Chronic ulcers cause a significant burden to patients and society. This study evaluated long-term mortality among patients with chronic ulcers diagnosed at a dermatology clinic between 1980 and 2010. The mortality risk and causes of death of 3,489 patients with ulcers were compared with a matched reference group of 10,399 individuals, and factors associated with increased mortality risk were examined. Long-term mortality was increased in patients with chronic ulcers (hazard ratio (HR) 1.74) and in both males and females (HR 1.99 and 1.62, respectively). Diabetes was the most relevant underlying cause of death (HR 8.98), and of the immediate causes of death, sepsis was strongly associated with mortality (HR 5.86). The mortality risk was highest among those with arterial ulcers (HR 2.85), but also increased in patients with atypical, mixed and venous leg ulcers. In conclusion, patients with chronic ulcers are at an increased mortality risk irrespective of age, sex and ulcer aetiology.
Key words: skin ulcer; leg ulcer; peripheral arterial disease; sepsis; diabetes mellitus.
Accepted Apr 14, 2021; Epub ahead of print Apr 15, 2021
Acta Derm Venereol 2021; 101: adv00455.
doi: 10.2340/00015555-3803
Corr: Teija Kimpimäki, Department of Dermatology, Tampere University Hospital, Central Hospital, PO Box 2000, FIN-33521 Tampere, Finland. E-mail: teija.kimpimaki@tuni.fi
SIGNIFICANCE
Chronic ulcers cause a significant burden to patients and society. In this study, long-term mortality and causes of death among 3,489 patients with chronic ulcers were compared with 10,399 matched individuals. Long-term mortality was increased in patients with chronic ulcers, in both sexes and all age groups. Diabetes was the most relevant underlying cause of death. The mortality risk was highest among those with arterial ulcers, but also increased in patients with atypical, mixed and venous leg ulcers. In conclusion, patients with chronic ulcers have increased mortality risk irrespective of age, sex and ulcer aetiology.
INTRODUCTION
Chronic ulcers are ulcers expressing impaired healing capability due to various internal or external factors. However, the exact definition and categorization of chronic ulcers in both clinical practice and research varies, especially as there is a lack of consensus regarding the duration of chronicity (1, 2). Nevertheless, chronic ulcers are known to cause a significant burden to society: the prevalence of chronic ulcers in industrialised countries has been reported to be up to 1% (3–5), and they cause remarkable healthcare costs (6), comparable to that of managing obesity (7). Moreover, as the population ages (8), the prevalence and incidence of chronic ulcers will increase (9, 10), escalating the costs of wound care even further (11).
The majority of chronic ulcers are of vascular aetiology: venous insufficiency constitutes approximately 50–70% of all chronic lower leg ulcers (12–14), and peripheral arterial disease and mixed arterial-venous disease cause 11–15% and 13–18% of chronic ulcers, respectively (12, 13). However, up to 20% of chronic ulcers have an atypical ulcer aetiology, such as vasculitis, pyoderma gangraenosum, rheumatoid arthritis, infection or malignancy (15–17).
In addition to the aetiological disease causing the chronic ulcer, the majority of patients with ulcers have one or several comorbidities that may further impair the wound-healing process (13, 14). Arterial hypertension is the most common comorbidity reported, but obesity and diabetes mellitus are also common among patients with chronic ulcers (13, 14). Moreover, patients with chronic ulcers are at risk of numerous complications, such as pain, various infections, amputation and even death (16–19).
Current evidence on mortality among patients with chronic ulcers mostly concerns patients with a diabetic foot ulcer, in which the mortality risk is even greater than 2-fold compared with non-diabetic patients (20). Considerably less is known about mortality among patients with other chronic wounds, and the evidence is somewhat conflicting, with varying study populations, study methods and follow-up times. There is some evidence suggesting that mortality is also increased in patients with arterial, pressure and malignant ulcers (19, 21–23), but the mortality among patients with venous leg ulcers has been reported to be both increased, and at the same level as in controls (19, 24). Moreover, scarce evidence exists about the causes of death among patients with chronic ulcers and whether they differ from those of non-ulcer controls.
