RESEARCH ARTICLE
Radiological features and treatment of erupting maxillary canines in relation to the occurrence of dental developmental abnormalities
Jenni Ristaniemia*, Terhi Karjalainena, Kati Kujasaloa, Wille Rajalaa, Paula Pesonenb and Raija Lähdesmäkia,c
aOral Development and Orthodontics, Research Unit of Population Health, Faculty of Medicine, University of Oulu, Oulu, Finland; bInfrastructure for Population Studies, Faculty of Medicine, University of Oulu, Oulu, Finland; cOral and Maxillofacial Department, Medical Research Center Oulu (MRC Oulu), Oulu University Hospital, Oulu, Finland
ABSTRACT
Objective: This study aimed to investigate the radiological features of the permanent canines and the treatment carried out to ensure their eruption relative to certain features involved in Dental Anomaly Patterns (DAP).
Material and Methods: The cross-sectional part of this retrospective register-based study focused on 1,315 dental panoramic tomographs (DPTs) of children aged 8.5–10.5 years, while the longitudinal part involved information on the treatment provided for 1,269 canines after the DPTs and on their eruption into the oral cavity.
Results: The canines of the DAP children more often showed evidence of early treatment (p = 0.014), with girls having more frequently interceptive treatment (p = 0.004) and boys early headgear (p = 0.022). Delayed dental age was associated with early treatment (OR 3.29, 95% CI 1.08–9.99). Either no or clear overlapping of a canine with the lateral incisor occurred more often in the DAP children, whereas canine inclination did not differ between the groups. The root development stage of the canine was more often either beginning or well advanced in the DAP children.
Conclusions: The children with dental developmental abnormalities more often showed evidence of early treatment for the canines. Monitoring of the erupting canines after the first mixed stage is important to enable timely early treatment.
KEYWORDS: Abnormal eruption; developing dentition; diagnostics; human; mixed dentition
Citation: ACTA ODONTOLOGICA SCANDINAVICA 2024; VOL. 83: 197–203. DOI: https://doi.org/10.2340/aos.v83.40488.
Copyright: © 2024 The Author(s). Published by MJS Publishing on behalf of Acta Odontologica Scandinavica Society. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 22 August 2023; Accepted: 19 December 2024; Published: 25 April 2024.
CONTACT Jenni Ristaniemi jenni.ristaniemi@oulu.fi Oral Development and Orthodontics, Research Unit of Population Health, Faculty of Medicine, University of Oulu, Oulu, Finland
Competing interests and funding: The authors report that there are no competing interests to declare.
This study was supported by grants from the Finnish Dental Society Apollonia, the Päivikki and Sakari Sohlberg Foundation, and the University of Oulu Scholarship Foundation (to JR).
Introduction
The development of the human dentition involves a number of abnormalities leading to clinical problems. One of the most problematic conditions is eruption disturbance in a maxillary permanent canine, since the eruption route is long and complex [1,2] and the eruption process shows many kinds of abnormalities [3]. Normally the maxillary canines erupt into the oral cavity at an age of 10–12 years, during the late stage of the mixed dentition, but with a normal deviation of several years [4].
Overlapping with the lateral incisor root and a larger mesial inclination angle of the maxillary canine are elements in the earlier stages of the eruption and development of the canines and both should be reduced if eruption is to proceed normally [5–7], whereas in an abnormal eruption path both will still be pronounced [6, 8, 9]. Root development does not differ between normally and abnormally erupting maxillary canines [6, 9].
Early diagnosis of eruption disturbances in the maxillary canines in relation to the stage in dental development is crucial so that early interceptive treatment can be performed effectively and in time. Extraction of a primary maxillary canine [10–13] and the use of headgear in the early mixed dentition [14, 15] are effective treatment options for managing eruption disturbances in the permanent canines.
Certain dental developmental abnormalities have been reported to occur together more often than can be explained by chance alone [16–22]. It was Peck who first described the concept of Dental Anomaly Patterns (DAP) [17, 23–30]. Many of these conditions can be diagnosed during the early stages of the mixed dentition, providing an opportunity to monitor features of DAP that may possibly occur later. Eruption disturbances in the maxillary canines have been linked to DAP, as palatally displaced maxillary canines, for example, have been stated to be one DAP feature [17, 24].
Dental panoramic tomograph (DPT) is a basic examination for assessing the developing dentition and observing the eruption of the permanent maxillary canines. The aim of the present study was to investigate the radiological features of the erupting canines a couple of years before eruption into the oral cavity and the treatment provided for the canines in relation to the dental developmental abnormalities involved in DAP as seen in a DPT. Our hypotheses were that children with the dental developmental abnormalities studied here have pronounced overlapping of the maxillary canines with the lateral incisors and larger inclination angles in the maxillary canines, and that such children more often receive treatment for a maxillary canine.
