ORIGINAL REPORT
Beyond Anxiety and Depression: Loneliness and Psychiatric Disorders in Adults with Atopic Dermatitis
Junfen ZHANG1 , Laura LOMAN
, Laura LOMAN , Jantje M. OLDHOFF
, Jantje M. OLDHOFF and Marie L. A. SCHUTTELAAR
and Marie L. A. SCHUTTELAAR
Department of Dermatology, University of Groningen, University Medical Centre Groningen, The Netherlands
There is a lack of knowledge concerning loneliness and psychiatric disorders other than anxiety and depression in patients with atopic dermatitis. This cross-sectional study was conducted within the Lifelines Cohort Study, in the Netherlands, by sending an atopic dermatitis questionnaire to adult participants (n = 135,950) in 2020. Psychiatric disorders were measured with a self-reported question and validated instrument (Mini International Neuropsychiatric Interview; M.I.N.I.), and loneliness was assessed with the validated 6-item De Jong Gierveld Loneliness Scale. In total, 56,896 subjects (mean age 55.8 years, 39.7% males) were included. Atopic dermatitis showed positive associations with self-reported chronic fatigue syndrome, burnout, depression, social phobia, panic disorder, attention deficit hyperactivity disorder, and eating disorder in the participants’ lifetimes. Based on the M.I.N.I., atopic dermatitis was positively associated with panic disorder and at least 1 anxiety disorder. In addition, subjects with atopic dermatitis were more likely to experience loneliness compared with those without atopic dermatitis. These associations were observed only in the moderate-to-severe, but not mild, atopic dermatitis group. This study raises awareness that a significant proportion of adults with atopic dermatitis feel lonely and are affected by several psychiatric disorders, especially those severely affected by atopic dermatitis. Further studies are required to evaluate if interdisciplinary care, such as the collaboration between dermatologists and psychiatrists, could optimize medical care for this vulnerable patient group.
Key words: atopic dermatitis; psychiatric disorder; loneliness; disease severity; epidemiology.
SIGNIFICANCE
Atopic dermatitis is one of the most common skin diseases, affecting up to 10% of adults in developed countries. It causes substantial disease burden to its patients, including decreased quality of life and work productivity, and impaired mental health. Existing research has focused on anxiety and depression, while the results of the current study indicate a significant proportion of patients being affected by other psychiatric disorders in addition to anxiety and depression, including eating disorders and attention deficit hyperactivity disorder. In addition, patients with atopic dermatitis are more likely to experience loneliness compared with healthy persons, in particular those severely affected by atopic dermatitis.
Citation: Acta Derm Venereol 2023; 103: adv9378. DOI https://doi.org/10.2340/actadv.v103.9378.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Jun 20, 2023; Published: Aug 22, 2023
Corr: Marie L. A. Schuttelaar, Department of Dermatology, University Medical Centre Groningen, PO Box 30 001, NL-9700 RB Groningen, The Netherlands. E-mail: m.l.a.schuttelaar@umcg.nl
Competing interests and funding: MLAS is an advisor, consultant, speaker and/or investigator for AbbVie, Pfizer, LEO Pharma, Regeneron, Sanofi Genzyme, Eli Lilly and Galderma. She has received grants from Regeneron, Sanofi Genzyme, Novartis and Pfizer.
INTRODUCTION
Atopic dermatitis (AD) is a common skin disease, with a lifetime prevalence of 9.3% among adults in the Dutch general population (1). This chronic disease often has a relapsing and remitting course, causing considerable disease burden, including intense itch, sleep disturbance, impaired quality of life, work productivity, and mental health, especially among those severely affected by AD (2). These factors may interact, resulting in cumulative impairment over the life course, which may lead to irreversible consequences, such as missed opportunities (3).
Previous studies on mental health have focused on anxiety and depression in patients with AD, demonstrating an elevated proportion of patients with AD being affected by depression and anxiety, especially those with severe disease (4, 5). In a meta-analysis of 16 cross-sectional studies, adult AD was positively associated with depression, with a pooled odds ratio (OR) of 2.08 (95% confidence interval (95% CI) 1.70–2.55); this association was stronger in those with greater disease severity (4). AD-related disease burden, such as increased stress (6), decreased quality of life, and comorbid atopic conditions (e.g. asthma, allergic rhinitis, food allergy) (7–10), might, in part, explain the vulnerability of patients with AD to psychiatric disorders. On the other hand, psychiatric disorders have the potential to worsen AD severity. However, little data exist on the association between adult AD and other psychiatric disorders, and how the association with psychiatric disorders varies across the disease severity of AD.
Moreover, results from a US population-based study showed that patients with AD were likely to perceive themselves as being judged and fear negative evaluations from others, due to their appearances, such as visible red/inflamed skin and affected face, and frequent scratching behaviour (11). In addition, a substantial proportion of patients with AD reported their social life being affected by their AD (12). As a consequence, patients with AD might avoid social interactions and participation, and might isolate themselves, leading to loneliness, which is one of the main indicators of social well-being. As yet, there is a lack of knowledge concerning the association between AD and loneliness.