The aim of the current study was to evaluate long-term mortality among patients with chronic ulcers, focusing especially on patients with vascular and atypical ulcers. A further aim was to evaluate the causes of death among patients with chronic ulcers and to analyse the factors associated with the increased mortality risk.
MATERIALS AND METHODS
Patients and their reference group
The study cohort consisted of patients with chronic ulcers diagnosed and treated as inpatients or outpatients at the Department of Dermatology, Tampere University Hospital, between 1980 and 2010. The patients with ulcers treated at the Department of Dermatology have hard-to-heal vascular, i.e. venous, arterial or mixed (arterial and venous aetiology), ulcers or atypical ulcers needing tertiary care. The treatment of atypical ulcers is centralized at the Department of Dermatology, but vascular ulcers are treated at both the Department of Dermatology and the Department of Vascular Surgery. Patients with peripheral arterial disease without ulcers are not treated at the Department of Dermatology. Also, diabetic foot and pressure ulcers were typically treated elsewhere at the time of the study.
Chronic ulcer patients aged 18 years or over at the time of the first ulcer diagnosis, i.e. the index day, were included in the study. The patient data were selected from Tampere University Hospital’s patient record system using International Classification of Diseases versions 8, 9 and 10 (ICD8-10), with the diagnostic codes 454.00, 454.99, 4540A, 4549X and I83.0 for venous ulcers and 440.20, 444.40, 4402A, 4408X, 4409X, 4442A and I70.2 for arterial ulcers. For mixed ulcers, both of the above-mentioned ICD8-10 codes for arterial and venous ulcers were required. For patients with pyoderma gangraenosum ulcers, ICD10 diagnostic code L88 was used. Finally, patients having unspecified or unclassified chronic ulcers were selected using ICD8-10 codes 707.08, 707.09, 7071A, 7078X, 7079X, L97 and L98.4, and for patients with vasculitic ulcers, a previously selected series of patients with skin-limited vasculitis manifesting as ulcers from the same study period and hospital was used (25). As a reference group, 3 subjects, matched for sex, age and place of residence on the index day, were selected for each patient with ulcers. Individuals for the reference group were selected from the Finnish Digital and Population Data Services Agency.
Methods
The medical records of patients with ulcers with an unspecified ulcer diagnosis (see above) were evaluated retrospectively in order to obtain a more specific ulcer diagnosis. From all patients with ulcers, in addition to the ulcer diagnosis, demographic data on the index day and the number of ulcer episodes treated at the Department of Dermatology, Tampere University Hospital, were recorded. Ulcer episodes were considered separate if the time period between the visits was 2 years or more. The date and cause of death and/or the date of emigration were obtained, using the personal identification codes of the patients with ulcers and their reference group from the Statistics Finland agency, which maintains the registry of causes of death covering virtually all deceased residents of Finland. The underlying and immediate causes of death were coded according to ICD8-10. In the registry, underlying causes of death are further classified into 54 groups (26), and all categories were analysed for cause-specific mortality. From the immediate causes of death, sepsis and pneumonia were selected for further analysis, as, according to the authors’ clinical experience and previous research, these are common among patients with ulcers (21, 24, 27). For mortality analysis, the follow-up time started from the date of the first entry into treatment due to a chronic ulcer and ended at the date of death, emigration from Finland or the data collection date (31 December 2017).
The mortality risk and causes of death of patients with chronic ulcers were compared with those of their reference group, and the demographic factors associated with mortality were assessed. In addition, the mortality risks of patients with arterial, venous, mixed and atypical ulcers were investigated separately, and in these analyses only patients having ulcers of one aetiology (one or more episodes) were included, i.e. patients having treatment episodes due to different ulcer aetiologies during the follow-up were excluded from the analysis. Finally, the effect of the number of ulcer episodes on mortality was examined, and, in this analysis, the patients with ulcers were divided into 3 groups: those having 1, 2 or 3 or more ulcer episodes.
