching. The DD patient group displayed statistically significantly impaired performance on all measurements within the RTI and RVP tests. Reaction time and information processing speed has both been linked to increased all-cause mortality (59, 60). In addition, slower processing speed has been found to be a possible risk factor for the development of mental distress (61), and reaction time has been correlated strongly with general mental ability (62).
Cognitive function is at the centre of myriad aspects of everyday life, such as school, work, carrying out social interactions and performing all types of executive functions in life. Knowledge of an impairment in cognition for patients with DD could motivate early evaluation, diagnosis and treatment of potential related disabilities. Appraising the possible need for supporting measures in school could be imperative for the individual, as well as possible adjustments and considerations in the workplace. There might be a need for targeted, systemic drugs that can work to alleviate not only dermal symptoms in DD, but also the symptoms from other organs, not least the brain. A limiting factor in the study was the relatively small number of individuals in each patient group; a natural consequence given the rarity of the diseases. Also, a higher ratio of matched cases:controls could have improved the statistical outcome.
In the authors’ own experiences, the results of this study raise important questions as to how patients with DD should be clinically appraised from a cognitive perspective. To date, there may be limited value to implementing cognitive testing as a standard in clinical practice, since no treatment is available. Nevertheless, testing could be meaningful for the individual, not least in childhood in order to better support special educational needs. It is likely that these patients do not currently receive proper support. Further study is needed, in which children of patients with DD who test mutation-positive undergo cognitive testing to determine whether the impairment described in this paper is also present in early childhood. In addition, for adult patients who might benefit from diagnosis of an impairment in cognitive function; for example, for social services support, the CANTAB Core Cognition test battery is a possible tool. However, this kind of assessment should mainly be performed by specialists, such as psychologists and neuropsychiatrists. Finally, genetic counselling is strongly recommended, primarily for patients who are planning to conceive, with referral to clinical geneticists, so that they can be informed about procedures such as preimplantation genetic diagnosis.
Conclusion
A statistically significant impairment in several measurements of cognitive function was observed in patients with DD, but not in patients with HHD, compared with closely matched healthy controls. These results demonstrate the importance of SERCA2 in the brain, and further indicate that DD should be treated as a multi-organ disorder and not just a dermatological disease, and hence may require special consideration.
ACKNOWLEDGEMENTS
We thank the participating patients, volunteers and Research Nurse Helena Griehsel. We are also grateful to the following funding agencies (Vetenskapsrådet, Hudfonden, Svenska Sällskapet för medicinsk forskning, ALF medicin Stockholm, Jeanssons stiftelse, Tore Nilssons Stiftelse) for their support.
The authors have no conflicts of interest to declare.
REFERENCES
- Burge SM, Wilkinson JD. Darier-White disease: a review of the clinical features in 163 patients. J Am Acad Dermatol 1992; 27: 40–50.
- Munro CS. The phenotype of Darier’s disease: penetrance and expressivity in adults and children. Br J Dermatol 1992; 127: 126–130.
- Cooper SM, Burge SM. Darier’s disease: epidemiology, pathophysiology, and management. Am J Clin Dermatol 2003; 4: 97–105.
- Engin B, Kutlubay Z, Celik U, Serdaroglu S, Tuzun Y. Hailey-Hailey disease: a fold (intertriginous) dermatosis. Clin Dermatol 2015; 33: 452–455.
- Engin B, Kutlubay Z, Erkan E, Tüzün Y. Darier disease: a fold (intertriginous) dermatosis. Clin Dermatol 2015; 33: 448–451.
- Burge SM. Hailey-Hailey disease: the clinical features, response to treatment and prognosis. Br J Dermatol 1992; 126: 275–282.
- Ben Lagha I, Ashack K, Khachemoune A. Hailey-Hailey disease: an update review with a focus on treatment data. Am J Clin Dermatol 2019.
- Sakuntabhai A, Ruiz-Perez V, Carter S, Jacobsen N, Burge S, Monk S, et al. Mutations in ATP2A2, encoding a Ca2+ pump, cause Darier disease. Nat Genet 1999; 21: 271–277.
- Nellen RG, Steijlen PM, van Steensel MA, Vreeburg M, Frank J, van Geel M, et al. Mendelian disorders of cornification caused by defects in intracellular calcium pumps: mutation update and database for variants in ATP2A2 and ATP2C1 associated with Darier disease and Hailey-Hailey disease. Hum Mutat 2017; 38: 343–356.