Materials and methods
Study material
The cross-sectional part of this register-based research included 1,454 digitally copied DPTs of the developing permanent dentition from a cohort of third-year primary school children of Finnish ancestry in Eastern Finland born between 1980 and 1996. For the longitudinal part of this research, the dental records and other dental radiographs were examined in order to determine the treatment carried out for the maxillary canines. The data were gathered retrospectively from the Health Centre’s dental records with permission (2006, 2015 and 2019) from the keeper of the register. All personal information was coded to prevent identification.
DAP features
The features listed below were introduced first as DAP by Peck [17] and were looked for in the DPTs studied here. Their prevalences have been reported earlier [22].
Absent teeth
A permanent tooth was deemed congenitally absent if the follicle was not visible. Absent teeth were assessed by ER and in cases of rare absences (maxillary canines, mandibular incisors and second molars) confirmed by JR. Third molar absences were excluded.
Microform teeth (peg-shaped maxillary lateral incisors)
Peg-shaped lateral incisors were recorded when the mesiodistal width of the crown was smaller than that of the cervical part of the tooth [31], the anatomical shape of the crown was pointed in form and the root was possibly smaller [32]. Peg-shaped maxillary lateral incisors were assessed by JR, and a consensus opinion was sought by JR and RL when necessary. The one exclusion criterion was an unclear DPT. Calibration of the DPT material was performed by JR and borderline cases (n = 14) discussed with RL.
Delay in tooth formation and eruption (generalized)
Dental age was assessed in terms of the delay (≤ -1 year) relative to the chronological age. Dental age was determined by EM and JI using the seven teeth dental maturity method of Demirjian [33, 34] and assessed by reference to Finnish maturity curves [35]. The exclusion criteria were an absent tooth (no counterpart) or poor quality of the DPT. The two examiners assessed the same set of 30 DPTs twice to test the accuracy of the assessments.
Infraocclusion (of primary molars)
The primary molars were assessed relative to the occlusal plane and the marginal ridges of the adjacent teeth, and the DPTs were categorized as showing no visible infraocclusion or visible infraocclusion in at least one primary molar in the maxilla or mandible, assessed by JR and calibrated by JR and RL. The exclusion criteria were an absent primary molar and no infraocclusion in the others, failure to determine the occlusal plane, significant loss of morphology in the primary molars, an orthodontic appliance in the area or an unclear DPT. Repeatability was estimated by measuring 146 DPTs twice.
Transposition
Transpositions of a canine and first premolar in the maxilla and a canine and lateral incisor in the mandible were included. Teeth were classified as transposed if their crowns had crossed each other as seen in the DPT despite the presence of adequate space in the dental arch. This was assessed by KK and confirmed by JR.
Distal angulation of unerupted mandibular second premolars
A mandibular second premolar was classified by KK as distally displaced if the long axis of the developing premolar intersected with the mesial border of the mandibular first molar (adapted from Baccetti et al. [20]). The exclusion criteria, confirmed by JR, were an emerged mandibular second premolar, mandibular second premolar root development that had not yet started, or the absence of the mandibular first molar.
Features of maxillary canines
Overlapping and inclination
Overlapping of a maxillary canine crown with the lateral incisor root (overlapping) and inclination (α) (inclination) were measured on the DPTs by KK using the neaView Radiology software (Neagen Oy) (see Figure 1 in Ristaniemi et al. [7], modified from Ericson and Kurol [10]). Overlapping was classified as Grade 0 (no overlapping), Grade 1 (crown of the canine covering half or less of the width of the lateral incisor root) and Grade 2 (crown of the canine covering more than half of the width of the lateral incisor root). Overlapping was not determined in dentition involving an absent lateral incisor. The inclination was measured as the angle between the mid-sagittal suture of the maxilla and the mid-axis of the canine, where the latter was defined by reference to the pulp chamber. In cases of crooked roots and rotated teeth, the average tooth axis was adjusted by reference to the crown and root. The exclusion criteria were an emerged canine, complete primary or permanent dentition, orthodontic treatment at the time of the DPT or an unclear DPT. The measurements were assessed for repeatability by measuring 31 DPTs twice.
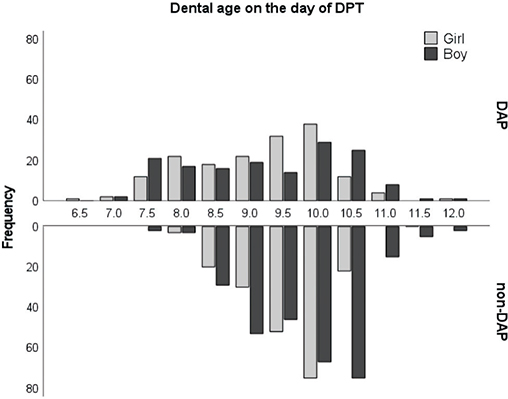
Figure 1. Distribution of DAP children (n = 392) and non-DAP children (n = 499) by dental age in years. DAP: Dental Anomaly Patterns.