Statistical analysis
The data were analysed using SPSS Statistics 25.0 (IBM Corp, Armonk, NY, USA) and Stata 16.0 (StataCorp LLC, College Station, TX, USA). Descriptive statistics of demographic variables were computed to characterize the patients with ulcers and their reference group. The Kaplan–Meier method was used to estimate survival curves for patients with ulcers and their reference group. Cox proportional hazards regression models were used to estimate the hazard ratios (HR) and 95% confidence intervals (95% CI) of all-cause mortality, as well as the mortality associated with ulcer aetiology, when comparing the patients with ulcers with their reference group. In addition, Cox’s proportional hazards regression models were used when assessing different causes of death, and Fine & Gray’s proportional subhazards model was used to assess mortality for the competing causes of death.
RESULTS
The study cohort comprised 3,489 adult patients with chronic ulcers and a matched reference group of 10,399 individuals. Three matches were not found for 34 of the patients with ulcers. The median age of the patients with ulcers at the index day was 71 (range 18–99) years, and 65% of the patients were female. At the time of first ulcer diagnosis, males were 8 years younger than females (median age 66 vs 74 years, p < 0.001). The most common aetiology of the first ulcer was venous insufficiency, followed by peripheral arterial disease. Of the 303 patients having an atypical ulcer as the first ulcer episode, 165 (54%) had vasculitis, 74 (24%) pyoderma gangraenosum, 47 (16%) a rheumatoid ulcer, 14 (5%) a malignant ulcer and 3 (1%) calciphylaxis. Among those with other ulcer aetiologies, 313 (44%) had an unspecified ulcer, 258 (36%) a post-traumatic ulcer, 68 (9%) a diabetic foot ulcer and the remainder had ulcer aetiologies which comprised less than 5% of the other ulcers (Table I).

During the follow-up time, 80% of the patients with ulcers had died, compared with 64% of the reference group. The median survival times for the patients with ulcers and the reference group were 7 and 13 years, respectively. The mortality risk of the patients with ulcers was higher than that of their reference group (Fig. 1, p < 0.001), and the HR for mortality among all patients with ulcers compared with the reference group was 1.74 (1.66–1.82) (Table II). When patients were divided into the age groups of < 50, 50–59, 60–69, 70–79 and ≥ 80 years, the mortality risk of the patients with ulcers was significantly higher in all age groups compared with their reference group (p < 0.001 in all analysis). When patients with ulcers were divided into 2 groups: one group aged 50 years or younger at the time of the first ulcer and another group who were older, the HR for mortality was higher among younger patients compared with their own reference group (4.04, 3.28–4.97 vs 1.75, 1.68–1.84). For male patients with chronic ulcers, the HR for mortality was higher compared with their reference group (1.99, 1.84–2.15) than that of the female patients with ulcers (1.62, 1.53–1.71). Among the most common underlying causes of death, the mortality risk of the patients with ulcers was highest for diabetes (HR 8.98; subdistribution hazard ratios (SHR) 7.01) compared with their reference group, but it was also increased for digestive diseases, pneumonia, ischaemic heart diseases, cerebrovascular diseases and malignancies (Table II). Sepsis was the immediate cause of death for 82 (3%) patients with ulcers and 54 (1%) individuals in the reference group, and it was strongly associated with mortality among patients with ulcers (HR 5.86, 4.15–8.27; SHR 4.56, 3.23–6.43). Pneumonia was also associated with an increased risk of mortality among patients with ulcers (HR 1.75, 1.56–1.96; SHR 1.27, 1.14–1.43), and it was the immediate cause of death for 425 (12%) patients with ulcers and 1,010 (10%) individuals in the reference group.


