RESEARCH ARTICLE
Impact of acquisition volume on cone beam computed tomography imaging of marginal bone: an ex vivo study
Maurice Ruettersa , Korallia Alexandroub, Holger Gehriga, Sinclair Awounvoc, Ti-Sun Kima, Anna Feltena, Christopher Luxb and Sinan Send
, Korallia Alexandroub, Holger Gehriga, Sinclair Awounvoc, Ti-Sun Kima, Anna Feltena, Christopher Luxb and Sinan Send
aDepartment of Conservative Dentistry, University Hospital Heidelberg, Heidelberg, Germany; bDepartment of Orthodontics, University Hospital Heidelberg, Heidelberg, Germany; cInstitute of Medical Biometry, University Hospital Heidelberg, Heidelberg, Germany; dDepartment of Orthodontics, University Hospital Schleswig Holstein, Kiel, Germany
ABSTRACT
Objective: The current study explores whether there is a clinically relevant distinction in the measurement of marginal bone loss when comparing high-dose (HD) versus low-dose (LD) cone beam computed tomography (CBCT) protocols in small and large acquisition volumes.
Material and Methods: CBCTs of four human cadaveric preparates were taken in HD and LD mode in two different fields of view 8 × 8 cm2 (LV) and 5 × 5 cm2 (SV). In total, 43 sites of 15 teeth were randomly chosen, and marginal bone loss was measured twice in all protocols at 43 sites of 15 teeth by one calibrated investigator. Bland-Altman plots and Lin’s concordance correlation coefficient (CCC) were calculated to assess the extent of agreement of the measurements. Additionally, the rater scored the certainty in each of the measurements.
Results: For HD-CBCT CCC of measurements obtained using SV versus LV was 0.991. CCC of measurements obtained using SV versus LV of LD-CBCT was 0.963. Both CCC values indicated excellent agreement between the two volumes in both protocols.
CCC also indicated high intramodality correlation between HD-CBCT and LD-CBCT independent of the acquisition volume (0.963 – 0.992). Bland-Altman plots also indicated no substantial differences. Results of certainty scoring showed significant differences (p = 0.004 (LV), p < 0.001(SV)) between the LD and HD-CBCT.
Conclusions: Accuracy of measurements of bone loss shows no clinical noticeable effects depending on the CBCT volume in this ex vivo study. There appears to be no relevant advantage of SV over LV, neither in HD-CBCT nor in LD-CBCT and additionally no relevant advantage of HD versus LD in visualizing marginal bone loss.
KEYWORDS: Cone beam computed tomography; low-dose cone beam computed tomography; computed radiography; periodontitis; periodontal bone defects
Citation: ACTA ODONTOLOGICA SCANDINAVICA 2024; VOL. 83: 204–209. DOI: https://doi.org/10.2340/aos.v83.40494.
Copyright: © 2024 The Author(s). Published by MJS Publishing on behalf of Acta Odontologica Scandinavica Society. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 23 January 2024; Accepted: 16 March 2024; Published: 25 April 2024.
CONTACT Maurice Ruetters maurice.ruetters@med.uni-heidelberg.de Department of Conservative Dentistry, University Hospital Heidelberg, Im Neuenheimer Feld 400, 69115 Heidelberg, Germany
Competing interests and funding: The authors declare that they have no conflict of interest.
The work was supported by the Department of Operative Dentistry, the Department of Orthodontics, and the Department of Oral and Maxillofacial Surgery of the University Hospital Heidelberg as well as the Department of Orthodontics of the University Medical Center Schleswig-Holstein. Maurice Ruetters is partly funded by the Physician-Scientist Program of Heidelberg University, Faculty of Medicine. The study is also funded by a fellowship of the Deutsche Gesellschaft für Zahn-Mund-und Kieferheilkunde (DGZMK).
Introduction
In recent years, the field of dental three-dimensional imaging has witnessed the introduction of an increasing array of cone beam computed tomography (CBCT) protocols, each designed to enhance diagnostic capabilities while addressing growing concerns about patient radiation exposure [1]. A significant thrust in this domain has been the development and optimization of strategies aimed at minimizing the radiation dose associated with CBCT. Among these strategies, the implementation of pre-programmed ‘low-dose’ (LD) protocols has emerged as a prominent approach [2]. The diagnostic efficacy of these LD protocols for a variety of clinical indications, such as the detailed visualization of peri-implant defects and complex periodontal structures, including furcations and marginal bone, has undergone extensive scrutiny and evaluation by multiple research groups. The outcomes of these investigations have been promising, suggesting that LD protocols could play a pivotal role in establishing a new standard for three-dimensional imaging, particularly in specialized fields like periodontology [3–6]. Furthermore, there are already initial studies that have investigated the suitability of low-dose digital volume tomography (LD-CBCT) in a clinical setting, for example, for the assessment of anatomical structures near wisdom teeth. Here too, the results were predominantly positive. The only exception was that the periodontal gap could be better determined in conventional CBCT protocols [7].
