QUIZ SECTION
Necrotic Lip Infection Complicated by Facial Cellulitis and Septic Thoracic Emboli in an 18-year-old Man: A Quiz
Olivier SARAUX1, Françoise FABRE2, Brigitte MILPIED1, Charles CAZANAVE3 and Marie BEYLOT-BARRY1*
1Dermatology Department, Bordeaux University Hospital, Bordeaux, 2Private office, Saint-Médard-en-Jalles and 3Infectious and Tropical Diseases Department, Bordeaux University Hospital, Bordeaux, France. *E-mail: marie.beylot-barry@chu-bordeaux.fr
Citation: Acta Derm Venereol 2023; 103: adv9605. DOI https://doi.org/10.2340/actadv.v103.9605.
Copyright: © Published by Medical Journals Sweden, on behalf of the Society for Publication of Acta Dermato-Venereologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Published: Sep 20, 2023
An 18-year-old man with no comorbidity developed cheilitis of the lower lip (Fig 1a). He took non-steroidal anti-inflammatory drugs (NSAID) in self-medication (ibuprofen, 400 mg). Two days later, the swelling of the lip had worsened (Fig. 1b) and he was prescribed oral valaciclovir (500 mg twice a day) and oral fusidic acid (500 mg twice a day). The cheilitis became highly inflammatory and associated with fever and the patient was admitted to the Dermatology Department, University hospital of Bordeaux 2 days later (Fig. 1c). Oral amoxicillin/clavulanic acid (AMC): 1g/125mg, 3 times a day, was started, but 36 h later his lip became necrotic, associated with facial cellulitis (Fig. 1d), with dyspnoea and thoracic pain. Computed tomography revealed cervico-facial cellulitis (Fig. 1e) and multiple thoracic septic emboli (Fig. 1f).
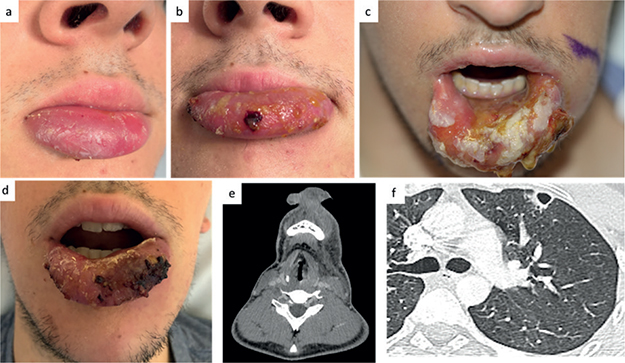
Fig. 1. Initial presentation and progression with necrotic cheilitis and cellulitis. (a) Initial presentation of cheilitis. (b) Worsening of the cheilitis 2 days later. (c) Highly inflammatory and ulcerative macrocheilitis. (d) Necrotic macrocheilitis with cellulitis. (e) Computed tomography (CT) scan: facial cellulitis. (f) CT scan: pulmonary emboli.
What is your diagnosis? See next page for answer.
ANSWERS TO QUIZ
Necrotic Lip Infection Complicated by Facial Cellulitis and Septic Thoracic Emboli in an 18-year-old Man: A Commentary
Diagnosis: Panton-Valentin leukocidin-positive Staphylococcus aureus cheilitis complicated by septic thoracic embolisms
Skin swab and blood cultures both isolated a methicillin-susceptible Staphylococcus aureus (MSSA) strain with fusidic acid resistance. Specific PCR detected Panton-Valentin leucocidin (PVL) gene. The patient received intravenous infusions of AMC plus linezolid (for an anti-toxinic activity) for 6 days followed by oral treatment with intravenous AMC, 6 g a day, plus intravenous linezolid 600 mg twice a day followed by oral AMC 6 g a day for 5 days and oral linozolid 600 mg twice a day. Rapid complete resolution of the symptoms occurred (Fig. 2). Investigations for cellular and humoral immunity, including human immunodeficiency virus infection did not reveal any abnormalities. Sites decolonization of the index case and family contacts (without sampling of the family) was performed for 7 days with chlorhexidin foaming solution 4%, once a day for 7 days. Mupirocin topical ointment 2%, in nose and ears, 3 times a day for 7 days. Seven months later, the patient presented an eyelid abscess due to PVL+MSSA, which was treated with oral AMC: 1 g/125 mg, 3 times a day, for 7 days. Ten days after completion of the course of antibiotics, sampling of colonization sites of the patient revealed, only for the nasal swab, a PVL+MSSA that was fusidic acid resistant. Decontamination was repeated for 10 days: for the patient, Mupirocin topical ointment 2%, in nose and ears, betadine (povidone-iodine) 10% mouthwash, both 3 times a day, for 7 days, and showers with chlorhexidine; for the family members: mupirocin cream and chlorhexidine showers only. However, antibiogram on the strain from the nasal site revealed a resistance to mupirocin. Before we proposed a further decontamination, the patient presented again with an eyelid infection, which was treated with oral AMC: 1 g/125 mg, 3 times a day, for 7 days. New samples of colonization sites for the patient and his family remained negative. No infectious recurrence was observed after 12-month follow-up.