Developmental stages of the maxillary canines and lateral incisors
The root development stages of the maxillary canines were assessed from the DPTs by WR following the method of Nolla [36] and scaled as Stage 1 (root formation started), Stage 2 (one-third of the root length completed), Stage 3 (half of the root length completed), Stage 4 (at least two-thirds of the root length completed) and Stage 5 (root completed, apex open/closed). The exclusion criteria were oligodontia (> six missing teeth) or an unclear DPT. Repeatability was estimated from 65 randomly selected DPTs (130 maxillary canines).
The development stages of the lateral incisors in the maxilla were assessed by WR from the DPTs and categorized as incomplete or complete (Stage 5). The exclusion criteria were a peg-shaped lateral incisor, an absent lateral incisor, oligodontia (> six missing teeth) or an unclear DPT.
Treatment
Orthodontic treatment necessitated by the eruption of a maxillary canine was carried out according to a treatment plan made by a senior orthodontist and information on this treatment was collected retrospectively by JR, KK and RL from the dental records found in the health centre’s paper archives or software after DPT and until the maxillary canine had been caused to erupt. The exclusion criteria for this variable were an emerged canine (based on DPT and/or dental records), oligodontia (> six absent teeth), poor quality of the DPT, odontoma or a cyst in the maxillary canine area or transposition of a maxillary canine and the first premolar. Orthodontic treatment carried out before DPT or after the eruption of a maxillary canine was not included. The forms of treatment were categorised as shown in Table 1.
Inclusion criteria
The inclusion criteria for this study were chronological age 8.5–10.5 years at the time of the DPT, dentition in the mixed stage and no syndromes of clefts (study material). The group of children with DAP (DAP children) included those with at least one dental developmental abnormality of the kind studied here as being involved in DAP [17] as seen in the DPT, while the group for comparison (non-DAP children) was selected from the rest of the children, who had no such dental developmental abnormalities in their DPT.
Statistics
The distributions of the variables studied here were described in terms of frequencies and percentages, and comparisons of the variables between the genders were performed using Pearson’s Chi-square test. Comparisons between the maxillary canines of the DAP and non-DAP children and between the treatment subgroups were performed with either Pearson’s Chi-square test or Fisher’s exact test. The normality of continuous variables such as angles and chronological and dental ages was assessed visually using histograms. Mean chronological and dental ages were analyzed with the independent samples t-test.
The single associations of independent DAP features and gender with the response variables (no treatment, early treatment, late treatment, all treatments) were determined with crude logistic regression models, while adjusted logistic regression models were used to check the associations of all DAP features and gender with the response variables in the study material. Statistically significant two-way interaction terms were checked during the formation of the models, the strength of each association being illustrated with an odds ratio and 95% confidence interval. The logistic regression models were resolved using the SAS glimmix procedure with random effect, to take account of children having two canines in the data.
The statistical analyses were performed using IBM SPSS Statistics (version 28.0) and SAS Enterprise guide 7.1. P-values <0.05 were considered statistically significant. Repeatability was assessed using Cohen’s kappa or intra-class correlation (ICC).
Results
Repeatability
Intra-rater repeatability was assessed for infraocclusion (k = 0.837), dental age (examiner 1 ICC = 0.789 and examiner 2 ICC = 0.945), overlapping (d.13 k = 0.917, d.23 k = 0.849), inclination (d.13 ICC = 0.933, d.23 ICC = 0.922) and MxC root development (Stages 1–5) (k = 0.777), while inter-rater reliability was assessed for dental age (ICC = 0.871). The assessments proved to be reliable in terms of their repeatability.
DAP and non-DAP children
The study material consisted of 1,315 DPTs representing 619 girls and 696 boys aged 8.5–10.5 years. The inclusion criteria for DAP children were met by 392 children (207 girls and 185 boys), their mean chronological age at the time of the DPTs being 9.4 years (SD 0.4), with no gender difference (p = 0.980). The group of non-DAP children included 499 children (202 girls and 297 boys), with a mean chronological age of 9.3 years (SD 0.3) and no difference between the genders (p = 0.070). The mean chronological age did not differ between the DAP and non-DAP children (p = 0.881).