- Sudbrak R, Brown J, Dobson-Stone C, Carter S, Ramser J, White J, et al. Hailey-Hailey disease is caused by mutations in ATP2C1 encoding a novel Ca(2+) pump. Hum Mol Genet 2000; 9: 1131–1140.
- Hu Z, Bonifas JM, Beech J, Bench G, Shigihara T, Ogawa H, et al. Mutations in ATP2C1, encoding a calcium pump, cause Hailey-Hailey disease. Nat Genet 2000; 24: 61–65.
- Miyauchi Y, Daiho T, Yamasaki K, Takahashi H, Ishida-Yamamoto A, Danko S, et al. Comprehensive analysis of expression and function of 51 sarco(endo)plasmic reticulum Ca2+-ATPase mutants associated with Darier disease. J Biol Chem 2006; 281: 22882–22895.
- Deng H, Xiao H. The role of the ATP2C1 gene in Hailey-Hailey disease. Cell Mol Life Sci 2017; 74: 3687–3696.
- Pizzo P, Lissandron V, Capitanio P, Pozzan T. Ca(2+) signalling in the Golgi apparatus. Cell Calcium 2011; 50: 184–192.
- Vandecaetsbeek I, Trekels M, De Maeyer M, Ceulemans H, Lescrinier E, Raeymaekers L, et al. Structural basis for the high Ca2+ affinity of the ubiquitous SERCA2b Ca2+ pump. Proc Natl Acad Sci U S A 2009; 106: 18533–18538.
- Vandecaetsbeek I, Vangheluwe P, Raeymaekers L, Wuytack F, Vanoevelen J. The Ca2+ pumps of the endoplasmic reticulum and Golgi apparatus. Cold Spring Harb Perspect Biol 2011; 3: a004184.
- Gunteski-Hamblin AM, Clarke DM, Shull GE. Molecular cloning and tissue distribution of alternatively spliced mRNAs encoding possible mammalian homologues of the yeast secretory pathway calcium pump. Biochemistry 1992; 31: 7600–7608.
- Vangheluwe P, Raeymaekers L, Dode L, Wuytack F. Modulating sarco(endo)plasmic reticulum Ca2+ ATPase 2 (SERCA2) activity: cell biological implications. Cell Calcium 2005; 38: 291–302.
- Britzolaki A, Saurine J, Klocke B, Pitychoutis PM. A role for SERCA pumps in the neurobiology of neuropsychiatric and neurodegenerative disorders. Adv Exp Med Biol 2020; 1131: 131–161.
- Murín R, Verleysdonk S, Raeymaekers L, Kaplán P, Lehotský J. Distribution of secretory pathway Ca2+ ATPase (SPCA1) in neuronal and glial cell cultures. Cell Mol Neurobiol 2006; 26: 1355–1365.
- Sepúlveda MR, Vanoevelen J, Raeymaekers L, Mata AM, Wuytack F. Silencing the SPCA1 (secretory pathway Ca2+-ATPase isoform 1) impairs Ca2+ homeostasis in the Golgi and disturbs neural polarity. J Neurosci 2009; 29: 12174–12182.
- Brown JM, García-García MJ. Secretory pathway calcium ATPase 1 (SPCA1) controls mouse neural tube closure by regulating cytoskeletal dynamics. Development 2018; 145.
- Li L, Hu GK. Pink1 protects cortical neurons from thapsigargin-induced oxidative stress and neuronal apoptosis. Biosci Rep 2015; 35.
- Yokota K, Sawamura D. Hailey-Hailey disease with affective disorder: report of a case with novel ATP2C1 gene mutation. J Dermatol Sci 2006; 43: 150–151.
- Körner J, Rietschel M, Nöthen MM, Wilk CM, Bauer R, Propping P, et al. Familial cosegregation of affective disorder and Hailey-Hailey disease. Br J Psychiatry 1993; 163: 109–110.
- Wilk M, Rietschel M, Körner J, Möller HJ, Nöthen MM, Bauer R, et al. [Pemphigus chronicus benignus familiaris (Hailey-Hailey disease) and bipolar affective disease in 3 members of a family]. Hautarzt 1994; 45: 313–317.
