This post hoc analysis examined SCORing Atopic Dermatitis (SCORAD) outcomes in 471 paediatric patients (children age 6–<12 years, n = 304; adolescents age 12–<18 years, n = 167) with atopic dermatitis treated with dupilumab, ± topical corticosteroids, in two 16-week phase 3 randomized controlled trials and a 1-year interim data cut of a subsequent open-label extension study. Paediatric patients treated with dupilumab (± topical corticosteroids) had significantly lower SCORAD, objective SCORAD (o-SCORAD), and individual SCORAD components from week 3 to 16 compared with placebo (± topical corticosteroids) in the randomized controlled trials. The results were sustained or continuously improved over 1 year of open-label treatment with dupilumab ± topical corticosteroids. SCORAD-50 was achieved in almost all patients (91.3–91.8%) by week 52 with continued dupilumab treatment across age groups. Almost all (> 86%) patients achieved mild or absent pruritus and sleep loss at week 52. In conclusion, dupilumab ± topical corticosteroids resulted in rapid and significant improvements in all aspects of SCORAD analysed, and the results were sustained over 1 year.
Key words: atopic dermatitis; SCORAD; dupilumab; paediatric.
Accepted Apr 8, 2022; Epub ahead of print Apr 8, 2022
Acta Derm Venereol 2022; 102: adv00726.
DOI: 10.2340/actadv.v102.854
Corr: Ana B. Rossi, Sanofi, 450 Water Street, Cambridge, MA, USA. E-mail: Ana.Rossi@sanofi.com
SIGNIFICANCE
Paediatric patients treated with dupilumab (± topical corticosteroids) had improvements in all aspects of SCORAD from week 3 to 16 compared with placebo (± topical corticosteroids) during 16 weeks. These results were sustained or continuously improved over 1 year of open-label treatment with dupilumab ± topical corticosteroids.
INTRODUCTION
Atopic dermatitis (AD), one of the most common chronic relapsing inflammatory dermatoses in the paediatric population, has a prevalence of up to 22.6% (1, 2). Moderate-to-severe AD is highly symptomatic and can have a profound multidimensional burden on children, adolescents, and their families, and symptoms such as pruritus and sleep loss contribute to reduced quality of life (QoL) (3, 4). Increased likelihood of attention deficit disorders, anxiety, and depression are common, as well as type 2 inflammatory comorbidities, such as asthma and allergic rhinitis (5–7).
Numerous clinical tools have been developed to assess AD severity (8–10). The most commonly used and validated scoring systems include the Eczema Area and Severity Index (EASI) and SCORing Atopic Dermatitis (SCORAD) (11, 12). SCORAD is an AD-specific validated measurement scale (0–103), which incorporates investigator assessment of affected body surface area (BSA) and severity of 6 disease signs, as well as patient-reported symptoms of pruritus and sleep loss. In contrast, EASI entails clinical assessment of the extent and severity of 4 disease signs in 4 anatomical body regions and does not include subjective symptoms. EASI is often used in clinical trials, whereas SCORAD is used in many countries by dermatologists to regularly assess disease severity and guide treatment decisions, as it is a more holistic representation of disease burden. The European Task Force on Atopic Dermatitis (ETFAD) recommends using SCORAD to measure overall disease severity and burden of AD and evaluate treatment response (13, 14). Moreover, the current European guidelines for diagnosis and treatment of AD propose a step-up/step-down treatment algorithm based on SCORAD (13, 14).
Dupilumab, a fully human monoclonal antibody, was shown in phase 3 randomized controlled trials (RCTs), ± topical corticosteroids (TCS), to significantly improve AD signs, symptoms, and QoL with an acceptable safety profile in adolescents and children with moderate-to-severe or severe AD through week 16, and through week 52 in open-label extension (OLE) studies (15–17). SCORAD was included as a secondary outcome in these studies to measure overall disease severity, and treatment response.
The aim of this study was to report the effects of dupilumab (± TCS) on total SCORAD and its components (objective and subjective SCORAD, BSA, individual signs and symptoms) in children age 6–<12 years with severe AD and adolescents age 12–<18 years with moderate-to-severe AD in 16-week phase 3 RCTs and a subsequent long-term OLE up to 1 year.
PATIENTS AND METHODS
Study design
This post hoc analysis includes data from 2 RCTs and an OLE study in children (6–< 12 years) and adolescents (12–< 18 years): LIBERTY AD PEDS (NCT03345914) (15); LIBERTY AD ADOL (NCT03054428) (17); and 1-year interim data from the ongoing 5-year OLE study, LIBERTY AD PEDS OLE (NCT02612454) (16). Detailed methodology, primary efficacy, and safety results were reported previously for the RCT studies (15–17).