The dental ages of the DAP children varied from 6.5 to 11.9 years, with a mean of 9.1 years (SD 1.0) in the girls and from 7.1 to 11.9 years, with a mean of 9.2 years (SD 1.1) in the boys, whereas the dental ages of the non-DAP children varied from 7.9 to 10.7 years, with a mean of 9.6 years (SD 0.6) in the girls and from 7.7 to 12.0, with a mean of 9.8 years (SD 0.8) in the boys (Figure 1).
Features of maxillary canines in the DAP and non-DAP children
The treatment provided could be assessed in the case of 1,269 canines, with no gender differences (p = 0.355). The maxillary canines of the DAP children had more often been subject to early treatment (p = 0.014) (Table 2), which was more often of an interceptive kind for the DAP girls (5.6% vs. 1.3%, p = 0.004), whereas the DAP boys more often had treatment with early headgear (5.9% vs. 2.5%, p = 0.022). Orthodontic treatment was provided more often for the non-DAP children (1.6% vs. 0.6%), but this difference was not statistically significant (p = 0.134).
| Girls | Boys | All | Pa | ||||||||||||
| DAP | non-DAP | Pa | DAP | non-DAP | Pa | DAP | non-DAP | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | ||||
| No treatment | 235 | 88.3 | 286 | 89.4 | 210 | 88.6 | 411 | 92.2 | 445 | 88.5 | 697 | 91.0 | |||
| Early treatment | 22 | 16 | 0.127b | 18 | 19 | 0.065b | 40 | 35 | 0.014b | ||||||
| Interceptive treatment | 15 | 5.6 | 4 | 1.3 | 0.004b | 4 | 1.7 | 8 | 1.8 | >0.999c | 19 | 3.8 | 12 | 1.6 | 0.012b |
| Early headgear | 7 | 2.6 | 12 | 3.8 | 0.477b | 14 | 5.9 | 11 | 2.5 | 0.022b | 21 | 4.2 | 23 | 3.0 | 0.243b |
| Late treatment | 9 | 18 | 0.230b | 9 | 16 | 0.821b | 18 | 34 | 0.529b | ||||||
| Orthodontic treatment | 2 | 0.8 | 7 | 2.2 | 0.198c | 1 | 0.4 | 5 | 1.1 | 0.669c | 3 | 0.6 | 12 | 1.6 | 0.134b |
| Treatment for crowding | 7 | 2.6 | 11 | 3.4 | 0.602b | 8 | 3.4 | 11 | 2.5 | 0.453b | 15 | 3.0 | 22 | 2.9 | 0.847b |
| DAP: Dental Anomaly Patterns. a Significances of differences between no treatment and the treatment subgroups; b Pearson’s Chi-square test; cFisher’s exact test. |
|||||||||||||||
The distributions of maxillary canine features in the DAP and non-DAP children by gender are presented in Table 3. Within the total set of canines studied (n = 1,515), overlapping occurred more often in the girls (p = 0.026). The maxillary canines of the DAP children more often not only showed clear overlapping (Grade 2) but also no overlapping occurred more often (p = 0.006). Some (Grade 1) or clear overlapping occurred more often in the maxillary canines of the non-DAP boys than in the DAP boys (p = 0.023), whereas no difference in this respect was found between the girls (p = 0.078). The mean inclination angle was 13.4° (SD 7.5), but there was no difference in grouped inclination (n = 1,539) between the genders (p = 0.051) or between the DAP and non-DAP children (p = 0.724).
| Girls | Boys | All | ||||||||||
| DAP | non-DAP | DAP | non-DAP | DAP | non-DAP | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Overlapping of caninea | ||||||||||||
| Grade 0 | 174 | 52.7 | 175 | 45.7 | 166 | 61.3 | 271 | 51.0 | 340 | 56.6 | 446 | 48.8 |
| Grade 1 | 137 | 41.5 | 191 | 49.9 | 98 | 36.2 | 243 | 45.8 | 235 | 39.1 | 434 | 47.5 |
| Grade 2 | 19 | 5.8 | 17 | 4.4 | 7 | 2.6 | 17 | 3.2 | 26 | 4.3 | 34 | 3.7 |
| P-valuec | 0.078 | 0.023 | 0.006 | |||||||||
| Inclination of canine (o) | ||||||||||||
| <15 | 198 | 58.9 | 229 | 59.5 | 168 | 60.2 | 347 | 64.4 | 336 | 59.5 | 576 | 62.3 |
| 15–19.9 | 73 | 21.7 | 81 | 21.0 | 63 | 22.6 | 107 | 19.9 | 136 | 22.1 | 188 | 20.3 |
| 20–24.9 | 34 | 10.1 | 44 | 11.4 | 35 | 12.5 | 56 | 10.4 | 69 | 11.2 | 100 | 10.8 |
| ≥25 | 31 | 9.2 | 31 | 8.1 | 13 | 4.7 | 29 | 5.4 | 44 | 7.2 | 60 | 6.5 |
| P-valuec | 0.078 | 0.548 | 0.724 | |||||||||
| Canine root developmentb | ||||||||||||
| Stage 1 | 21 | 5.1 | 4 | 1.0 | 73 | 20.9 | 67 | 11.3 | 94 | 12.3 | 71 | 7.1 |
| Stage 2 | 224 | 54.4 | 223 | 57.7 | 225 | 64.3 | 423 | 71.5 | 449 | 58.9 | 656 | 65.9 |