The aim of the current study is to determine the association of AD with several psychiatric disorders and loneliness among adults in the Dutch general population. Secondarily, this study examined how the association with psychiatric disorders and loneliness varied with disease severity of AD.
MATERIALS AND METHODS
Study design and population
This cross-sectional study was conducted within the Lifelines Cohort Study (13), a multi-disciplinary prospective population-based cohort study examining the health and health-related behaviours of 167,729 persons living in the north of the Netherlands in a unique 3-generation design. It employs a broad range of investigative procedures in assessing the biomedical, socio-demographic, behavioural, physical and psychological factors that contribute to the health and disease of the general population, with a special focus on multi-morbidity and complex genetics. Baseline assessment was conducted between 2006 and 2013. Since then follow-up visits have been scheduled every 5 years and in between follow-up visits, participants receive follow-up questionnaires. Data on AD and atopic comorbidities (i.e. asthma and/or hay fever) was obtained by sending an add-on questionnaire to all adult participants (n = 135,950) of the Lifelines Cohort Study in 2020, with a response rate of 42.4% (1). Subjects were identified with AD based on self-reported physician-diagnosed AD in lifetime, and AD severity was measured using the Patient-Oriented Eczema Measure (POEM) (14). The presence of atopic comorbidities in the participant’s lifetime was determined by a question, “Have you ever had asthma or hay fever?”. All procedures were approved by the Medical Ethics Committee of University Medical Centre Groningen, the Netherlands (reference numbers METc 2007/152 and METc 2019/571) and all subjects provided written informed consent.
Psychiatric disorder
Data on psychiatric disorders were extracted from the baseline assessment. Two definitions of psychiatric disorders were used: self-reported psychiatric disorders in lifetime and the validated Mini International Neuropsychiatric Interview (M.I.N.I.) (15).
Self-reported psychiatric disorders in lifetime. The lifetime prevalence of self-reported psychiatric disorders was assessed by asking participants if they have (ever had) each of the following psychiatric disorders or related conditions, including chronic fatigue syndrome (CFS), burnout, depression, social phobia, agoraphobia, panic disorder, (other) anxiety disorder, bipolar disorder, schizophrenia, obsessive-compulsive disorder (OCD), attention deficit hyperactivity disorder (ADHD), and eating disorders.
Mini International Neuropsychiatric Interview. The M.I.N.I. (15) is a brief, reliable and valid structured diagnostic interview for diagnosing psychiatric disorders, compatible with the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and International Statistical Classification of Diseases (ICD-10). The M.I.N.I. was performed as a face-to-face interview with a nurse practitioner at baseline assessment to measure the following psychiatric disorders: major depressive disorder (MDD), dysthymia, panic disorder, agoraphobia, social phobia, and generalized anxiety disorder (GAD). Furthermore, subjects were identified with at least 1 depression disorder(s) if they reported having MDD and/or dysthymia. Subjects were identified with at least 1 anxiety disorder(s) if they reported having at least 1 of panic disorder, agoraphobia, social phobia, and GAD.
Loneliness
The 6-item De Jong Gierveld Loneliness Scale (16), a valid and reliable instrument, was included in the follow-up questionnaire between 2016 and 2019. It was used to assess overall, emotional, and social loneliness, in which loneliness is defined as a situation that occurs from a lack of quality relationships (16). This scale consists of 6 items, as listed below, with the first 3 items addressing emotional loneliness and the last 3 addressing social loneliness. Both emotional and social loneliness score range from 0 to 3 (0–1: not lonely; 2–3: lonely), and the total loneliness score ranges from 0 to 6 (0–1: not lonely; 2–6: lonely).
- I experience an emptiness around me.
- I miss people around me.
- I often feel abandoned.
- I have enough people to fall back on in case of adversity.
- I have many people that I can fully trust.
- There are enough people that I feel closely connected to.
Statistical analysis
Variables were analysed using descriptive statistics, including mean ± standard deviation (SD) and proportions. All proportions were computed after excluding missing answers. Differences between independent groups (e.g. responders vs non-responders) were assessed using an independent Student’s t-test, a χ2 test, or a Mann–Whitney U test. Non-responders were identified if they did not respond to the add-on questionnaire on AD. Binary logistic regression analysis was performed to estimate ORs (95% CI) by comparing the odds of reporting psychiatric disorders and loneliness between the subjects with AD (mild, moderate-to-severe, and all AD) and those without AD. Potential confounders based on literature research, including age (17), sex (17), and atopic comorbidities (i.e. asthma and/or hay fever) (7, 8), were adjusted in the multivariate model. IBM SPSS Statistics for Windows, version 25.0 (SPSS Inc. Chicago, IL, USA) was used for all analyses. A p-value <0.05 was regarded as statistically significant.