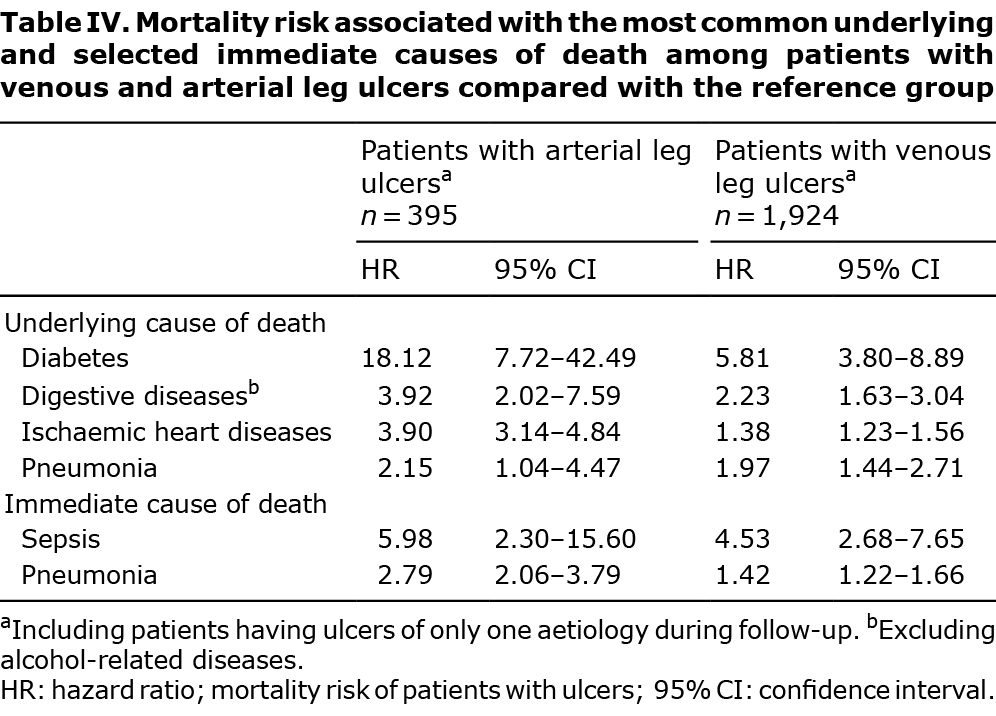
When the mortality of the patients with ulcers according to ulcer aetiology was analysed, the survival time was 3 years for an arterial leg ulcer, 4 years for a mixed leg ulcer, 8 years for an atypical ulcer and 9 years for a venous leg ulcer (p < 0.001). Correspondingly, the HR for mortality was highest among patients with an arterial leg ulcer (HR 2.85), but it was significantly increased in all groups (Table III). When the causes of death were analysed according to ulcer aetiology, patients with mixed leg ulcers had an increased mortality risk for ischaemic heart diseases (HR 3.27, 1.04–5.09), but, other than that, statistically significant results were not detected among patients with mixed leg ulcers or atypical ulcers. Instead, significantly increased mortality risks were detected among patients with arterial and venous leg ulcers (Table IV). Of the underlying causes of death, the highest mortality risk was associated with diabetes: the HR for patients with arterial leg ulcers was 18.12, and for patients with venous leg ulcers, it was 5.81. As an immediate cause of death, the HR for sepsis was higher than that for pneumonia in both groups.

During the follow-up time, patients with ulcers had up to 6 ulcer episodes: 2,913 (84%) had one, 423 (12%) 2 and 129 (4%) 3 or more ulcer episodes. Compared with the patients with ulcers with only 1 ulcer episode, patients having 2 or at least 3 ulcer episodes had lower HRs for mortality (0.63, 0.56–0.71 and 0.49, 0.40–0.60; respectively). When age was analysed in these groups, patients with ulcers who had only one ulcer episode during the follow-up time were older on the index day compared with the patients with ulcers with 2 or at least 3 ulcer episodes (p < 0.001).
DISCUSSION
The current study established that patients with ulcers have a significantly increased long-term mortality risk compared with their age-, sex- and place of residence-matched reference group. The mortality was increased in all age groups and also in both sexes, but, intriguingly, the HR for mortality was higher among male than female patients with ulcers and also among those receiving their first diagnosis of ulcer at the age of 50 years or younger. Furthermore, the mortality risk was shown to be increased irrespective of ulcer aetiology. However, the risk was highest among patients with an arterial leg ulcer and lowest among those with a venous leg ulcer.