| Stage 3 | 112 | 27.2 | 140 | 34.7 | 40 | 11.4 | 85 | 14.4 | 152 | 19.9 | 225 | 22.6 |
| Stage 4 | 52 | 12.6 | 27 | 6.7 | 12 | 3.4 | 17 | 2.9 | 64 | 8.4 | 44 | 4.4 |
| Stage 5 | 3 | 0.7 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 3 | 0.4 | 0 | 0.0 |
| P-valuec | <0.001 | <0.001 | <0.001 | |||||||||
| Lateral incisor developmentb | ||||||||||||
| Incomplete | 324 | 80.6 | 314 | 79.7 | 320 | 92.0 | 514 | 87.7 | 644 | 85.9 | 828 | 84.5 |
| Complete | 78 | 19.4 | 80 | 20.3 | 28 | 8.0 | 72 | 12.3 | 106 | 14.1 | 152 | 15.5 |
| P-valuec | 0.750 | 0.043 | 0.426 | |||||||||
| DAP: Dental Anomaly Patterns. a Grade 0 (no overlapping), Grade 1 (≤ 1/2 overlapping) and Grade 2 (> 1/2 overlapping); b Division is based on developmental stages as defined by Nolla’s method [36]; c Pearson’s Chi-square test. |
||||||||||||
The stage of canine root development yielded Nolla’s values [36] in the range 6.0–9.0 (n = 1,758) and was significantly more advanced in the girls (p < 0.001), as was also the case with the stage of lateral incisor development (n = 1,730) (p < 0.001). The root development stage of the canines varied among the DAP and non-DAP children, with the DAP children’s canines more often in either an early (Stage 1) or later stage (Stages 4–5), whereas those of the non-DAP children were mainly at Stages 2 and 3 (p < 0.001). The stage of lateral incisor development was more often incomplete in the DAP boys (p = 0.043) but did not differ among the girls (p = 0.750).
Associations between DAP features and maxillary canine treatment
In crude logistic regression analysis of the study material, the absence of teeth (OR 2.09, 95% CI 1.01–4.35) and delayed dental age were associated with the provision of treatment (OR 2.39, 95% CI 1.04–5.49), within which delayed dental age was especially associated with early treatment (OR 3.29, 95% CI 1.08–9.99) (Table 4). The adjusted logistic regression models for the study material did not give any associations between the DAP features studied here and the treatment groups (Table 4).
| Early treatment | Late treatment | All treatments | ||||||||||
| Crude | Model | Crude | Model | Crude | Model | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Gender boy (ref. Girl) | 0.83 | 0.47–1.47 | 0.89 | 0.44–1.81 | 1.03 | 0.59–1.80 | 0.72 | 0.33–1.56 | 0.93 | 0.62–1.41 | 0.81 | 0.46–1.41 |
| Absent teeth (ref. no) | 2.57 | 0.98–6.80 | 3.49 | 0.93–13.09 | 1.52 | 0.53–4.32 | 2.25 | 0.40–12.56 | 2.09 | 1.01–4.35 | 2.93 | 0.94–9.12 |
| Peg-shaped MxI2 (ref. no)b | 4.03 | 0.68–23.75 | 2.27 | 0.29–17.54 | 0.83 | 0.07–10.28 | – | – | 2.50 | 0.61–10.20 | 1.41 | 0.21–9.53 |
| Delayed dental age (ref. normal) | 3.29 | 1.08–9.99 | 2.53 | 0.83–7.69 | 1.53 | 0.46–5.10 | 0.74 | 0.14–3.92 | 2.39 | 1.04–5.49 | 1.89 | 0.72–4.95 |
| Infraocclusion (ref. no) | 1.15 | 0.53–2.50 | 1.39 | 0.58–3.31 | 0.36 | 0.11–1.14 | 0.35 | 0.10–1.27 | 0.78 | 0.41–1.48 | 0.87 | 0.41–1.84 |
| Distal angulation of MnP2 (ref. no) | 1.09 | 0.34–3.55 | 0.62 | 0.10–3.94 | 1.04 | 0.31–3.52 | 2.10 | 0.51–8.74 | 1.07 | 0.45–2.55 | 1.21 | 0.38–3.82 |
| DAP feature (ref. no)c | 1.81 | 0.96–3.42 | 0.84 | 0.40–1.76 | 1.32 | 0.81–2.16 | ||||||
| DAP: Dental Anomaly Patterns. a Prevalences of DAP features in the study material are presented in Table 2 [22]; b Peg-shaped MxI2 was excluded from the logistic regression model for late treatment; c Transposition was excluded from the analysis and models Results are illustrated for the maxillary canines, so that the DAP feature was the same for both maxillary canines. Statistically significant values (p < 0.05) are in bold. |
||||||||||||
Discussion
The present report on radiological features of the maxillary permanent canines and the treatment carried out in relation to the occurrence of certain dental developmental abnormalities [17, 22] is based on the same representative age cohort of DPTs as the researchers’ earlier studies of maxillary canine eruption [7, 9].