RESULTS
Study population
A total of 56,896 subjects (mean age 55.8 years, 39.7% males) were included in the analysis after excluding subjects below 18 years of age at baseline due to missing data on psychiatric disorders (Table I). The prevalence and disease severity of AD have been described previously (1).
| Total n (%) N = 56, 896 | Non-AD n (%) = 51, 174 | Physician-diagnosed AD n (%) N = 5, 196 | Non-AD vs physician-diagnosed AD | ||||
| Crude model OR (95% CI) | p - value | aOR (95% CI)a | p - value | ||||
| Age, years, mean± SD | 55.8 ± 12.2 | 56.1 ± 12.1 | 52.5 ± 11.9 | 0.98 (0.97–0.98) | < 0.001 | 0.99 (0.99–0.99) | < 0.001 |
| Missing, n | 0 | 0 | 0 | ||||
| Sex | |||||||
| Male | 22,577 (39.7) | 20,956 (41.0) | 1,472 (28.3) | 1 | < 0.001 | 1 | < 0.001 |
| Female | 34,319 (60.3) | 30,218 (59.0) | 3,724 (71.7) | 1.75 (1.65–1.87) | 1.59 (1.49–1.70) | ||
| Missing, n | 0 | 0 | 0 | ||||
| Asthma and/or hay fever | 7,100 (12.6) | 4,301 (8.4) | 2,775 (53.5) | 12.55 (11.79–13.37) | < 0.001 | 11.80 (11.07–12.58) | < 0.001 |
| Missing, n | 499 | 11 | 12 | ||||
| Llifetime prevalence of self-reported psychiatric disorders or related conditions | |||||||
| Chronic fatigue syndrome | 652 (1.2) | 541 (1.1) | 97 (1.9) | 1.77 (1.42–2.20) | < 0.001 | 1.30 (1.01–1.66) | 0.04 |
| Burnout | 5,046 (9.0) | 4,427 (8.8) | 553 (10.8) | 1.25 (1.14–1.37) | < 0.001 | 1.13 (1.02–1.25) | 0.02 |
| Depression | 5,283 (9.5) | 4,567 (9.1) | 642 (12.5) | 1.43 (1.31–1.56) | < 0.001 | 1.15 (1.04–1.27) | 0.01 |
| Social phobia | 492 (0.9) | 417 (0.8) | 65 (1.3) | 1.53 (1.18–2.00) | 0.00 | 1.46 (1.09–1.96) | 0.01 |
| Agoraphobia (fear of open spaces) | 272 (0.5) | 231 (0.5) | 36 (0.7) | 1.53 (1.08–2.18) | 0.02 | 1.23 (0.83–1.83) | 0.30 |
| Panic disorder | 1,501 (2.7) | 1,255 (2.5) | 221 (4.3) | 1.76 (1.52–2.03) | < 0.001 | 1.42 (1.21–1.68) | < 0.001 |
| (other) anxiety disorder | 1,609 (2.9) | 1,386 (2.8) | 198 (3.9) | 1.42 (1.22–1.65) | < .001 | 1.15 (0.98–1.37) | 0.10 |
| Manic-depressive disorder (bipolar disorder) | 169 (0.3) | 141 (0.3) | 23 (0.4) | 1.60 (1.03–2.49) | 0.04 | 1.42 (0.87–2.33) | 0.16 |
| Schizophrenia | 30 (0.1) | 26 (0.1) | < 10 (<0.2)b | 1.13 (0.34–3.74) | 0.84 | 1.53 (0.42–5.51) | 0.52 |
| Obsessive compulsive disorder | 167 (0.3) | 145 (0.3) | 21 (0.4) | 1.42 (0.90–2.25) | 0.13 | 1.33 (0.80–2.22) | 0.27 |
| ADHD | 364 (0.7) | 301 (0.6) | 60 (1.2) | 1.96 (1.49–2.60) | < 0.001 | 1.46 (1.06–2.00) | 0.02 |
| Eating disorder | 796 (1.4) | 657 (1.3) | 123 (2.4) | 1.86 (1.53–2.25) | < 0.001 | 1.35 (1.08–1.68) | 0.01 |
| Missing, n | 1,003 | 928 | 67 | ||||
| Point prevalence of psychiatric disorders based on the M.I.N.I. | |||||||
| Major depressive disorder | 872 (1.6) | 762 (1.5) | 97 (1.9) | 1.25 (1.01–1.55) | 0.04 | 0.97 (0.77–1.23) | 0.83 |
| Missing, n | 1,582 | 1,464 | 106 | ||||
| Dysthymia | 526 (1.0) | 460 (0.9) | 59 (1.2) | 1.26 (0.96–1.65) | 0.10 | 1.01 (0.75–1.36) | 0.96 |
| Missing, n | 2,619 | 2,375 | 215 | ||||
| Panic disorder | 109 (0.2) | 90 (0.2) | 18 (0.4) | 1.96 (1.18–3.25) | 0.01 | 1.85 (1.05–3.26) | 0.03 |
| Missing, n | 1,582 | 1,464 | 106 | ||||
| Agoraphobia | 1,985 (3.6) | 1,725 (3.5) | 225 (4.4) | 1.29 (1.12–1.48) | 0.00 | 1.12 (0.96–1.31) | 0.16 |
| Missing, n | 1,582 | 1,464 | 106 | ||||
| Social phobia | 404 (0.7) | 344 (0.7) | 53 (1.0) | 1.51 (1.13–2.02) | 0.01 | 1.22 (0.88–1.69) | 0.23 |
| Missing, n | 1,583 | 1,464 | 107 | ||||
| Generalized anxiety disorder | 1,901 (3.4) | 1,640 (3.3) | 230 (4.5) | 1.39 (1.21–1.60) | < 0.001 | 1.13 (0.97–1.32) | 0.12 |