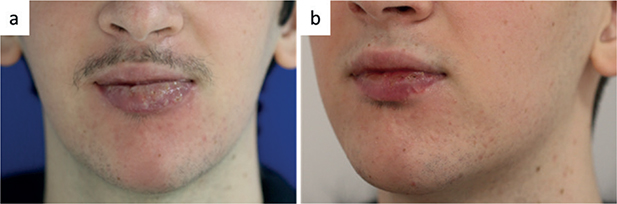
Fig. 2. Favourable outcome and complete resolution. (a) Outcome after 5 days of intravenous antibiotics; (b) complete resolution after 1 month.
This case is informative on several points. First, it underlines the likely role of NSAIDs, used here as self-medication, in the worsening of the skin infection with systemic involvement diffusion. Indeed, exposure to NSAIDs has been shown to be associated with high risk of invasive bacterial infections, such as necrotizing soft-tissue infection, due both to impairment of host neutrophils defences, and possible alteration of antibiotic efficacy, enhancing local dissemination of the infection. Moreover, NSAID use may mask clinical signs and delay appropriate diagnosis and management (1, 2). Secondly, this impressive clinical presentation should suggest PVL+ S. aureus. These skin and soft tissue infections may have critical outcome, with life-threatening systemic localizations, such as pneumonia or meningitis (3). Moreover, the current case as well as the case reported by Chaya et al. (4), illustrated the severity of infection due to PVL+ S. aureus even in a young patient with no comorbidity or immunodeficiency. PVL is a bicomponent, pore-forming toxin produced by several strains of S. aureus, not necessarily methicillin-resistant. PVL is a predictive marker for the severity of bone and joint infections, deep abscesses and complicated skin and soft-tissue infections (5). The choice of antibiotics to treat staphylococcal infection is determined by the methicillin-susceptibility but also by the PVL+ character. In severe PVL+ MSSA infection, as in the current case, first-line treatment is AMC (or intravenous oxacillin 1–2 g every 4 h and oral or intra venous linezolid 600 mg twice a day (5). Lastly, antimicrobial resistance is a current concern, as it leads to multiple recurrences. Although mupirocin is the first-line antibiotic for staphylococcal decontamination, resistance is increasingly described, hence this precious antibiotic must be used with caution (6).
REFERENCES
- Souyri C, Olivier P, Grolleau S, Lapeyre-Mestre M, French Network of Pharmacovigilance Centres. Severe necrotizing soft-tissue infections and nonsteroidal anti-inflammatory drugs. Clin Exp Dermatol 2008; 33: 249–255.
- Hua C, Urbina T, Bosc R, Parks T, Sriskandan S, de Prost N, et al. Necrotising soft-tissue infections Lancet Infect Dis 2023; 23: e81–94.
- Salliot C, Zeller V, Puechal W, Manceron V, Sire S, Varache N, et al. Panton-valentine leukocidin-producing Staphylococcus aureus infections: report of 4 French cases. Scand J Infect Dis 2006; 38: 192–195.
- Chaya A, Sato M, Namkoon H, Wada N. Panton-valentine leukocidin-positive methicillin-resistant Staphylococcus aureus infection of the lip. Int J Infect Dis 2018; 75: 80–81.
- Gillet Y, Dumitrescu O, Tristan A, Dauwalder O, Javouhey E, Floret D. Pragmatic management of panton-valentine leukocidin-associated staphylococcal diseases. Int J Antimicrob Agents 2011; 38: 457–464.
- Dadashi M, Hajikhani, Darban-Sarokhalil D, Belkum A, Goudarzi M. Mupirocin resistance in staphylococcus aureus: a systematic review and meta-analysis. J Glob Antimicrob Resist 2020; 20: 238–247.