- Cederlof M, Bergen SE, Langstrom N, Larsson H, Boman M, Craddock N, et al. The association between Darier disease, bipolar disorder, and schizophrenia revisited: a population-based family study. Bipolar Disord 2015; 17: 340–344.
- Dodiuk-Gad RP, Cohen-Barak E, Khayat M, Milo H, Amariglio-Diskin L, Danial-Faran N, et al. Darier disease in Israel: combined evaluation of genetic and neuropsychiatric aspects. Br J Dermatol 2016; 174: 562–568.
- Gordon-Smith K, Jones LA, Burge SM, Munro CS, Tavadia S, Craddock N. The neuropsychiatric phenotype in Darier disease. Br J Dermatol 2010; 163: 515–522.
- Gordon-Smith K, Green E, Grozeva D, Tavadia S, Craddock N, Jones L. Genotype-phenotype correlations in Darier disease: a focus on the neuropsychiatric phenotype. Am J Med Genet B Neuropsychiatr Genet 2018; 177: 717–726.
- Ringpfeil F, Raus A, DiGiovanna JJ, Korge B, Harth W, Mazzanti C, et al. Darier disease – novel mutations in ATP2A2 and genotype-phenotype correlation. Exp Dermatol 2001; 10: 19–27.
- Denicoff KD, Lehman ZA, Rubinow DR, Schmidt PJ, Peck GL. Suicidal ideation in Darier’s disease. J Am Acad Dermatol 1990; 22: 196–198.
- Jacobsen NJ, Lyons I, Hoogendoorn B, Burge S, Kwok PY, O’Donovan MC, et al. ATP2A2 mutations in Darier’s disease and their relationship to neuropsychiatric phenotypes. Hum Mol Genet 1999; 8: 1631–1636.
- Craddock N, Owen M, Burge S, Kurian B, Thomas P, McGuffin P. Familial cosegregation of major affective disorder and Darier’s disease (keratosis follicularis). Br J Psychiatry 1994; 164: 355–358.
- Cheour M, Zribi H, Abdelhak S, Drira S, Ben Osman A. Les manifestations neuropsychiatriques de la maladie de Darier: résultat préliminaire d’une étude epidémioclinique et génétique de huit familles. [Darier’s disease: an evaluation of its neuropsychiatric component]. Encephale 2009; 35: 32–35.
- Jones I, Jacobsen N, Green EK, Elvidge GP, Owen MJ, Craddock N. Evidence for familial cosegregation of major affective disorder and genetic markers flanking the gene for Darier’s disease. Mol Psychiatry 2002; 7: 424–427.
- Burge S. Darier’s disease – the clinical features and pathogenesis. Clin Exp Dermatol 1994; 19: 193–205.
- Cederlof M, Karlsson R, Larsson H, Almqvist C, Magnusson PK, Nordlind K, et al. Intellectual disability and cognitive ability in Darier disease: Swedish nation-wide study. Br J Dermatol 2015; 173: 155–158.
- Dodiuk-Gad R, Lerner M, Breznitz Z, Cohen-Barak E, Ziv M, Shani-Adir A, et al. Learning disabilities in Darier’s disease patients. J Eur Acad Dermatol Venereol 2014; 28: 314–319.
- CANTAB®. p. [Cognitive assessment software]. Cambridge, UK: Cambridge Cognition; 2020.
- Robbins TW, James M, Owen AM, Sahakian BJ, McInnes L, Rabbitt P. Cambridge Neuropsychological Test Automated Battery (CANTAB): a factor analytic study of a large sample of normal elderly volunteers. Dementia 1994; 5: 266–281.
- Haring L, Mõttus R, Koch K, Trei M, Maron E. Factorial validity, measurement equivalence and cognitive performance of the Cambridge Neuropsychological Test Automated Battery (CANTAB) between patients with first-episode psychosis and healthy volunteers. Psychol Med 2015; 45: 1919–1929.
- Lowe C, Rabbitt P. Test/re-test reliability of the CANTAB and ISPOCD neuropsychological batteries: theoretical and practical issues. Cambridge Neuropsychological Test Automated Battery. International Study of Post-Operative Cognitive Dysfunction. Neuropsychologia 1998; 36: 915–923.
- CANTAB®. p. Core Cognition. [accessed 2020 Sept]. Available from: https://www.cambridgecognition.com/cantab/test-batteries/core-cognition/.