| Missing, n | 1,582 | 1,464 | 106 | ||||
| At least 1 depression disorder(s) | 1,398 (2.5) | 1,222 (2.5) | 156 (3.1) | 1.25 (1.06–1.49) | 0.01 | 0.99 (0.82–1.19) | 0.88 |
| Missing, n | 1,747 | 1,613 | 118 | ||||
| At least 1 anxiety disorder(s) | 3,771 (6.8) | 3,275 (6.6) | 435 (8.5) | 1.33 (1.19–1.47) | < 0.001 | 1.13 (1.00–1.26) | 0.05 |
| Missing, n | 1,583 | 1,464 | 107 | ||||
| At least 1 depression or anxiety disorder(s) | 4,385 (7.9) | 3,817 (7.7) | 499 (9.8) | 1.31 (1.19–1.44) | < 0.001 | 1.10 (0.98–1.22) | 0.10 |
| Missing, n | 1,693 | 1,562 | 116 | ||||
| Loneliness | |||||||
| Overall loneliness (6-item) | |||||||
| Not lonely (0–1) | 28,674 (73.1) | 26,117 (73.4) | 2,340 (70.0) | 1 | 1 | ||
| Lonely (2–6) | 10,576 (26.9) | 9,473 (26.6) | 1,004 (30.0) | 1.18 (1.10–1.28) | < 0.001 | 1.14 (1.04–1.24) | 0.00 |
| Missing, n | 17,646 | 15,584 | 1,852 | ||||
| Emotional loneliness subscale (3-item) | |||||||
| Not lonely (0–1) | 34,658 (88.4) | 31,514 (88.6) | 2,874 (86.0) | 1 | 1 | ||
| Lonely (2–3) | 4,550 (11.6) | 4,037 (11.4) | 468 (14.0) | 1.27 (1.15–1.41) | < 0.001 | 1.10 (.98–1.23) | 0.11 |
| Missing, n | 17,688 | 15,623 | 1,854 | ||||
| Social loneliness subscale (3-item) | |||||||
| Not lonely (0–1) | 31,671 (80.8) | 28,790 (81.0) | 2,635 (78.9) | 1 | 1 | ||
| Lonely (2–3) | 7,544 (19.2) | 6,769 (19.0) | 706 (21.1) | 1.14 (1.04–1.24) | 0.00 | 1.15 (1.05–1.27) | 0.00 |
| Missing, n | 17,681 | 15,615 | 1,855 | ||||
| All characteristics are self-reported. | |||||||
| aAdjusted for age, sex, asthma and/or hay fever. bn < 10 was displayed to prevent traceability to participants if a group size was smaller than 10. | |||||||
| SD: standard deviation; AD: atopic dermatitis; ADHD: attention deficit hyperactivity disorder; OR: odds ratio; 95% CI: 95% confidence interval; aOR: adjusted odds ratio; M.I.N.I., Mini International Neuropsychiatric Interview. Significant p-values (< 0.05) are in bold. | |||||||
Non-responders were younger, and more often males than responders. They generally reported having psychiatric disorders and loneliness more frequently than responders (Table SI).
Atopic dermatitis in lifetime in relation to psychiatric disorders
In terms of self-reported psychiatric disorders over a lifetime, subjects with AD compared with those without had higher odds of reporting CFS (adjusted OR (aOR), 1.30; 95% CI 1.01–1.66), burnout (aOR 1.13; 95% CI 1.02–1.25), depression (aOR 1.15; 95% CI 1.04–1.27), social phobia (aOR 1.46; 95% CI 1.09–1.96), panic disorder (aOR 1.42; 95% CI 1.21–1.68), ADHD (aOR 1.46; 95% CI 1.06–2.00), and eating disorder (aOR 1.35; 95% CI 1.08–1.68) (Table I).
Based on the M.I.N.I., AD was positively associated with greater odds of reporting panic disorder (aOR 1.85; 95% CI 1.05–3.26) and at least 1 anxiety disorder(s) (aOR 1.13; 95% CI 1.00–1.26) after adjusting for age, sex and atopic comorbidities (Table I).
Atopic dermatitis in lifetime in relation to loneliness
AD showed positive associations with higher odds of reporting overall loneliness (aOR 1.14; 95% CI 1.04–1.24) and social loneliness (aOR 1.15; 95% CI 1.05–1.27) after adjusting for age, sex, and atopic comorbidities (Table I).
Disease severity of atopic dermatitis in relation to psychiatric disorders and loneliness
Subjects with moderate-to-severe AD based on the POEM, generally had the highest prevalence of psychiatric disorders and loneliness, followed by those with mild AD, and subjects without AD had the lowest prevalence of psychiatric disorders and loneliness (Fig. 1).