The RCT LIBERTY AD ADOL included patients aged 12–< 18 years with moderate-to-severe AD, randomized to placebo or 1 of 3 dupilumab monotherapy groups: 300 mg every 4 weeks (q4w) regardless of baseline weight; or every 2 weeks (q2w) (weight < 60 kg: 200 mg q2w, weight ≥ 60 kg: 300 mg q2w)). LIBERTY AD PEDS (RCT) included patients 6–< 12 years with severe AD, randomized to placebo plus TCS (other topical anti-inflammatory permitted) or 1 of the 3 dupilumab doses + TCS: 300 mg q4w regardless of baseline weight, or 100 mg q2w if < 30 kg, or 200 mg q2w if ≥ 30 kg. In the PEDS OLE study, an ongoing longitudinal open-label extension safety study enrolling both placebo and dupilumab-treated patients who completed a parent RCT, all patients receive dupilumab weekly. In the original protocol, the dose regime was 2 mg/kg or 4 mg/kg weekly (qw); however, after protocol amendment the weight-based dose was changed to a fixed dose of 300 mg q4w with an up-titration in case of inadequate response (defined as failure to achieve clear or almost clear skin according to investigator’s assessment) at week 16 (200 mg q2w in patients with baseline weight < 60 kg, or 300 mg q2w in patients with baseline weight ≥ 60 kg).
All trials were approved by the respective institutional review boards and conducted in accordance with the ethical principles outlined in the Declaration of Helsinki, the International Conference on Harmonization Good Clinical Practice guidelines (18), and applicable regulatory requirements. All patients or caregivers provided written informed assent before entering the trials.
Assessments
The assessments used in this post hoc analysis included SCORAD and its constituent components assessed by investigator and patient/caregiver (19). SCORAD comprises 3 components: Part A, the extent of disease (investigator-assessed) 0–100%; Part B, the intensity of signs of disease (investigator-assessed); and Part C, symptoms (patient/caregiver assessed). Each of the 5 signs (Fig. 1: erythema, oedema/papulation, excoriation, lichenification, oozing/crusting) is graded 0–3 in a target lesion considered by the investigator as representative of global disease severity. The sixth sign, dryness, is assessed on non-lesional areas. Signs scores of 0 correspond to none, 1 correspond to mild, 2 correspond to moderate, and 3 correspond to severe. Part C includes the 2 most important symptoms in AD, pruritus (itch) and sleep loss, which patients or caregivers assess the average value for the last 3 days or nights using a visual analogic scale (VAS) (0–10). Fig. 1 shows photographs with examples of severity of the 5 signs assessed in lesional skin.

SCORAD was assessed at screening, baseline, weeks 1, 2, 4, 6, 8, 12, and 16 in the RCT studies, and every 4 weeks thereafter through week 52 in the OLE. The following severity bands were used in these analyses: for SCORAD mild (< 25), moderate (25–50), and severe (> 50); for objective SCORAD (o-SCORAD) clear (0–7.9), mild (8.0–23.9), moderate (24.0–37.9), and severe (38.0–83); for SCORAD pruritus VAS and sleep loss VAS: none (0), mild (> 0 –< 4), moderate (4–< 7), severe (7–< 9), and very severe (9–10).
This analysis includes results over time for each study for the following outcome measures: SCORAD, o-SCORAD, SCORAD- 50 (50% improvement from baseline in total SCORAD), SCORAD component scores (Parts A, B, and C), percent change from baseline in total SCORAD, categorical changes in SCORAD severity according to the severity strata outlined previously (11, 13), categorical changes in individual signs severity over time, the percentage reduction in Parts A, B, and C, change in absolute values from baseline to week 16 or 52 for SCORAD, o-SCORAD, Part A, Part B, and Part C, individual symptoms (pruritus VAS and sleep loss VAS).
Statistical analysis
Efficacy analyses were performed on the full analysis set, which included all randomized patients. For continuous outcomes (SCORAD, o-SCORAD, and SCORAD components), patients missing an assessment or who received rescue treatment were considered “non-responders” (censoring) and imputed using the multiple imputation method. The p-values for categorical endpoints were derived by a Cochran-Mantel-Haenszel (CMH) test stratified by region (North America vs Europe) and baseline weight category (for children 6–< 12 years, < 30 kg and ≥ 30 kg and for adolescents 12–< 18 years, < 60 kg and ≥ 60 kg). For categorical outcomes (SCORAD-50, SCORAD components by severity strata), patients who received rescue treatment were considered non-responders after rescue treatment use (non-responder imputation). Significance values were considered nominal for all analyses. For Sankey plots of changes in SCORAD severity over time, values were set to missing after rescue treatment, and missing total SCORAD scores were set to the highest category (severe). Analyses were performed using SAS V9.4 or higher.