- Svendsen IB, Albrectsen B. The prevalence of dyskeratosis follicularis (Darier’s disease) in Denmark: an investigation of the heredity in 22 families. Acta Derm Venereol 1959; 39: 256–269.
- Fairclough RJ, Lonie L, Van Baelen K, Haftek M, Munro CS, Burge SM, et al. Hailey-Hailey disease: identification of novel mutations in ATP2C1 and effect of missense mutation A528P on protein expression levels. J Invest Dermatol 2004; 123: 67–71.
- Ahanian T, Curman P, Leong IUS, Brismar K, Bachar-Wikstrom E, Cederlof M, et al. Metabolic phenotype in Darier disease: a cross-sectional clinical study. Diabetol Metab Syndr 2020; 12: 12.
- Bachar-Wikstrom E, Curman P, Ahanian T, Leong IUS, Larsson H, Cederlof M, et al. Darier disease is associated with heart failure: a cross-sectional case-control and population based study. Sci Rep 2020; 10: 6886.
- Cederlöf M, Curman P, Ahanian T, Leong IUS, Brismar K, Bachar-Wikstrom E, et al. Darier disease is associated with type 1 diabetes: findings from a population-based cohort study. J Am Acad Dermatol 2019; 81: 1425–1426.
- Consortium SWGotPG. Biological insights from 108 schizophrenia-associated genetic loci. Nature 2014; 511: 421–427.
- Richard EA, Khlestova E, Nanu R, Lisman JE. Potential synergistic action of 19 schizophrenia risk genes in the thalamus. Schizophr Res 2017; 180: 64–69.
- Hough C, Lu SJ, Davis CL, Chuang DM, Post RM. Elevated basal and thapsigargin-stimulated intracellular calcium of platelets and lymphocytes from bipolar affective disorder patients measured by a fluorometric microassay. Biol Psychiatry 1999; 46: 247–255.
- Betzer C, Lassen LB, Olsen A, Kofoed RH, Reimer L, Gregersen E, et al. Alpha-synuclein aggregates activate calcium pump SERCA leading to calcium dysregulation. EMBO Rep 2018; 19: e44617.
- Goodwin J, Nath S, Engelborghs Y, Pountney DL. Raised calcium and oxidative stress cooperatively promote alpha-synuclein aggregate formation. Neurochem Int 2013; 62: 703–711.
- Dreses-Werringloer U, Lambert JC, Vingtdeux V, Zhao H, Vais H, Siebert A, et al. A polymorphism in CALHM1 influences Ca2+ homeostasis, Abeta levels, and Alzheimer’s disease risk. Cell 2008; 133: 1149–1161.
- Brunello L, Zampese E, Florean C, Pozzan T, Pizzo P, Fasolato C. Presenilin-2 dampens intracellular Ca2+ stores by increasing Ca2+ leakage and reducing Ca2+ uptake. J Cell Mol Med 2009; 13: 3358–3369.
- Nensa FM, Neumann MH, Schrötter A, Przyborski A, Mastalski T, Susdalzew S, et al. Amyloid beta a4 precursor protein-binding family B member 1 (FE65) interactomics revealed synaptic vesicle glycoprotein 2A (SV2A) and sarcoplasmic/endoplasmic reticulum calcium ATPase 2 (SERCA2) as new binding proteins in the human brain. Mol Cell Proteomics 2014; 13: 475–488.
- Britzolaki A, Saurine J, Flaherty E, Thelen C, Pitychoutis PM. The SERCA2: A Gatekeeper of Neuronal Calcium Homeostasis in the Brain. Cell Mol Neurobiol 2018; 38: 981–994.
- Der G, Deary IJ. Reaction times match IQ for major causes of mortality: evidence from a population based prospective cohort study. Intelligence 2018; 69: 134–145.
- Iwasa H, Kai I, Yoshida Y, Suzuki T, Kim H, Yoshida H. Information processing speed and 8-year mortality among community-dwelling elderly Japanese. J Epidemiol 2014; 24: 52–59.
- Gale CR, Harris A, Deary IJ. Reaction time and onset of psychological distress: the UK Health and Lifestyle Survey. J Epidemiol Community Health 2016; 70: 813–817.
- Der G, Deary IJ. The relationship between intelligence and reaction time varies with age: Results from three representative narrow-age age cohorts at 30, 50 and 69 years. Intelligence 2017; 64: 89–97.