Previous research has shown rather unequivocally that mortality is increased among patients with diabetic foot ulcers (19, 20, 28–30), and also, several studies demonstrate an increased mortality associated with pressure ulcers (21–23). The current study included only a very small number of patients with diabetic foot ulcers and sporadic patients with pressure ulcers, so these patients do not explain the increased mortality associated with chronic ulcers in the present study. In parallel with the current findings of a increased mortality risk particularly among patients with arterial leg ulcers, peripheral arterial disease has been shown to independently associate with increased mortality risk (31, 32), and a doubled risk of death has been reported in a follow-up study consisting of 84 patients with arterial leg ulcers (19). In a Swedish study, the 5-year survival of patients with a venous ulcer was shown not to significantly differ from that of the controls (19). However, similar to the current study, a large register-based German study detected increased mortality for patients with a venous leg ulcer compared with that of the age-standardized mortality rate (24). In the current study, including a matched reference group, the HR for mortality among patients with a venous leg ulcer was slightly lower than that of all patients with ulcers, but still significantly elevated. Furthermore, the current study revealed that the mortality risk for patients diagnosed as having atypical ulcers was increased more than for patients with mixed or venous leg ulcers. Previous knowledge about the mortality of patients diagnosed as having an atypical ulcer is scarce, and, furthermore, the group is heterogenic, since the patients having atypical ulcers can have a wide spectrum of aetiologies causing the ulcers (15). In the current study, the majority of patients with atypical ulcers had vasculitis, and previous evidence showing increased mortality has consisted mainly of ANCA-associated vasculitic patients or also included patients with systemic vasculitis (33, 34). In addition, a slightly higher mortality risk has been found in patients with rheumatoid vasculitis (35, 36). Moreover, a rather large cohort study from the UK identified a 3-fold higher mortality risk associated with pyoderma gangraenosum compared with the general population controls (37). Malignant ulcers, which constituted only a minority of atypical ulcers within the current study, have been associated with a more than 3-fold increase in mortality risk compared with other ulcer aetiologies in a small Danish study consisting of home care patients (23). However, comparison between the results of different studies may be rather challenging, due to the discrepancies in study design, follow-up time and study population.
Similar to the findings of the current study, an association of an increased mortality risk among male patients with chronic ulcers has also been reported in other studies (20, 21, 23, 24, 27), and this observation has been, at least partly, explained by the general increased mortality associated with the male sex (38). However, this cannot explain the increased mortality associated with the male sex in the present study, since the mortality risk of male patients with ulcers was compared with that of their matched male references. Intriguingly, in the current study males were younger than females at the time of the first ulcer diagnosis, and also, younger age at the time of the first ulcer was associated with higher HR for mortality. Age might thus be associated with mortality among males, or else there are other explanatory factors, which we were unable to investigate in this register-based study (e.g. comorbidities), that might explain this association. Comorbidities are assumed to influence wound healing (13), and, for example, the presence of diabetes has also been shown to have a remarkable impact on the mortality risk of patients with chronic ulcers (19). In addition to diabetes, the common comorbidities in patients with ulcers are arterial hypertension, obesity, dyslipidaemia and metabolic syndrome, and a German multicentre study, consisting of 1,000 patients with ulcers, revealed that 80% of patients had one or several relevant comorbidities (13). Moreover, comorbidities have been shown to be more frequent in patients treated in wound centres, but, interestingly, this did not seem to have an effect on the mortality risk (39).
Another important finding of the current study was that the mortality risk was elevated in all age groups, but particularly among young patients affected with a chronic ulcer, and to our knowledge, this is a previously unreported finding. Furthermore, according to the current results, the mortality risk was higher for those patients with ulcers that only had one ulcer episode, although this is probably largely explained by the higher age of those patients, as younger patients have more time to develop chronic ulcer recurrences (19).