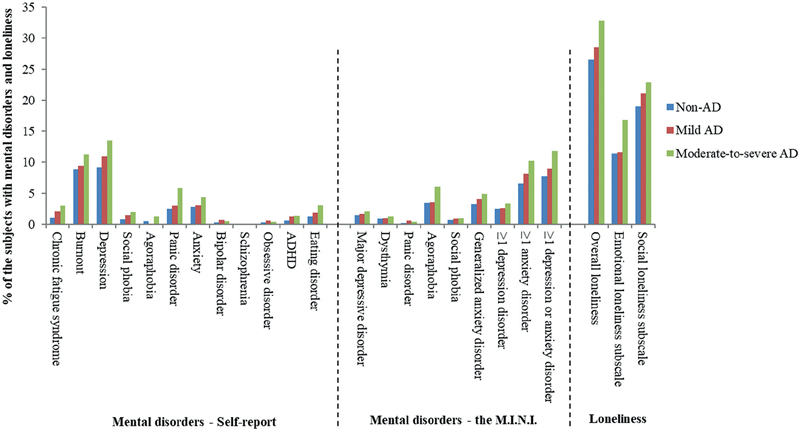
Fig. 1. Proportion of subjects with psychiatric disorders and loneliness among the non-, mild, and moderate-to-severe atopic dermatitis (AD) group. M.I.N.I.: Mini International Neuropsychiatric Interview; ADHD: attention deficit hyperactivity disorder.
In general, the odds of reporting psychiatric disorders and loneliness increased with increasing disease severity of AD (Fig. 2). Subjects with moderate-to-severe AD compared with those without, had greater odds of reporting CFS (aOR 2.10; 95% CI 1.46–3.01) depression (aOR 1.25; 95% CI 1.05–1.48), social phobia (aOR 2.17; 95% CI 1.40–3.36), agoraphobia (aOR 2.17; 95% CI 1.25–3.78), panic disorder (aOR 1.97; 95% CI 1.52–2.55) and eating disorder (aOR 1.70; 95% CI 1.20–2.43) in lifetime after adjusting for age, sex, and atopic comorbidities. In addition, moderate-to-severe AD showed positive associations with greater odds of reporting agoraphobia (aOR 1.65; 95% CI 1.28–2.11), at least 1 anxiety disorder(s) (aOR 1.36; 95% CI 1.12–1.65) and at least 1 anxiety or depression disorder(s) (aOR 1.33; 95% CI 1.11–1.60) based on the M.I.N.I. Moreover, the multivariate analysis showed positive associations of moderate-to-severe AD with overall loneliness (aOR 1.26; 95% CI 1.07–1.47), as well as emotional (aOR 1.31; 95% CI 1.08–1.60) and social loneliness (aOR 1.25; 95% CI 1.05–1.49). These observed associations were not found in the mild AD group (Fig. 2; Table SII).
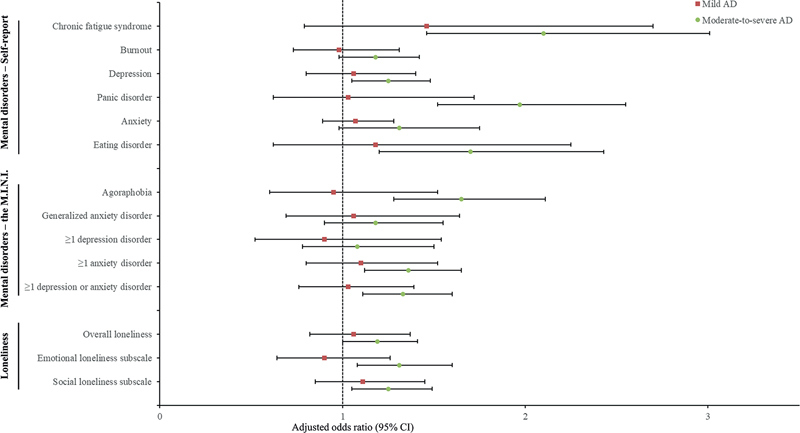
Fig. 2. Adjusted* (odds ratios) ORs for psychiatric disorders and loneliness stratified by severity of atopic dermatitis (AD) among those with vs without AD. *Adjusted for age, sex, asthma and/or hay fever. ADHD: attention deficit hyperactivity disorder; 95% CI: 95% confidence interval; M.I.N.I.: Mini International Neuropsychiatric Interview.
DISCUSSION
The current study found that adult AD showed positive associations with self-reported CFS, burnout, depression, social phobia, panic disorder, ADHD, and eating disorder in lifetime. According to the M.I.N.I., AD was positively associated with panic disorder and at least 1 anxiety disorder(s). In addition, subjects with AD were more likely to experience loneliness compared with those without AD, especially social loneliness. Furthermore, the odds of reporting psychiatric disorders and loneliness increased with increasing disease severity of AD. There were positive associations of moderate-to-severe AD with several psychiatric disorders and loneliness, while there was no association with any psychiatric disorders and loneliness among those with mild AD.
