QUIZ SECTION
Brownish Finger-like Patches on the Flanks: A Quiz
Ilaria TRAVE1, Andrea MURACCHIOLI1, Emanuele COZZANI1*, Antonio GUADAGNO2 and Aurora PARODI1
1Section of Dermatology – Department of Health Sciences, University of Genoa and 2Unit of Pathology, IRCCS – Ospedale Policlinico San Martino, Genoa, Italy. *E-mail: emanuele.cozzani@unige.it
Citation: Acta Derm Venereol 2023; 103: adv9428. DOI: https://doi.org/10.2340/actadv.v103.9428.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Apr 27, 2023
A 50-year-old man presented with a 20-year history of asymptomatic plaques on his trunk and limbs (Fig. 1A). The plaques had gradually increased in size and number and occurred on varying sites. No medical triggers and disorders were found except for mild hypertension and localized vitiligo. Physical examination revealed well-demarcated, yellowish-pink, linear plaques characterized by fine desquamation. The lesions were 2–5 cm in width and arranged in streaks along the axis of the ribs on the trunk. No lesions were present on other parts of the body. No lymphadenomegalies were observed. The patient denied systemic symptoms, such as fever, asthenia or weight loss. Skin biopsy was performed for pathology examination (Fig. 1B)
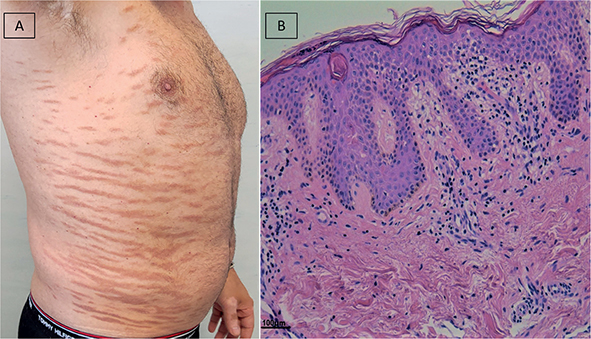
Fig. 1. (A) Lesions arranged in streaks along the axis of the ribs on the trunk. Patient consent to publish photographs was obtained. (B) Haematoxylin and eosin, original magnification 20×: the skin shows a slightly hyperplastic epidermis with mild and focal spongiosis. In the superficial dermis a perivascular dermis a perivascular lymphocytic infiltrate is observed with minimal intraepidermal lymphocytic exocytosis. Scale bar: 100 μm.
What is your diagnosis? See next page for answer
ANSWERS TO QUIZ
Brownish Finger-like Patches on the Flanks: A Commentary
Diagnosis: Digitate dermatosis
Pathological examination revealed hyperkeratosis with multiple foci of parakeratosis, irregular acanthosis and mild spongiosis of epidermidis with focal degeneration of basal keratinocytes. In the dermis, a lymphohistiocytic infiltrate with superficial interstitial and perivascular distribution was present. Minimal foci of lymphocyte intraepithelial exocytosis with minimal cytological atypia were also observed. The immunophenotypic study revealed the presence of T cell infiltrate (CD3+) with a prevalent co-expression of the CD4 molecule vs CD8 molecule. Molecular biological examination revealed the presence of T lymphocyte oligoclonality. Since the patient was asymptomatic, no specific therapies were prescribed, but follow-up was performed every 6 months.
Digitate dermatosis (DD) is a variant of small-plaque parapsoriasis, originally reported by Hu & Winkelmann in 1973 (1). The relationship between small-plaque parapsoriasis and cutaneous lymphoma is controversial, with no or minimal risk of malignant transformation and with specific featuring that support a risk of progression (2). Clues that differentiate parapsoriasis from mycosis fungoides are: chronicity (parapsoriasis manifests as chronic), symptoms (small-plaque parapsoriasis is most frequently asymptomatic) and clinical featuring (small-plaque parapsoriasis presents recalcitrant patches or thin plaques). On histopathology, epidermotropism (Pautrier’s microabscesses) and lymphocytic atypia are distinctive characteristics of mycosis fungoides, even though they can also be less pronounced in parapsoriasis. In addition, immunohistochemistry with elevated CD4:CD8 ratio (> 6), loss of common T-cell markers (3) and the detection of identical clones from 2 different skin sites (4) may be helpful in confirming a diagnosis of mycosis fungoides.
The oligoclonal pattern on molecular genetic study is an uncommon pattern, which is present in 11% of small-plaque parapsoriasis cases in the literature (5), and in both small-plaque parapsoriasis and mycosis fungoides without a referred higher risk of evolution for the former (5).
To conclude, digitate dermatosis is a rare and distinctive variant of small-plaque parapsoriasis which it is important to recognize. Although a risk of 10% rate of progression (6) is reported only for small-plaque parapsoriasis and its variants, it is important that all patients undergo regular long-term follow-up examination every 3-6 months for 1 year and subsequently, every year to exclude the development of mycosis fungoides or other lymphoma. A rebiopsy of skin lesions is also recommended in suspicious cases. Finally, the finding of an oligoclonality in small patch parapsoriasis does not seem to require closer follow-up. Various therapeutic approaches have been reported in the literature, including topical therapies (e.g. corticosteroids, bexarotene, nitrogen mustard, carmustine), laser and light-based therapy, such as narrowband UVB, and psoralen ultraviolet A (2).
REFERENCES
- Hu CH, Winkelmann RK. Digitate dermatosis. A new look at symmetrical, small plaque parapsoriasis. Arch Dermatol 1973; 107: 65–69.
- Chairatchaneeboon M, Thanomkitti K, Kim EJ. Parapsoriasis – a diagnosis with an identity crisis: a narrative review. Dermatol Ther (Heidelb) 2022; 12: 1091–1102.
- Sarveswari KN, Yesudian P. The conundrum of parapsoriasis versus patch stage of mycosis fungoides. Indian J Dermatol Venereol Leprol 2009; 75: 229–235.
- Kikuchi A, Naka W, Harada T, Sakuraoka K, Harada R, Nishikawa T. Parapsoriasis en plaques: its potential for progression to malignant lymphoma. J Am Acad Dermatol 1993; 29: 419–422.
- Belousova IE, Vanecek T, Samtsov AV, Michal M, Kazakov DV. A patient with clinicopathologic features of small plaque parapsoriasis presenting later with plaque-stage mycosis fungoides: report of a case and comparative retrospective study of 27 cases of “nonprogressive” small plaque parapsoriasis. J Am Acad Dermatol 2008; 59: 474–482.
- Calonje E, Lazar A, Brenn T, McKee PH. McKee’s pathology of the skin with clinical correlations. 4th edn. Saint Louis, MO: Elsevier Saunders; 2012.