Overall, the knowledge that exists about causes of death among patients with ulcers is rather limited, and studies have mainly addressed patients with diabetic ulcers, whose main causes of death have been previously identified as cardiovascular events, diabetes and malignancies (20, 27). The current study thus provided new knowledge about causes of death among patients with ulcers in general and patients with different ulcer aetiologies, and the mortality risk was highest for diabetes, and increased particularly among patients with arterial and venous leg ulcers. It is well recognized that diabetes is a major risk factor for peripheral arterial disease, but diabetes has been previously also been found to be common among patients with venous and vasculitic ulcers (13). Moreover, the mortality for ischaemic heart disease was elevated among all, including for patients with arterial and venous leg ulcers, a result that is consistent with a Swedish study from the 1980s (40). Intriguingly, the mortality for digestive diseases was also increased: inflammatory bowel diseases are common comorbidities of pyoderma gangraenosum (15), but, other than that, the explanation remains obscure. Likewise, the reason for slightly increased mortality risk for malignancies among patients with chronic ulcers is unclear, but it might be attributed to the chronic inflammation associated with chronic ulcer or better diagnostics of malignancies among patients with ulcers treated at a hospital. Infections are a possible complication of chronic ulcers (14, 16, 21, 24, 27–30, 39), and, in this study, sepsis as an immediate cause of death was strongly associated with mortality among patients with chronic ulcers. This corresponds to the findings of a recent study demonstrating even a slightly higher HR (7.18 vs 5.86) for sepsis mortality among patients with venous leg ulcers (24). In addition, pneumonia as an underlying and also immediate cause of death was increased in patients with ulcers in the current study, even though to a lesser extent than sepsis, highlighting the risk and significance of infection complications in patients with chronic ulcers even further.
The major strengths of the current study were the large number of consecutive patients with ulcers included in the study cohort and the usage of a large matched reference group for comparison. The follow-up period of the current study is, to our knowledge, the longest reported to date. Furthermore, the mortality-register used has almost 100% coverage and is highly reliable. Moreover, to avoid bias associated with patients having consecutive ulcer episodes with different aetiologies when the mortality risk associated with each ulcer aetiology was investigated, patients having several ulcer aetiologies were excluded from the analysis. We must emphasize, however, that the current study included patients with ulcers who were from a single tertiary care centre treating mostly hard-to-heal ulcers, and it is therefore possible that the results are not reflective of the general population of patients with ulcers. However, the sex distribution, age and ulcer aetiology of the current study cohort was rather representative of a typical ulcer population described in previous chronic ulcer studies (5, 12–14, 24). A limitation of the current study was that, since the study design was retrospective and register-based, it was not possible to investigate all factors that might influence mortality. Also, the patients were selected using diagnostic codes for ulcers. In addition, the exact location and duration of each ulcer was unknown.
In conclusion, this study demonstrated an almost 2-fold increased long-term mortality among patients with chronic ulcers. The risk of death was elevated regardless of age, sex and ulcer aetiology, but particularly at risk were males with ulcers and those with an arterial leg ulcer. The current study highlights the importance of the effective management of comorbidities, especially diabetes, since the most common morbidities associated with chronic ulcers were shown to have the highest HR for death in this study. In addition, the prompt and accurate diagnosis and treatment of infections is of the utmost importance. Even though dermatologists are frequently key persons in ulcer diagnosis and treatment, the management of a multidisciplinary team is often required, in order to optimize treatment and improve the prognosis of patients with chronic ulcers.
ACKNOWLEDGEMENTS
The study was financially supported by the Competitive Research Funding of Tampere University Hospital (grants 9X061 and 9AA082) and the Finnish Dermatological Society.
REFERENCES
- Martin P, Nunan R. Cellular and molecular mechanisms of repair in acute and chronic wound healing. Br J Dermatol 2015; 173: 370–378.
- Kyaw BM, Järbrink K, Martinengo L, Car J, Harding K, Schmidtchen A. Need for improved definition of “chronic wounds” in clinical studies. Acta Derm Venereol 2018; 98: 157–158.
