Widespread Papules in a 70-year-old Man: A Quiz
Italo F. Aromolo1,2*, Carlo A. Maronese1,2*, Giovanni Genovese1,2, Marco Cusini1 and Angelo V. Marzano1,2
1Dermatology Unit, Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Via Pace, 9, IT-20122 Milano and 2Department of Pathophysiology and Transplantation, Università degli Studi di Milano, Milan, Italy. E-mail: italo.aromolo@unimi.it
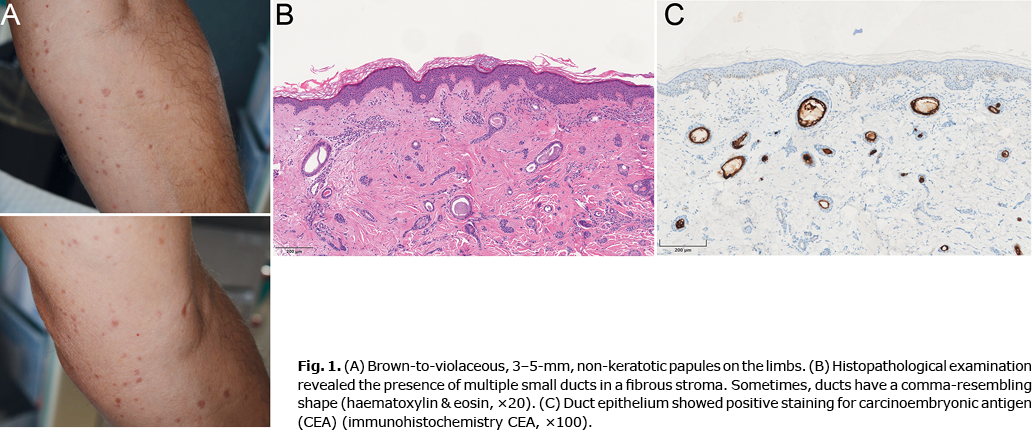
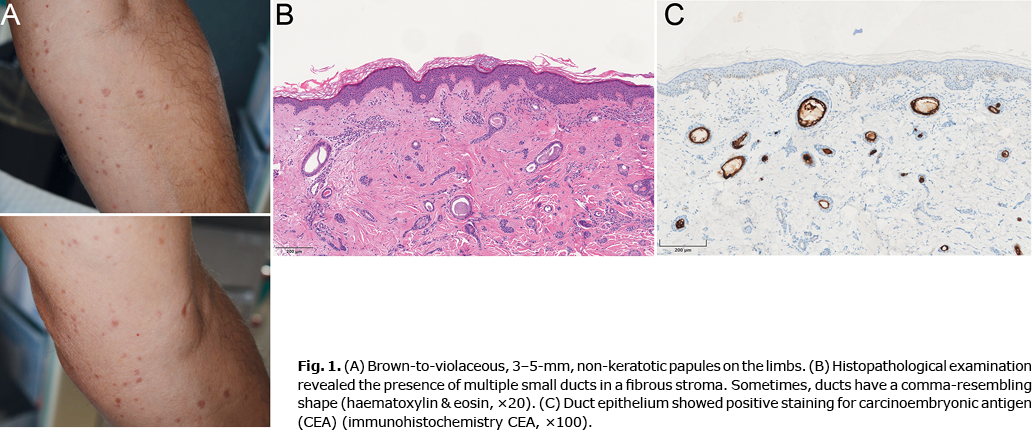
An otherwise healthy 70-year-old man presented to our dermatology unit with a 5-year history of a waxing and waning dermatosis. The eruption had a tendency to recur during the summer months, although no definitive association with sun exposure was documented. Physical examination revealed numerous, flat-topped, brown-to-violaceous, 3–5-mm non-keratotic papules, disseminated on his neck, trunk, and limbs (Fig. 1A). Dermoscopy was non-specific/unremarkable, as only a fine pigment network could be seen. The lesions were mildly pruritic. Darier’s sign was negative. Histopathological examination revealed a normal epidermis, and multiple dermal ducts lined by 1 or 2 layers of cuboidal epithelium (Fig. 1B). Some of the ducts had a tadpole or comma morphology, with positive carcinoembryonic antigen (CEA) immunostaining in the duct epithelium (Fig. 1C).
What is your diagnosis? See next page for answer.
Widespread Papules in a 70-year-old Man: A Commentary
Acta Derm Venereol 2022; 102: adv00705.