The overlapping of maxillary canines was found to vary significantly more in the DAP children, and these more often had either clear overlapping or no overlapping at all. The non-DAP boys had either clear overlapping or some overlapping significantly more often than did the DAP boys. Thus, we can only partly accept our first hypothesis with regard to more pronounced overlapping in the canines of children with the dental developmental abnormalities studied here. On the other hand, there was no significant difference between the DAP and non-DAP children in the inclination angle of the maxillary canines, so that this part of the hypothesis must be rejected.
Our second hypothesis, concerning the treatment of maxillary canines was partly confirmed, since the canines of the children with dental developmental abnormalities received early treatment significantly more often. Interceptive treatment was carried out significantly more often in the DAP girls, while the DAP boys tended to receive early headgear treatment. Late treatment was less related to the occurrence of DAP features, and therefore our hypothesis concerning this must be rejected. The number of children in orthodontic treatment, including surgical exposure, was small, but orthodontic treatment was mentioned over twice as often (1.6% vs. 0.6%) in the children without dental developmental abnormalities.
The children in the present series were equally divided in terms of chronological age both between the genders and between the DAP and non-DAP groups. Delayed dental age is one feature involved in DAP [17], and it has also been connected with eruption disturbances in the maxillary canines [21, 37, 38]. Delayed dental age was found in this material to be associated with early treatment, suggesting that early treatment should be started early enough, i.e. after the first mixed stage. As expected, the dental ages of the children with DAP were later and varied by as much as five and a half years in these children as opposed to four and a half years in the non-DAP children. These findings reflect differences in occlusal development and underline the importance of evaluating the mixed dentition stage as part of the overall dental examination.
It has been found earlier that canine root development neither differ between normal and ectopic canines [6] nor between naturally erupting and treated canines [9]. In this study the early stage of canine root development in the DAP children can be attributed to the delayed dental age, our new finding was that advanced root development (at least two-thirds completed) occurred more often in the DAP children than in the non-DAP children.
A couple of years before the maxillary canines erupt into the oral cavity the development of the lateral incisors is in most cases incomplete and more often complete in girls [7, 9]. Thus, a comparison of the DAP and non-DAP groups showed lateral incisor development to differ only in the boys, whereas those with DAP more often had incomplete lateral incisors. The background to this may be that delayed dental age is one of the studied DAP features.
As a feature involved in DAP, absent teeth were slightly associated with the treatment of a maxillary canine. This is in line with earlier findings that children with absent teeth more often presented with ectopic eruption of a maxillary canine [16, 19].
One limitation of this work can be seen in its retrospective design and the cross-sectional sample represented by the DPTs. Due to variation in dental development, some of the DAP features might have been visible before or after the DPTs had been taken. In the light of the senior orthodontist’s treatment plans, some children had received orthodontic treatment for the primary dentition or during the early mixed stage (before the DPT), probably in the form of a Quad Helix for posterior cross-bite, braces on the upper incisors to close a large medial diastema, slicing of the primary canines mesially in the case of minimum space deficiency during the eruption of the lateral incisors, or elastics for a first molar cross-bite. The method used here for dental age estimation [35] is gender-specific, and thus it should be observed that the dental age differences between the genders do not directly reflect gender differences in dental development stages. The subsamples used for assessing the treatment provided for the maxillary canines were substantially small, another limitation that must be considered when reflecting on the results.
Our findings with regard to the treatment provided represent a successful follow up and early treatment of maxillary canines in the children with dental developmental abnormalities. Nevertheless, the results underline the importance of monitoring the erupting canines in children with and without dental developmental abnormalities. The oral examinations for the present children were mainly carried out at one primary school level, and it is noticeable that dental age varied markedly. This may suggest that early treatment was completed in time, as dental development was later in the DAP children. It is necessary to monitor the erupting maxillary canines after the first mixed stage in the dentition, and by evaluating the child’s dental developmental stage it is possible to enable early treatment. Early treatment after the first mixed stage, e.g. with headgear [14, 15], can ensure proper space conditions for the canines to erupt. Similar studies will be needed to verify these results and support clinical decision-making.