This study has confirmed previous studies that found associations between adult AD and a greater prevalence of anxiety and depression (4, 18). In the current study a distinction was made between social phobia, agora-phobia, panic disorder, and GAD in respect of anxiety disorders. However, very few studies exist on the association of adult AD with other psychiatric disorders. Results from a US population-based study (19) showed that adult AD was positively associated with ADHD (aOR 1.61; 95% CI 1.25–2.06), and several factors were found to increase the odds of reporting ADHD in adults with AD, including asthma, insomnia, and headaches. Regardless of different study populations and definitions of AD and ADHD, our point estimate (aOR 1.46) is within the confidence limits of this US study. A Finnish nationwide registry study reported positive associations of adult AD with schizophrenia and bipolar disorders (20). Based on insurance-covered health data, a regional German study showed that adult AD was positively associated with affective, stress-related, behaviour, and schizophrenic disorder (21). Due to a low prevalence of bipolar disorder, schizophrenia, and OCD in the current study population, we cannot draw a conclusion regarding these psychiatric disorders. It is worth noting that there are no previous data on CFS, burnout, and eating disorder in adults with AD. The current study found that adults with AD reported ever having CFS, burnout, and eating disorder more often than those without AD.
As yet, studies on loneliness have not been conducted in adults with AD. The current study showed a positive association between adult AD and loneliness, in particular social loneliness. Previous studies have shown that patients with AD were likely to perceive themselves as socially isolated due to lifestyle limitations, missed days in school and work, and decreased social participation caused by their disease (11, 12, 22). Also, patients with AD compared with those without, reported feeling stigmatized owing to their disease more frequently (12). The most commonly reported indicators of stigma included feeling awkward to be touched or seen by others, being bullied or teased, being stared at by other people, finding it difficult to find a romantic partner, and impaired social life due to their AD (12).
Furthermore, the current study included an assessment of AD severity based on the POEM and of its impacts on psychiatric disorders and loneliness. The results showed positive associations with several psychiatric disorders and loneliness among adults with moderate-to-severe AD, while there was no association with any psychiatric disorders and loneliness among those with mild AD. These findings are in line with previous results (5, 21, 23), despite heterogeneity in study methodology, study population, and severity assessment. Based on data from the 2015 Korean National Health Insurance Research Database, moderate-to-severe AD, but not mild AD, was positively associated with depression and anxiety in adults, in which disease severity was based on prescriptions for AD (23). Similar results were reported in a large population-based study from the UK (5). The authors used a validated algorithm to identify patients with AD and prescriptions to measure AD severity (5). In a case-control study from Germany, the frequency of physician visits due to AD was used as a surrogate measure of AD severity (21). The authors found that the likelihood of being affected by affective, stress-related, and schizophrenic disorder among adults with AD increased with increasing AD severity (21). The correlation of disease severity with psychiatric disorders and loneliness among adults with AD is bidirectional. Those severely affected are more predisposed to develop psychiatric disorders and loneliness due to greater disease burden. In addition, the presence of psychiatric disorders and loneliness are likely to impair patients’ (self)management skills for taking care of their disease, leading to an exacerbation of AD.
There are several mechanisms underlying the association of adult AD with psychiatric disorders and loneliness. Patients with AD often experience stress (6), which could affect various pathophysiological processes related to psychiatric disorders and loneliness, such as the dysregulation of the hypothalamic-pituitary-adrenal (HAP) axis (24, 25). This could alter neurotransmitter and neuroendocrine systems, which have been considered as a risk factor for some psychiatric disorders (e.g. depression and ADHD) and loneliness (24, 26). Asthma and allergic rhinitis, common comorbidities related to AD, have been associated with psychiatric disorders and loneliness (7–10). For instance, asthma, and allergic rhinitis could trigger panic attacks in patients due to their fear of dyspnoea (10). While the observed associations remained significant even after adjusting for atopic comorbidities (i.e. asthma and/or hay fever) in the current results. Moreover, adults with AD might perceive stigma as a result of their AD, leading to their avoidance of social interactions and participation, and even the occurrence of social phobia (11, 12). This could also consequently result in an inadmissible lack of quality relationships, from which loneliness stems. In addition, AD-related sleep disturbance, fatigue (22), and changes in lifestyle (e.g. greater likelihood of being obese) (6) might contribute to the occurrence of CFS, burnout, and eating disorders.
These findings underscore the necessity for more psychological support for patients with moderate-to-severe AD. Treatment guidelines have suggested psychotherapy or counselling in selected cases and to provide education to patients with AD on how to manage disease-related stress (31). Incorporating psychological interventions into management strategies has been shown to be helpful in reducing disease severity, itch intensity and scratching behaviour, while also improving QoL, sleep, and performance in patients with AD (27–30). Ultimately, this might help to prevent cumulative life course impairment. A range of psychological approaches have been utilized, including relaxation techniques, behaviour management, family constellation seminars, cognitive behavioural therapy, and habit reversal treatment. However, the existing literature on evaluations of psychological interventions remains limited, necessitating further trials verify their effects.