RESULTS
Patients
In this analysis, 304 children (aged 6–<12 years) were randomized to placebo or dupilumab (both with TCS); 146 continued treatment in the long-term extension study of dupilumab, with 110 completing 52 weeks of treatment at the interim database lock. A total of 167 adolescents (aged 12–<18 years) were randomized to placebo or dupilumab (monotherapy); 46 continued treatment with dupilumab in the OLE study (+ optional TCS), with 36 completing 52 weeks of treatment.
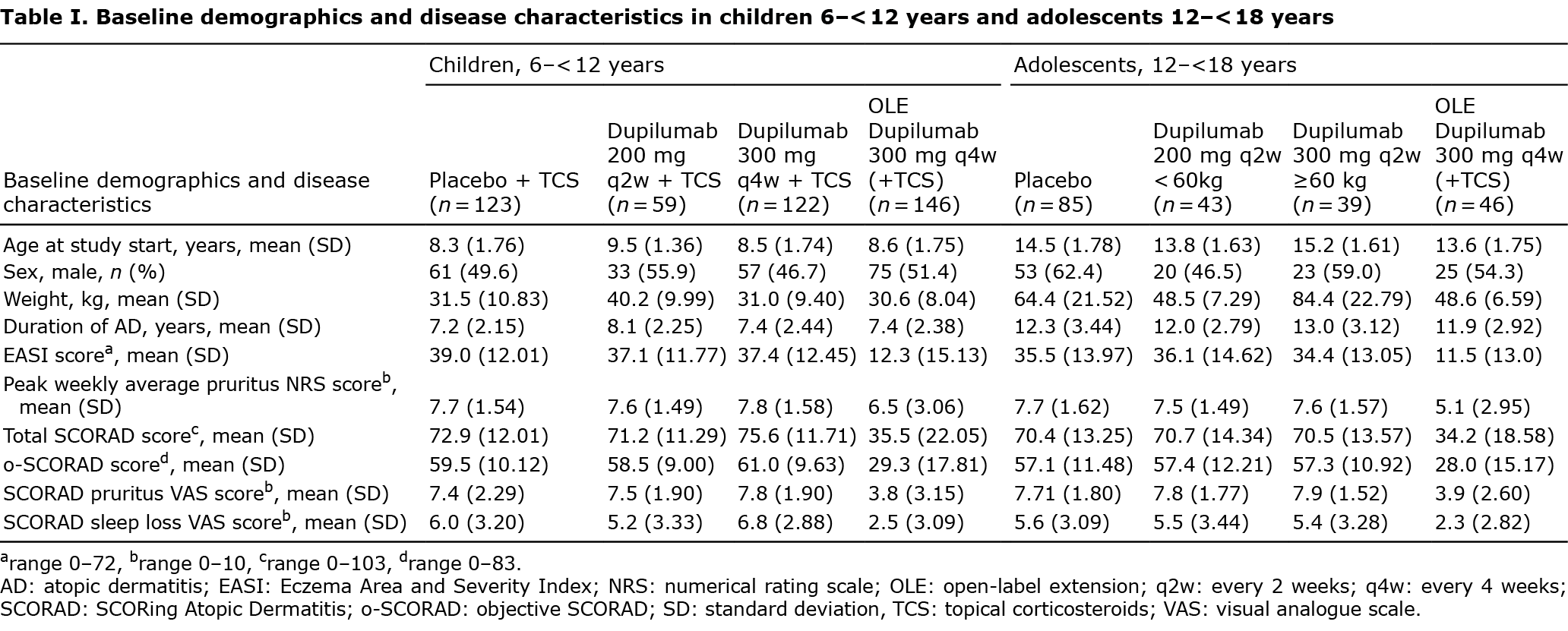
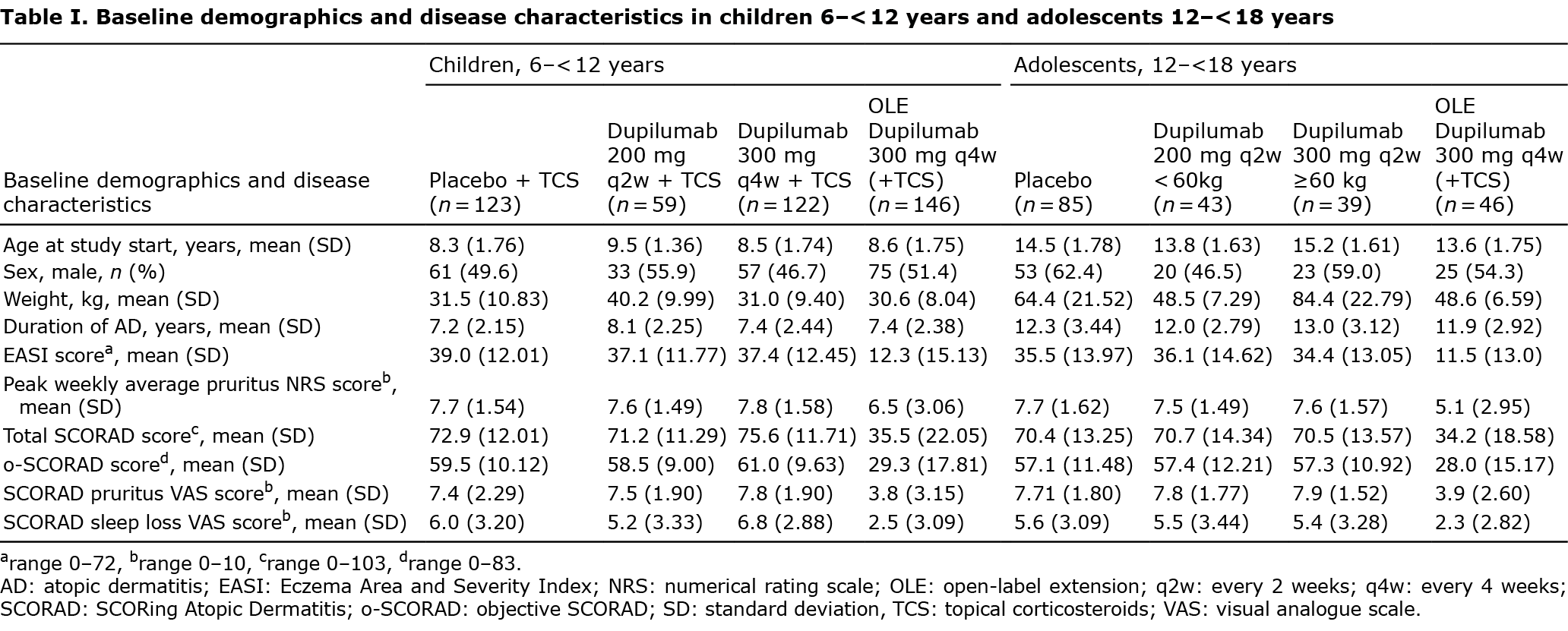
Baseline characteristics were balanced between the placebo and dupilumab groups in the RCTs (Table I), and all patients in both studies had severe SCORAD at baseline (Fig. 2). At the start of the OLE, SCORAD was lower due to the prior 16 weeks of treatment received.

Efficacy analysis by SCORAD, o-SCORAD, and SCORAD-50
Least squares (LS) mean SCORAD and o-SCORAD declined rapidly in all dupilumab treatment groups and continued to improve over time with early and progressively widening differentiation from placebo across age groups. Scores were significantly lower in all dupilumab-treated groups compared with placebo from week 3 (p < 0.05) through week 16 (p < 0.0001, Fig. 2). This downward trend continued with open-label use of dupilumab 300 mg q4w through 1 year in both children (age 6–< 12 years) and adolescents (age 12–< 18 years). Approximately 71–75% of children and 42–46% of adolescents treated with dupilumab achieved SCORAD-50 at the end of the 16-week randomized treatment period (vs 7–23% of control), and almost all (> 90%) following subsequent 1-year open-label treatment (Fig. 2).
The proportion of patients in each SCORAD severity category shifted over time in both age groups, with more than two-thirds of children and adolescents achieving mild SCORAD by 1 year of continued dupilumab treatment (Fig. 3).

SCORAD components
A large number of patients had moderate or severe scores for individual signs and symptoms at baseline, all of which reduced significantly by week 16 (Table II). By week 3, significantly more dupilumab-treated patients in both age groups achieved lower overall BSA and pruritus vs control (Table II, p < 0.05). Overall, BSA declined from a mean of 54.6 at baseline to ~16% at week 16 in children in the dupilumab 300 mg q4w group (vs 35.5% for placebo + TCS, p < 0.0001) and from a mean of 55.6–56.5% at baseline to ~ 25–28% in adolescents (vs 44.8% for placebo, p < 0.001), and further decline to ~8% for both age groups after 1 year of treatment (Fig. 4). Most children and adolescents had severe or very severe pruritus VAS scores at baseline, and improvement was observed in dupilumab-treated patients vs placebo within the first month of treatment, from week 2 in children and from week 3 in adolescents. Similar results were observed with sleep loss VAS. Almost all (> 86%) patients reached mild or absent pruritus and sleep loss at week 52 (Fig. S1).