Conclusion
A couple of years before the eruption of a maxillary canine the DPT showed that:
- Either no overlapping or clear overlapping occurred more often in the DAP children, while canine inclination did not differ between the DAP and non-DAP children.
- The root development stage of the canines was more often either at the beginning or advanced in the DAP children.
The canines of the DAP children had more often undergone early treatment and delayed dental age as a DAP feature was associated with this early treatment. This enabled the proper timing of early treatment in relation to the dental developmental stage.
Acknowledgments
The authors wish to express their thanks to the oral healthcare personnel at the Health Centre in Lapinlahti, for making this study possible. They would also like to thank Eeva Melaluoto (EM), Jenni Iivari (JI) and Eelis Rytkonen (ER) for their work with the DAP feature determinations.
References
[1] Broadbent BH. Ontogenic development of occlusion. Angle Orthod. 1941;11:223–41.
[2] Coulter J, Richardson A. Normal eruption of the maxillary canine quantified in three dimensions. Eur J Orthod. 1997;19(2):171–83. https://doi.org/10.1093/ejo/19.2.171
[3] Becker A, Chaushu S. Etiology of maxillary canine impaction: a review. Am J Orthod Dentofacial Ortho. 2015;148(4):557–67. https://doi.org/10.1016/j.ajodo.2015.06.013
[4] Haavikko K. The formation and the alveolar and clinical eruption of the permanent teeth. An Orthopantomographic Study. Suom Hammaslaak Toim. 1970;66(3):103–70.
[5] Fernández E, Bravo LA, Canteras M. Eruption of the permanent upper canine: a radiologic study. Am J Orthod Dentofacial Orthop. 1998;113(4):414–20. https://doi.org/10.1016/S0889-5406(98)70251-3
[6] Sajnani AK, King NM. Early prediction of maxillary canine impaction from panoramic radiographs. Am J Orthod Dentofacial Orthop. 2012;142(1):45–51. https://doi.org/10.1016/j.ajodo.2012.02.021
[7] Ristaniemi J, Rajala W, Karjalainen T, et al. Eruption pattern of the maxillary canines: features of natural eruption seen in DPT at the late mixed stage-Part I. Eur Arch Paediatr Dent. 2022;23(2):223–32. https://doi.org/10.1007/s40368-021-00650-1
[8] Chalakkal P, Thomas AM, Chopra S. Displacement, location, and angulation of unerupted permanent maxillary canines and absence of canine bulge in children. Am J Orthod Dentofac Orthop. 2011;139(3):345–50. https://doi.org/10.1016/j.ajodo.2009.03.044
[9] Ristaniemi J, Karjalainen T, Kujasalo K, et al. Eruption pattern of the maxillary canines: features indicating treatment needs as seen in DPT at the late mixed stage-Part II. Eur Arch Paediatr Dent. 2022;23(4):567–78. https://doi.org/10.1007/s40368-022-00719-5
[10] Ericson S, Kurol J. Early treatment of palatally erupting maxillary canines by extraction of the primary canines. Eur J Orthod. 1988;10(4):283–95. https://doi.org/10.1093/ejo/10.4.283
[11] Power SM, Short MB. An investigation into the response of palatally displaced canines to the removal of deciduous canines and an assessment of factors contributing to favourable eruption. Br J Orthod. 1993;20(3):215–23. https://doi.org/10.1179/bjo.20.3.215
[12] Bazargani F, Magnuson A, Lennartsson B. Effect of interceptive extraction of deciduous canine on palatally displaced maxillary canine: a prospective randomized controlled study. Angle Orthod. 2014;84(1):3–10. https://doi.org/10.2319/031013-205.1
[13] Naoumova J, Kurol J, Kjellberg H. Extraction of the deciduous canine as an interceptive treatment in children with palatal displaced canines – part I: shall we extract the deciduous canine or not? Eur J Orthod. 2015;37(2):209–18. https://doi.org/10.1093/ejo/cju040
[14] Silvola AS, Arvonen P, Julku J, et al. Early headgear effects on the eruption pattern of the maxillary canines. Angle Orthod. 2009;79(3):540–5. https://doi.org/10.2319/021108-83.1
[15] Hadler-Olsen S, Pirttiniemi P, Kerosuo H, et al. Does headgear treatment in young children affect the maxillary canine eruption path? Eur J Orthod. 2018;40(6):583–91. https://doi.org/10.1093/ejo/cjy013
[16] Baccetti T. A controlled study of associated dental anomalies. Angle Orthod. 1998;68(3):267–74.