- Callam MJ, Ruckley CV, Harper DR, Dale JJ. Chronic ulceration of the leg: extent of the problem and provison of care. BMJ 1985; 290: 1855–1856.
- Nelzén O, Bergqvist D, Lindhagen A. The prevalence of chronic lower-limb ulceration has been underestimated: results of a validated population questionnaire. Br J Surg 1996; 83: 255–258.
- Graham ID, Harrison MB, Nelson EA, Lorimer K, Fischer A. Prevalence of lower-limb ulceration: a systematic review of prevalence studies. Adv Skin Wound Care 2003; 16: 305–316.
- Nussbaum SR, Carter MJ, Fife CE, DaVanzo J, Haught R, Nusgart M et al. An economic evaluation of the impact, cost, and Medicare policy implications of chronic nonhealing wounds. Value Health 2018; 21: 27–32.
- Guest JF, Ayoub N, Mcllwraith T, Uchegbu I, Gerrish A, Weidlich D et al. Health economy burden that wounds impose on the National Health Service in the UK. BMJ Open 2015; 5: e009283.
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2019: Highlights (ST/ESA/SER.A/430). 2019. [Accessed 2020 Sept 19]. Available from: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf.
- Heyer K, Herberger K, Protz K, Glaeske G, Augustin M. Epidemiology of chronic wounds in Germany: analysis of statutory health insurance data. Wound Repair Regen 2016; 24: 434–442.
- Moffatt CJ, Doherty DC, Smithdale R, Franks PJ. Clinical predictors of leg ulcer healing. Br J Dermatol 2010; 162: 51–58.
- Guest JF, Vowden K, Vowden P. The health economic burden that acute and chronic wounds impose on an average clinical commissioning group/health board in the UK. J Wound Care 2017; 26: 292–303.
- Körber A, Klode J, Al-Benna S, Wax C, Schadendorf D, Steinstraesser L et al. Etiology of chronic leg ulcers in 31,619 patients in Germany analyzed by an expert survey. J Dtsch Dermatol Ges 2011; 9: 116–121.
- Jockenhöfer F, Gollnick H, Herberger K, Isbary G, Renner R, Stücker M, et al. Aetiology, comorbidities and cofactors of chronic leg ulcers: retrospective evaluation of 1000 patients from 10 specialised dermatological wound care centers in Germany. Int Wound J 2016; 13: 821–828.
- Apollonio A, Antignani PL, Di Salvo M, Failla G, Guarnera G, Mosti G, et al. A large Italian observational multicentre study on vascular ulcers of the lower limbs (Studio Ulcere Vascolari). Int Wound J 2014; 13: 27–34.
- Isoherranen K, O’Brien JJ, Barker J, Dissemond J, Hafner J, Jemec GBE, et al. Atypical wounds. Best clinical practices and challenges. J Wound Care 2019; 28: 1–92.
- Kirsner RS, Vivas AC. Lower-extremity ulcers: diagnosis and management. Br J Dermatol 2015; 173: 379–390.
- Morton LM, Phillips TJ. Wound healing and treating wounds: differential diagnosis and evaluation of chronic wounds. J Am Acad Dermatol 2016; 74: 589–605.
- Renner R, Seikowski K, Simon JC. Association of pain level, health and wound status in patients with chronic leg ulcers. Acta Derm Venereol 2014; 94: 50–53.
- Nelzén O, Bergqvist D, Lindhagen A. Long-term prognosis for patients with chronic leg ulcers: a prospective cohort study. Eur J Vasc Endovasc Surg 1997; 13: 500–508.
- Iversen MM, Tell GS, Riise T, Hanestad BR, Østbye T, Graue M, et al. History of foot ulcer increases mortality among individuals with diabetes: ten-year follow-up of the Nord-Trøndelag Health Study, Norway. Diabetes Care 2009; 32: 2193–2199.
- Redelings MD, Lee NE, Sorvillo F. Pressure ulcers: more lethal than we thought? Adv Skin Wound Care 2005; 18: 367–372.