Fig. 4 shows progressive improvements in mean absolute SCORAD components from baseline to the RCT end of treatment (week 16) and then through 1 year of the OLE. Uniformly moderate, severe, or very severe disease at baseline improved to mild or absent disease activity across SCORAD components by week 52 of the OLE in both age groups.
SCORAD signs
Severity of all SCORAD signs decreased by week 16 with dupilumab ± TCS in comparison with placebo/control, including lichenification. Improvement in severity of signs continued over 52 weeks (Table II). Of all signs measured, oozing and excoriation reduced the most, reaching a reduction of 88–90% and 75–82% by week 52, respectively.
Safety
Detailed safety results were reported for the RCT studies previously (15–17). Briefly, during the RCT study in children, the rates of Treatment-Emergent Adverse Events (TEAE) were lower in the dupilumab + TCS groups than in the placebo + TCS control arm. In adolescents, overall TEAE rates were similar in the placebo and dupilumab groups. Serious TEAE rates were very low, not different from placebo, and not related to study drug. No deaths or treatment-related events of hypersensitivity or anaphylaxis occurred. As in adult dupilumab trials, injection-site reactions were more common with dupilumab than with placebo, occurring in 8.5% and 11.2% of dupilumab-treated adolescents and children vs 3.5 and 5.8% in the placebo groups, respectively. Conjunctivitis also occurred more frequently with dupilumab: occurring in 9.8% of adolescents and 7.3% of children treated with dupilumab vs 4.7 and 4.2% treated with placebo, respectively. Most cases of conjunctivitis were of mild-moderate severity, resolved during treatment, and did not lead to discontinuation of treatment. Skin infections were less common in the dupilumab-treated patients vs placebo in both age groups. Overall, dupilumab had an acceptable safety profile across all studies, with commonly reported adverse events consistent with the adult trials.
DISCUSSION
This post hoc analysis demonstrates that dupilumab monotherapy in adolescents and dupilumab with TCS in children significantly improves SCORAD outcomes in 16-week randomized control trials, with continued progressive improvements observed over 52-week open-label use. Rapid improvement was seen with dupilumab across all SCORAD components evaluating signs and symptoms in both age groups, with significant improvements in itch and sleep vs placebo/control as early as week 1 or 2 (following 1 dose of dupilumab) as measured by pruritus and sleep loss VAS.
Most children and adolescents achieved mild or absent pruritus and sleep loss by week 16, both of which are known contributors to diminished QoL in paediatric patients, these results are consistent with prior analyses showing improvement in the Patient-Oriented Eczema Measure (POEM) and Children’s Dermatology Life Quality Index (CDLQI) (15, 17). Sleep loss, in particular, is detrimental to the health of patients with AD, leading to increased fatigue, and decreased alertness, and is associated with a range of neuropsychiatric sequelae, including attention deficit disorders, anxiety, and depression (20–23). As AD is a chronic disease, sustained benefits of dupilumab were observed over 1 year, with almost all patients achieving either mild or absent symptoms at week 52.
Recently, SCORAD-35 was shown to be a good metric of disease improvement for clinical practice (12), and in this study, children reached this endpoint as early as week 3 with dupilumab + TCS, and adolescents as early as week 2; and 99.3% of children and 100% of adolescents achieving the SCORAD-35 endpoint by week 52 in the OLE study.
Scoring metrics are an essential part of assessing disease severity and treatment response. Although the EASI score is recommended by the Harmonizing Outcome Measures for Eczema (HOME) initiative as the core outcome instrument for measuring AD signs in clinical trials (24), both EASI and o-SCORAD were validated extensively, with SCORAD in frequent use in clinical trials and clinical practice worldwide. SCORAD was also reported to have numerically stronger correlation with patient-reported severity than EASI (25). Localized severe lesions, including lesions in functionally important (i.e. extremities) or aesthetically sensitive (i.e. face) areas, are also specifically captured by SCORAD (26, 27).
Dupilumab demonstrated efficacy across individual signs, which may indicate activity across AD pathomechanisms and phases of disease. Erythema, oozing, and excoriations tend to be signs of “acute or subacute” activity, while lichenification represents more gradual skin remodelling due to chronic inflammation, pruritus, and repeated scratching and/or rubbing (28). Lichenification is histologically hallmarked by epidermal acanthosis and dermal fibrosis, and is a particularly recalcitrant sign in AD, often slow to improve or entirely resistant to treatment (29). This study showed that most patients had improvement in lichenification across all dupilumab groups in the randomized controlled studies, with open-label dupilumab treatment. Significant reduction in dryness, assessed in non-lesional areas, indicates the benefits of dupilumab on skin-barrier in AD, possibly suggesting structural normalization and improved moisture retention. Type 2 inflammation is known to contribute to skin-barrier dysfunction in AD, and previous studies have shown that dupilumab significantly improved abnormalities in skin-barrier gene expression and epidermal proliferation in patients with AD (30–33). Dupilumab’s potential to restore the skin-barrier have been be confirmed clinically by evaluating improvement in trans-epidermal water loss (TEWL) and pre- and post-treatment profiling of structural protein and lipid components of the upper epidermal layers (34). Last, among AD signs, oozing and excoriation showed greatest overall reduction in both dupilumab cohorts, which may correlate with the substantial relief of pruritus also observed in this analysis.