Study strengths and limitations
This study extends the existing literature by exploring the association of adult AD with a broad range of psychiatric disorders and loneliness, and further examining how these associations varied across AD severity, in a large sample of the Dutch general population. Several validated measures have been utilized, including the M.I.N.I., the POEM, and the 6-item loneliness scale. Definitions of psychiatric disorders were also based on self-report, which could, to some extent, reflect patients’ perception regarding their mental health. The study also has some limitations. First, definitions of AD and atopic comorbidities were based on a self-administered questionnaire, which could cause misclassification of atopic patients. Secondly, this cross-sectional study is impossible to determine the direction of the observed associations. However, the onset of AD usually occurs in early childhood (32), while psychiatric disorders and loneliness mainly develop in later life. This indicates that there is less possibility of the observed psychiatric disorders and loneliness increasing the risk for the development of AD. Meanwhile, the finding of association of greater AD severity with psychiatric disorders and loneliness could, to some extent, support the causal mechanism underlying the impact of AD on psychiatric disorders and loneliness. Thirdly, some chronic comorbidities related to AD, such as cardiovascular diseases (33), may be potential confounders for the association of AD with psychiatric disorders and loneliness, which were not adjusted in the current study model. Fourthly, due to the study design, there is a time gap between data collection on psychiatric disorders, loneliness, and AD, which could impact the power of the current results. Fifthly, non-responder bias might affect the generalizability of the current results. In addition, a correction for multiple testing was not applied, although the p-values of most found significant associations were much smaller than 0.05.
Conclusion
This study reported a positive association of adult AD with loneliness and a broad range of psychiatric disorders and related conditions, including not only anxiety. Furthermore, the odds of reporting psychiatric disorders and loneliness increased with increasing disease severity of AD. The results of the current study highlight that a significant proportion of adults with AD are affected by several psychiatric disorders and loneliness, especially those with moderate-to-severe AD. Further studies are required to evaluate whether interdisciplinary care, such as the collaboration between dermatologists and psychiatrists, could optimize medical care for this vulnerable patient group.
ACKNOWLEDGEMENTS
This study was financially supported by Novartis, but they had no role in the design or conduct of the study, interpretation of the data, or the decision to submit the manuscript for publication. The Lifelines Biobank initiative has been made possible by subsidy from the Dutch Ministry of Health, Welfare and Sport, the Dutch Ministry of Economic Affairs, the University Medical Centre Groningen (UMCG The Netherlands), University Groningen and the Northern Provinces of the Netherlands. JZ was supported by the China Scholarship Council (CSC) (grant #201806200089).
REFERENCES
- Zhang J, Loman L, Voorberg AN, Schuttelaar MLA. Prevalence of adult atopic dermatitis in the general population, with a focus on moderate-to-severe disease: results from the Lifelines Cohort Study. J Eur Acad Dermatol Venereol 2021; 35: e787–e790.
- Simpson EL, Guttman-Yassky E, Margolis DJ, Feldman SR, Qureshi A, Hata T, et al. Association of inadequately controlled disease and disease severity with patient-reported disease burden in adults with atopic dermatitis. JAMA Dermatol 2018; 154: 903–912.
- von Stülpnagel CC, Augustin M, Düpmann L, da Silva N, Sommer R. Mapping risk factors for cumulative life course impairment in patients with chronic skin diseases – a systematic review. J Eur Acad Dermatol Venereol 2021; 35: 2166–2184.
- Patel KR, Immaneni S, Singam V, Rastogi S, Silverberg JI. Association between atopic dermatitis, depression, and suicidal ideation: a systematic review and meta-analysis. J Am Acad Dermatol 2019; 80: 402–410.
- Schonmann Y, Mansfield KE, Hayes JF, Abuabara K, Roberts A, Smeeth L, et al. Atopic eczema in adulthood and risk of depression and anxiety: a population-based cohort study. J Allergy Clin Immunol Pr 2020; 8: 248–257.
- Zhang J, Loman L, Oldhoff JM, Schuttelaar MLA. Moderate-to-severe atopic dermatitis and lifestyle factors in the Dutch general population. Clin Exp Dermatol 2022; 47: 1523–1535.
- Kim DH, Han K, Kim SW. Relationship between allergic rhinitis and mental health in the general Korean adult population. Allergy Asthma Immunol Res 2016; 8: 49–54.
- Scott KM, Von Korff M, Ormel J, Zhang M, Bruffaerts R, Alonso J, et al. Mental disorders among adults with asthma: results from the World Mental Health Survey. Gen Hosp Psychiatry 2007; 29: 123–133.
- Christiansen J, Qualter P, Friis K, Pedersen SS, Lund R, Andersen CM, et al. Associations of loneliness and social isolation with physical and mental health among adolescents and young adults. Perspect Public Health 2021; 141: 226–236.
- Hsieh M-T, Liang SH-Y, Yang Y-H, Kuo T-Y, Lin T-Y, Wang T-N, et al. Allergic rhinitis increases the risk of incident panic disorder among young individuals: a nationwide population-based cohort study in Taiwan. J Affect Disord 2019; 252: 60–67.