[17] Peck S. Dental Anomaly Patterns (DAP). A new way to look at malocclusion. Angle Orthod. 2009;79(5):1015–16. https://doi.org/10.2319/0003-3219-079.005.1015
[18] Brin I, Becker A, Shalhav M. Position of the maxillary permanent canine in relation to anomalous or missing lateral incisors: a population study. Eur J Orthod. 1986;8(1):12–16. https://doi.org/10.1093/ejo/8.1.12
[19] Pirinen S, Arte S, Apajalahti, S. Palatal displacement of canine is genetic and related to congenital absence of teeth. J Dent Res. 1996;75(10):1742–6. https://doi.org/10.1177/00220345960750100601
[20] Baccetti T, Leonardi M, Giuntini V. Distally displaced premolars: a dental anomaly associated with palatally displaced canines. Am J Orthod Dentofacial Orthop. 2010;138(3):318–22. https://doi.org/10.1016/j.ajodo.2008.09.036
[21] Rozylo-Kalinowska I, Kolasa-Raczka A, Kalinowski P. Dental age in patients with impacted maxillary canines related to the position of the impacted teeth. Eur J Orthod. 2011;33(5):492–7. https://doi.org/10.1093/ejo/cjq123
[22] Ristaniemi J, Kujasalo K, Rytkonen E, et al. Features of dental anomaly patterns in Finnish children as seen in panoramic radiographs at the late mixed stage. Acta Odontol Scand. 2023;81:609–14. https://doi.org/10.1080/00016357.2023.2232859
[23] Peck L, Peck S, Attia Y. Maxillary canine-first premolar transposition, associated dental anomalies and genetic basis. Angle Orthod. 1993;63(2):99–110.
[24] Peck S, Peck L, Kataja M. The palatally displaced canine as a dental anomaly of genetic origin. Angle Orthod. 1994;64(4):249–56.
[25] Peck S, Peck L, Kataja M. Mandibular lateral incisor-canine transposition, concomitant dental anomalies, and genetic control. Angle Orthod. 1998;68(5):455–66.
[26] Langberg BJ, Peck S. Tooth-size reduction associated with occurrence of palatal displacement of canines. Angle Orthod. 2000;70(2):126–8.
[27] Shalish M, Peck S, Wasserstein A, et al. Malposition of unerupted mandibular second premolar associated with agenesis of its antimere. Am J Orthod Dentofacial Orthop. 2002;121(1):53–6. https://doi.org/10.1067/mod.2002.120399
[28] Peck S, Peck L, Kataja M. Concomitant occurrence of canine malposition and tooth agenesis: evidence of orofacial genetic fields. Am J Orthod Dentofacial Orthop. 2002 Dec;122(6):657–60. https://doi.org/10.1067/mod.2002.129915
[29] Garib DG, Peck S, Gomes SC. Increased occurrence of dental anomalies associated with second-premolar agenesis. Angle Orthod. 2009;79(3):436–41. https://doi.org/10.2319/021308-87.1
[30] Shalish M, Peck S, Wasserstein A, et al. Increased occurrence of dental anomalies associated with infraocclusion of deciduous molars. Angle Orthod. 2010;80(3):440–5. https://doi.org/10.2319/062609-358.1
[31] Grahnén H. Hypodontia in the permanent dentition. Odontol Revy. 1956;7:1–100.
[32] Nelson SJ. The permanent maxillary incisors. In: Wheeler’s dental anatomy, physiology and occlusion. 11th ed. St. Louis, MO: Elsevier; 2019, pp. 90–102.
[33] Demirjian A, Goldstein H, Tanner JM. A new system of dental age assessment. Hum Biol. 1973;45(2):211–27.
[34] Demirjian A, Goldstein H. New systems for dental maturity based on seven and four teeth. Ann Hum Biol. 1976;3(5):411–21. https://doi.org/10.1080/03014467600001671
[35] Chaillet N, Nystrom M, Kataja M, et al. Dental maturity curves in Finnish children: Demirjian’s method revisited and polynomial functions for age estimation. J Forensic Sci. 2004;49(6):1324–31. https://doi.org/10.1520/JFS2004211
[36] Nolla CM. The development of the permanent teeth. J Dent Child. 1960;27:254–266.
[37] Becker A, Chaushu S. Dental age in maxillary canine ectopia. Am J Orthod Dentofacial Orthop. 2000;117(6):657–62. https://doi.org/10.1016/S0889-5406(00)70174-0
[38] Naser DH, Abu Alhaija ES, Al-Khateeb SN. Dental age assessment in patients with maxillary canine displacement. Am J Orthod Dentofacial Orthop. 2011;140(6):848–55. https://doi.org/10.1016/j.ajodo.2011.04.027