Strengths of this analysis include the 1 year of data collection following the RCT studies. The post hoc nature of the analysis is a limitation, as only total SCORAD and BSA were included as secondary outcomes in the RCT studies. In addition, TCS use in some study arms may obscure the potential benefits of dupilumab alone.
In conclusion, dupilumab ± TCS compared with placebo ± TCS resulted in rapid, sustained, and statistically and clinically significant improvements in BSA affected, AD signs, pruritus, and sleep loss, as assessed by total SCORAD and its components, in children with severe AD and in adolescents with moderate-to-severe AD through week 16. After a 1-year extension of treatment with dupilumab most patients achieved scores of mild/minimal or no disease.
ACKNOWLEDGEMENTS
Research sponsored by Sanofi and Regeneron Pharmaceuticals, Inc. Medical writing and editorial support was provided by Carolyn Ellenberger, PhD, of Excerpta Medica, funded by Sanofi and Regeneron Pharmaceuticals, Inc.
We thank patients and investigators who participated in the studies; Adriana Mello, and El-Bdaoui Haddad of Sanofi; and Linda Williams of Regeneron Pharmaceuticals, Inc.
Clinical trial registration: LIBERTY AD ADOL: ClinicalTrials.gov Identifier: NCT03054428; EudraCT: 2015-004458-16. LIBERTY AD PEDS: ClinicalTrials.gov Identifier: NCT03345914; EudraCT: 2016-004997-16. LIBERTY AD PEDS OLE: ClinicalTrials.gov Identifier: NCT02612454; EudraCT: 2015-001396-40.
Conflicts of interest: AW: Beiersdorf, Eli Lilly, Galderma, LEO Pharma, MedImmune, Novartis, Pfizer, Regeneron Pharmaceuticals, Inc., Sanofi – investigator; AbbVie, Almirall, Anacor Pharmaceuticals, Eli Lilly, Galapagos, Galderma, LEO Pharma, MedImmune, Novartis, Pfizer, Regeneron Pharmaceuticals, Inc., Sanofi – consultant; Beiersdorf, LEO Pharma, Pierre Fabre – research grants. DM: AbbVie, Amgen, Eli Lilly, Janssen, LEO Pharma, Novartis, Pfizer, Sanofi, Regeneron Pharmaceuticals, Inc – investigator; AbbVie, Amgen, BMS, Eli Lilly, Janssen, LEO Pharma, Novartis, Pfizer, Regeneron Pharmaceuticals, Inc., Sanofi, UCB – consultant; AbbVie, Amgen, BMS, Novartis, Pfizer, Regeneron Pharmaceuticals, Inc., Sanofi – speaker. JIS: AbbVie, BMS, Eli Lilly, GlaxoSmithKline, Incyte, Kiniksa Pharmaceuticals, LEO Pharma, Realm Therapeutics, Regeneron Pharmaceuticals, Inc. – investigator; AbbVie, Eli Lilly, Galderma, GlaxoSmithKline, Incyte, Kiniksa Pharmaceuticals, LEO Pharma, MedImmune (AstraZeneca), Menlo Therapeutics, Pfizer, Realm Therapeutics, Regeneron Pharmaceuticals, Inc. – consultant; Regeneron Pharmaceuticals, Inc. – speaker. VA: Sanofi – Eli Lilly (clinical trials) LEO Pharma, Sanofi and AbbVie (consultant) honoraria. EB: Almirall, Pierre Fabre Dermatologie, Regeneron Pharmaceuticals, Inc., Sanofi – consultant; Eli Lilly, LEO Pharma, Novartis, Pfizer – investigator. NL, HZ: Regeneron Pharmaceuticals, Inc. − employees and shareholders. AT: consultant for Pierre Fabre, Galderma, Novartis, Johnson and Johnson, Incyte, Abbvie, Modilac, Pfizer, Lilly, Arena, Bioderma, Sanofi, and Regeneron. ABR: Sanofi – employee, may hold stock and/or stock options in the company.