- Silverberg JI, Gelfand JM, Margolis DJ, Boguniewicz M, Fonacier L, Grayson MH, et al. Patient burden and quality of life in atopic dermatitis in US adults: A population-based cross-sectional study. Ann Allergy, Asthma Immunol 2018; 121: 340–347.
- Roosta N, Black DS, Peng D, Riley LW. Skin disease and stigma in emerging adulthood: impact on healthy development. J Cutan Med Surg 2010; 14: 285–290.
- Scholtens S, Smidt N, Swertz MA, Bakker SJL, Dotinga A, Vonk JM, et al. Cohort Profile: LifeLines, a three-generation cohort study and biobank. Int J Epidemiol 2015; 44: 1172–1180.
- Charman CR, Venn AJ, Ravenscroft JC, Williams HC. Translating patient-oriented eczema measure (POEM) scores into clinical practice by suggesting severity strata derived using anchor-based methods. Br J Dermatol 2013; 169: 1326–1332.
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998; 59: 22–33.
- de Jong Gierveld J, van Tilburg T. [A shortened scale for overall, emotional and social loneliness]. Tijdschr Gerontol Geriatr 2008; 39: 4–15.
- Barbarot S, Auziere S, Gadkari A, Girolomoni G, Puig L, Simpson EL, et al. Epidemiology of atopic dermatitis in adults: results from an international survey. Allergy 2018; 73: 1284–1293.
- Dalgard FJ, Gieler U, Tomas-Aragones L, Lien L, Poot F, Jemec GBE, et al. The psychological burden of skin diseases: a cross-sectional multicenter study among dermatological out-patients in 13 European countries. J Invest Dermatol 2015; 135: 984–991.
- Strom MA, Fishbein AB, Paller AS, Silverberg JI. Association between atopic dermatitis and attention deficit hyperactivity disorder in U.S. children and adults. Br J Dermatol 2016; 175: 920–929.
- Kauppi S, Jokelainen J, Timonen M, Tasanen K, Huilaja L. Adult patients with atopic eczema have a high burden of psychiatric disease: a Finnish Nationwide Registry Study. Acta Derm Venereol 2019; 99: 647–651.
- Schmitt J, Romanos M, Pfennig A, Leopold K, Meurer M. Psychiatric comorbidity in adult eczema. Br J Dermatol 2009; 161: 878–883.
- Silverberg JI, Garg NK, Paller AS, Fishbein AB, Zee PC. Sleep disturbances in adults with eczema are associated with impaired overall health: a US population-based study. J Invest Dermatol 2015; 135: 56–66.
- Ahn H-J, Shin MK, Seo J-K, Jeong SJ, Cho AR, Choi S-H, et al. Cross-sectional study of psychiatric comorbidities in patients with atopic dermatitis and nonatopic eczema, urticaria, and psoriasis. Neuropsychiatr Dis Treat 2019; 15: 1469–1478.
- Campagne DM. Stress and perceived social isolation (loneliness). Arch Gerontol Geriatr 2019; 82: 192–199.
- Leistner C, Menke A. Hypothalamic-pituitary-adrenal axis and stress. Handb Clin Neurol 2020; 175: 55–64.
- Buske-Kirschbaum A, Schmitt J, Plessow F, Romanos M, Weidinger S, Roessner V. Psychoendocrine and psychoneuroimmunological mechanisms in the comorbidity of atopic eczema and attention deficit/hyperactivity disorder. Psychoneuroendocrinology 2013; 38: 12–23.
- Chida Y, Steptoe A, Hirakawa N, Sudo N, Kubo C. The effects of psychological intervention on atopic dermatitis. A systematic review and meta-analysis. Int Arch Allergy Immunol 2007; 144: 1–9.
- Norén P, Hagströmer L, Alimohammadi M, Melin L. The positive effects of habit reversal treatment of scratching in children with atopic dermatitis: a randomized controlled study. Br J Dermatol 2018; 178: 665–673.
- Revankar RR, Revankar NR, Balogh EA, Patel HA, Kaplan SG, Feldman SR. Cognitive behavior therapy as dermatological treatment: a narrative review. Int J Women’s Dermatology 2022; 8: e068.
- Capec S, Petrek M, Capec G, Yaremkevych R, Andrashko Y. Psychologic interventions in patients with the chronic dermatologic itch in atopic dermatitis and psoriasis: A step forward with family constellations seminars. Front Med 2022; 9: 965133.
- Wollenberg A, Kinberger M, Arents B, Aszodi N, Avila Valle G, Barbarot S, et al. European guideline (EuroGuiDerm) on atopic eczema – part II: non-systemic treatments and treatment recommendations for special AE patient populations. J Eur Acad Dermatol Venereol 2022; 36: 1904–1926.
- Langan SM, Irvine AD, Weidinger S. Atopic dermatitis. Lancet 2020; 396: 345–360.
- Silverberg JI, Gelfand JM, Margolis DJ, Boguniewicz M, Fonacier L, Grayson MH, et al. Association of atopic dermatitis with allergic, autoimmune, and cardiovascular comorbidities in US adults. Ann Allergy Asthma Immunol 2018; 121: 604–612.e3