- Landi F, Onder G, Russo A, Bernabei R. Pressure ulcer and mortality in frail elderly people living in community. Arch Gerontol Geriatr 2007; 44: 217–223.
- Zarchi K, Martinussen T, Jemec GBE. Wound healing and all-cause mortality in 958 wound patients treated in home care. Wound Repair Regen 2015; 23: 753–758.
- Kreft D, Keiler J, Grambow E, Kischkel S, Wree A, Doblhammer G. Prevalence and mortality of venous leg diseases of the deep veins: an observational cohort study based on German Health Claims Data. Angiology 2020; 71: 452–464.
- Kimpimäki T, Huotari-Orava R, Antonen J, Vaalasti A. Increased incidence of cutaneous vasculitic ulcers: 30-year results from a population-based retrospective study. Acta Derm Venereol 2017; 97: 653–654.
- Statistics Finland, Classification of causes of death. [Accessed 2020 Nov 22]. Available from: https://www.stat.fi/en/luokitukset/kuolinsyyt/kuolinsyyt_61_19960101/0/.
- Morbach S, Furchert H, Gröblinghoff U, Hoffmeier H, Kersten K, Klauke GT, et al. Long-term prognosis of diabetic foot patients and their limbs: amputation and death over the course of a decade. Diabetes Care 2012; 35: 2021–2027.
- Ghanassia E, Villon L, Thuan Dit Dieudonné JF, Boegner C, Avignon A, Sultan A. Long-term outcome and disability of diabetic patients hospitalized for diabetic foot ulcers: a 6.5-year follow-up study. Diabetes Care 2008; 31: 1288–1292.
- Prompers L, Schaper N, Apelqvist J, Edmonds M, Jude E, Mauricio D, et al. Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study. Diabetologia 2008; 51: 747–755.
- Chammas NK, Hill RLR, Edmonds ME. Increased mortality in diabetic foot ulcer patients: the significance of ulcer type. J Diabetes Res 2016; 2016: 2879809.
- Golomb BA, Dang TT, Criqui MH. Peripheral arterial disease: morbidity and mortality implications. Circulation 2006; 114: 688–699.
- Criqui MH, Langer RD, Fronek A, Feigelson HS, Klauber MR, McCann TJ et al. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med 1992; 326: 381–386.
- Wallace ZS, Fu X, Harkness T, Stone JH, Zhang Y, Choi H. All-cause and cause-specific mortality in ANCA-associated vasculitis: overall and according to ANCA type. Rheumatology (Oxford) 2020; 59: 2308–2315.
- Arora A, Wetter DA, Gonzalez-Santiago TM, Davis MD, Lohse CM. Incidence of leukocytoclastic vasculitis, 1996 to 2010: a population-based study in Olmsted County, Minnesota. Mayo Clin Proc 2014; 89: 1515–1524.
- Turesson C, Jacobsson L, Bergstrom U. Extra-articular rheumatoid arthritis: prevalence and mortality. Rheumatology (Oxford) 1999; 38: 668–674.
- Voskuyl AE, Zwinderman AH, Westedt ML, Vandenbroucke JP, Breedveld FC, Hazes JM. The mortality of rheumatoid vasculitis compared with rheumatoid arthritis. Arthritis Rheum 1996; 39: 266–271.
- Langan SM, Groves RW, Card TR, Gulliford MC. Incidence, mortality, and disease associations of pyoderma gangrenosum in the United Kingdom: a retrospective cohort study. J Invest Dermatol 2012; 132: 2166–2170.
- Rosella LC, Calzavara A, Frank JW, Fitzpatrick T, Donnelly PD, Henry D. Narrowing mortality gap between men and women over two decades: a registry-based study in Ontario, Canada. BMJ Open 2016; 6: e012564.
- Escandon J, Vivas AC, Tang J, Rowland KJ, Kirsner RS. High mortality in patients with chronic wounds. Wound Repair Regen 2011; 19: 526–528.
- Hansson C, Andersson E, Swanbeck G. A follow-up study of leg and foot ulcer patients. Acta Derm Venereol 1987; 67: 496–500.