REFERENCES
- Silverberg JI, Barbarot S, Gadkari A, Simpson EL, Weidinger S, Mina-Osorio P, et al. Atopic dermatitis in the pediatric population: a cross-sectional, international, epidemiologic study. Ann Allergy Asthma Immunol 2021; 126: 417–428.e2.
- Bylund S, Kobyletzki LB, Svalstedt M, Svensson Å. Prevalence and incidence of atopic dermatitis: a systematic review. Acta Derm Venereol 2020; 100: adv00160.
- Slattery MJ, Essex MJ, Paletz EM, Vanness ER, Infante M, Rogers GM, et al. Depression, anxiety, and dermatologic quality of life in adolescents with atopic dermatitis. J Allergy Clin Immunol 2011; 128: 668–671.
- Yang EJ, Beck KM, Sekhon S, Bhutani T, Koo J. The impact of pediatric atopic dermatitis on families: a review. Pediatr Dermatol 2019; 36: 66–71.
- Silverberg JI, Barbarot S, Gadkari A, Simpson EL, Weidinger S, Mina-Osorio P, et al. Atopic dermatitis in the pediatric population: a cross-sectional, international epidemiologic study. Ann Allergy Asthma Immunol 2021; 126: 417–28.e2.
- Gilaberte Y, Pérez-Gilaberte JB, Poblador-Plou B, Bliek-Bueno K, Gimeno-Miguel A, Prados-Torres A. Prevalence and comorbidity of atopic dermatitis in children: a large-scale population study based on real-world data. J Clin Med 2020; 9: 1632.
- Huang AH, Roh YS, Sutaria N, Choi J, Williams KA, Canner JK, et al. Real-world comorbidities of atopic dermatitis in the pediatric ambulatory population in the United States. J Am Acad Dermatol 2021; 85: 893–900.
- Wollenberg A, Barbarot S, Bieber T, Christen-Zaech S, Deleuran M, Fink-Wagner A, et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part I. J Eur Acad Dermatol Venereol 2018; 32: 657–682.
- Wollenberg A, Barbarot S, Bieber T, Christen-Zaech S, Deleuran M, Fink-Wagner A, et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part II. J Eur Acad Dermatol Venereol 2018; 32: 850–878.
- Eichenfield LF, Tom WL, Chamlin SL, Feldman SR, Hanifin JM, Simpson EL, et al. Guidelines of care for the management of atopic dermatitis: section 1. Diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol 2014; 70: 338–351.
- Chopra R, Vakharia PP, Sacotte R, Patel N, Immaneni S, White T, et al. Severity strata for Eczema Area and Severity Index (EASI), modified EASI, Scoring Atopic Dermatitis (SCORAD), objective SCORAD, Atopic Dermatitis Severity Index and body surface area in adolescents and adults with atopic dermatitis. Br J Dermatol 2017; 177: 1316–1321.
- Silverberg JI, Lei D, Yousaf M, Janmohamed SR, Vakharia PP, Chopra R, et al. What are the best endpoints for Eczema Area and Severity Index and Scoring Atopic Dermatitis in clinical practice? A prospective observational study. Br J Dermatol 2021; 184: 888–895.
- Wollenberg A, Oranje A, Deleuran M, Simon D, Szalai Z, Kunz B, et al. ETFAD/EADV Eczema task force 2015 position paper on diagnosis and treatment of atopic dermatitis in adult and paediatric patients. J Eur Acad Dermatol Venereol 2016; 30: 729–747.
- Wollenberg A, Christen-Zäch S, Taieb A, Paul C, Thyssen JP, de Bruin-Weller M, et al. ETFAD/EADV Eczema task force 2020 position paper on diagnosis and treatment of atopic dermatitis in adults and children. J Eur Acad Dermatol Venereol 2020; 34: 2717–2744.
- Paller AS, Siegfried EC, Thaçi D, Wollenberg A, Cork MJ, Arkwright PD, et al. Efficacy and safety of dupilumab with concomitant topical corticosteroids in children 6 to 11 years old with severe atopic dermatitis: a randomized, double-blinded, placebo-controlled phase 3 trial. J Am Acad Dermatol 2020; 83: 1282–1293.
- Cork MJ, Thaçi D, Eichenfield LF, Arkwright PD, Hultsch T, Davis JD, et al. Dupilumab in adolescents with uncontrolled moderate-to-severe atopic dermatitis: results from a phase IIa open-label trial and subsequent phase III open-label extension. Br J Dermatol 2020; 182: 85–96.
- Simpson EL, Paller AS, Siegfried EC, Boguniewicz M, Sher L, Gooderham MJ, et al. Efficacy and safety of dupilumab in adolescents with uncontrolled moderate to severe atopic dermatitis: a phase 3 randomized clinical trial. JAMA Dermatol 2020; 156: 44–56.