DOI: 10.2340/actadv.v102.853
Diagnosis: Syringoma
Syringoma are benign adnexal tumours arising from eccrine or apocrine gland ducts (1). They typically present as multiple skin-coloured to reddish-brown, flat-topped, non-scaly, firm, discrete, 2–4-mm papules. Syringoma are usually asymptomatic, or rarely mildly pruritic. Typically, the periorbital area is involved, although any body-site may be involved. Eruptive syringoma is a generalized variant of syringoma, consisting of successive crops of lesions on the neck, trunk and limbs. Eruptive syringoma most frequently appear during adolescence or early adulthood, sometimes with a positive family history (2). An association with Down syndrome (3) and with hyperthyroidism (4) has been described.
On histopathology (5), the dermis is primarily involved: multiple small ducts, surrounded by 2 layers of cuboidal epithelial cells, are scattered in a fibrous stroma. Sometimes, ducts have a curved, comma-resembling, shape. Basal melanosis can often be seen. Syringoma exhibit an immunohistochemical pattern similar to normal eccrine ducts (CK6, CK19 and CEA in luminal cells) (6). Positive CEA expression enables differentiation of syringoma from desmoplastic trichoepithelioma, in which it is usually negative (7). Common dermoscopic features of syringoma include a delicate brown pigment network with a reddish background (8).
We report here a case of eruptive syringoma in a 70-year-old man. Differential diagnoses of eruptive syringoma include some chronic, diffuse, papular eruptions, such as mastocytosis and lichen planus. In contrast to mastocytosis, Darier’s sign is negative and pruritus is usually absent in syringoma (9). Lichen planus papules are violaceous, finely scaly and usually itchy, in contrast to syringoma. The presence of Wickham striae is also a clue (10). Clinical diagnosis in the current case was challenging, due to the late onset and pruritic presentation. In a case series of 27 patients with eruptive syringoma (2), the correct diagnosis was clinically hypothesized only in 8 patients.
Given the benign prognosis and the absence of symptoms, treatment of syringomas is exclusively cosmetic. Therapeutic options are various and not standardized, and include surgical excision, cryotherapy, chemical peeling, electrodessication with curettage and CO2 laser (11–13). However, the aesthetic outcome is not always satisfactory.
ACKNOWLEDGEMENTS
This study was conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national), according to the principles of the Declaration of Helsinki 1975, as revised in 2000, and with the Taipei Declaration.
Anonymized data will be shared upon reasonable request from any qualified investigator for purposes of replicating procedures and results.
The authors have no conflicts of interest to declare.
REFERENCES
- Bolognia JL, Schaffer JV, Cerroni L. Dermatology. Second edition. Maryland Heights, MO: Mosby Elsevier, 2008: p.1704.
- Soler-Carrillo J, Estrach T, Mascaró JM. Eruptive syringoma: 27 new cases and review of the literature. J Eur Acad Dermatol Venereol 2001; 15: 242–246.
- Thomas L, Chamchikh N, Audefray D, Moulin G. Syringoma and trisomy 21. Ann Dermatol Venereol 1993; 120: 689–691.
- Polat M, Pelitli A, Oztaş P, Unal T, Alli N. Eruptive syringoma associated with hyperthyroidism. Skinmed 2010; 8: 124–125.
- Weedon D. Eccrine tumors: a selective review. J Cutan Pathol 1984; 11: 421–436.
- Ohnishi T, Watanabe S. Immunohistochemical analysis of keratin expression in clear cell syringoma: a comparative study with conventional syringoma. J Cutan Pathol 1997; 24: 370–376.
- Landau-Price D, Barnhill RL, Kowalcyzk AP, Penneys NS, Ziegels-Weissman J. The value of carcinoembryonic antigen in differentiating sclerosing epithelial hamartoma from syringoma. J Cutan Pathol 1985; 12: 8–12.
- Botsali A, Caliskan E, Coskun A, Tunca M. Eruptive syringoma: two cases with dermoscopic features. Skin Appendage Disord 2020; 6: 319–322.
- Bergström A, Rollman O, Emtestam L, Mattson M, Hägglund H, Nilsson G, Karlsson M. Cutaneous mastocytosis – update and clinical guidelines. Lakartidningen 2018; 115: FASY.
- Gorouhi F, Davari P, Fazel N. Cutaneous and mucosal lichen planus: a comprehensive review of clinical subtypes, risk factors, diagnosis, and prognosis. ScientificWorldJournal 2014; 2014: 742826.
- Belardi MG, Maglione MA, Vighi S, di Paola GR. Syringoma of the vulva. A case report. J Reprod Med 1994; 39: 957–959.
- Karam P, Benedetto AV. Intralesional electrodessication of syringomas. Dermatol Surg 1997; 23: 921–924.
- Wang JL, Roenigk HH Jr. Treatment of multiple facial syringomas with the carbon dioxide laser. Dermatol Surg 1999; 25: 136–139.