- Battisti WP, Wager E, Baltzer L, Bridges D, Cairns A, Carswell CI, et al. Good publication practice for communicating company-sponsored medical research: GPP3. Ann Intern Med 2015; 163: 461–464.
- Severity scoring of atopic dermatitis: the SCORAD index. Consensus Report of the European Task Force on Atopic Dermatitis. Dermatology 1993; 186: 23–31.
- McKenzie C, Paller AS, Fishbein A, Silverberg JI. Association between the longitudinal course of AD, sleep disturbance, and overall health in US children. J Allergy Clin Immunol Pract 2020; 8: 812–814.e1.
- Silverberg JI, Garg NK, Paller AS, Fishbein AB, Zee PC. Sleep disturbances in adults with eczema are associated with impaired overall health: a US population-based study. J Invest Dermatol 2015; 135: 56–66.
- Fishbein AB, Cheng BT, Tilley CC, Begolka WS, Carle AC, Forrest CB, et al. Sleep disturbance in school-aged children with atopic dermatitis: prevalence and severity in a cross-sectional sample. J Allergy Clin Immunol Pract 2021; 9: 3120–3129.e3.
- Fishbein AB, Mueller K, Kruse L, Boor P, Sheldon S, Zee P, et al. Sleep disturbance in children with moderate/severe atopic dermatitis: a case-control study. J Am Acad Dermatol 2018; 78: 336–341.
- Schmitt J, Spuls PI, Thomas KS, Simpson E, Furue M, Deckert S, et al. The Harmonising Outcome Measures for Eczema (HOME) statement to assess clinical signs of atopic eczema in trials. J Allergy Clin Immunol 2014; 134: 800–807.
- Vakharia PP, Chopra R, Sacotte R, Patel N, Immaneni S, White T, et al. Severity strata for five patient-reported outcomes in adults with atopic dermatitis. Br J Dermatol 2018; 178: 925–930.
- Kunz B, Oranje AP, Labrèze L, Stalder JF, Ring J, Taïeb A. Clinical validation and guidelines for the SCORAD index: consensus report of the European Task Force on Atopic Dermatitis. Dermatology 1997; 195: 10–19.
- Stalder JF, Barbarot S, Wollenberg A, Holm EA, De Raeve L, Seidenari S, et al. Patient-Oriented SCORAD (PO-SCORAD): a new self-assessment scale in atopic dermatitis validated in Europe. Allergy 2011; 66: 1114–1121.
- Brandt EB, Sivaprasad U. Th2 cytokines and atopic dermatitis. J Clin Cell Immunol 2011; 2: 110.
- Kolb L, Ferrer-Bruker S. Atopic dermatitis. StatPearls (Internet) 2021 Available from: https://www.ncbi.nlm.nih.gov/books/NBK448071/.
- Beck LA, Thaçi D, Hamilton JD, Graham NM, Bieber T, Rocklin R, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med 2014; 371: 130–139.
- Hamilton JD, Suárez-Fariñas M, Dhingra N, Cardinale I, Li X, Kostic A, et al. Dupilumab improves the molecular signature in skin of patients with moderate-to-severe atopic dermatitis. J Allergy Clin Immunol 2014; 134: 1293–1300.
- Guttman-Yassky E, Bissonnette R, Ungar B, Suárez-Fariñas M, Ardeleanu M, Esaki H, et al. Dupilumab progressively improves systemic and cutaneous abnormalities in patients with atopic dermatitis. J Allergy Clin Immunol 2019; 143: 155–172.
- Rohner MH, Thormann K, Cazzaniga S, Yousefi S, Simon HU, Schlapbach C, et al. Dupilumab reduces inflammation and restores the skin barrier in patients with atopic dermatitis. Allergy 2021; 76: 1268–1270.
- Berdyshev E, Goleva E, Bissonnette R, Bronova I, Bronoff AS, Richers B, et al. Dupilumab treatment significantly improves skin barrier function in adult and adolescent patients with moderate to severe atopic dermatitis. J All Clin Immunol 2022; 149: AB10.
![]() , Danielle Marcoux2
, Danielle Marcoux2![]() , Jonathan I. Silverberg3
, Jonathan I. Silverberg3![]() , Valeria Aoki4
, Valeria Aoki4![]() , Eulalia Baselga5
, Eulalia Baselga5![]() , Haixin Zhang6, Noah A. Levit6
, Haixin Zhang6, Noah A. Levit6![]() , Alain Taieb7,8
, Alain Taieb7,8![]() and Ana B. Rossi9
and Ana B. Rossi9![]()