Concurrently, another significant approach to radiation reduction involves the strategic minimization of the acquisition volume [8]. This method not only achieves a decrease in radiation exposure but also leads to benefits such as reduced image noise and therefore enhanced image clarity [9, 10]. This aspect is particularly pertinent when imaging fine anatomical structures like the marginal bone, where precision is paramount. The visualization of the marginal bone holds substantial relevance in both periodontal and orthodontic treatment planning, as accurate knowledge of its morphology can aid in circumventing adverse effects like gingival recessions, which might arise from excessive tooth movements beyond the confines of the bony dental arch [11]. However, it is important not to choose volumes that are too small, in order to capture the regions of interest within a single image, thereby selecting a volume appropriate to the indication to avoid duplicate representations of the structures and the associated higher radiation exposure. Nonetheless, the question remains whether, in specific cases, a smaller volume might provide more detailed information regarding the marginal bone.
The aim of this study is therefore to validate whether there is a relevant advantage in illustrating marginal bone loss using small volumes (SV) compared to large volumes (LV) in LD as well as HD CBCT protocols.
Therefore, the hypotheses were:
- Small-volume CBCT has no advantages over LV CBCT in depicting marginal bone loss, both in LD and HD protocols.
- Low-dose CBCT is as suitable as HD CBCT for depicting marginal bone loss, both in small and large volume acquisitions.
Materials and methods
This ex vivo study investigated 43 sites of 15 teeth from four human hemisected cadaveric heads. The number of different tooth types included in this study is listed in Table 1. Three of the teeth had amalgam restorations. The others were free of restorations.
| Tooth type | number |
| Upper molars | 5 |
| Upper premolars | 4 |
| Lower molars | 4 |
| Lower premolars | 2 |
The heads were from bodies donated to the Institute of Anatomy and Cell Biology of the University of Heidelberg and were preserved with 99% ethanol, glycerin, and 37% formalin. At the time of the radiographic investigations, the hemisected cadaveric heads, including the mandibles, were fully covered by soft tissue and by the adjacent muscles of the cheek. The tongue, neck muscles, base of the skull, and cervical vertebrae were also still present. To ensure clear reproducibility of the image planes in the different acquisition modes, two depressions were made at the sites of the crown, where the measurements were performed by means of a round diamond burr (801L 314 016, Komet Dental, Gebr. Brasseler GmbH & Co. KG, Lemgo, Germany). The teeth were then radiographically imaged using two CBCT protocols (Figure 1): one LD-CBCT protocol and one high-dose (HD) CBCT protocol of one device (Veraview X800, J. Morita Europe, Dietzenbach, Germany) in the very same position.
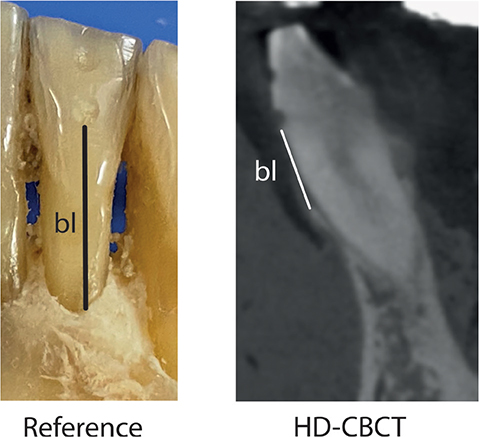
Figure 1. Measurement scheme. Left image (Reference): schematic image of the reference measurements bl. Right image (HD-CBCT): schematic image of the corresponding measurement in a HD-CBCT image. The orientation procedure was as follows: (1) the two depressions were identified, and the axis of the coronal plane was placed through the center of the depressions. (2) The axial slice was then aligned with the lower depression. (3) Measurements bl were then taken in the sagittal plane.
The volumetric acquisition protocols were as follows:
- HD-CBCT protocol LV: 17.9 s radiation time, 5.00 mA, 102 kV, FOV 8 × 8 cm2, isotropic voxel size 0.125 mm, DAP 1396.95 mGy cm2.
- LD-CBCT protocol LV: 9.4 s radiation time, 1.6 mA, 72 kV, FOV 8 x 8 cm2, isotropic voxel size 0.125 mm, DAP 87, 19 mGy cm2
- HD-CBCT protocol SV: 17.9 s radiation time, 5.00 mA, 102 kV, FOV 4 × 4 cm2, isotropic voxel size 0.08 mm, DAP 383.57 mGy cm2.
- LD-CBCT protocol SV: 9.4 s radiation time, 1.6 mA, 72 kV, FOV 4 x 4 cm2, isotropic voxel size 0.125 mm, DAP 23.00 mGy cm2
The protocols were chosen because the field of view (FOV) of 8 × 8 allows for the depiction of the majority of the complete dentition. 4 × 4 was selected as it represents the smallest possible FOV of the available CBCT scanner. Additionally, the 8 × 8 protocol enabled comparability with previously conducted studies. The HD parameters were selected according to the manufacturer’s recommendations for an optimal image quality. For the LD protocols, the parameters were chosen to achieve the lowest possible radiation dose with the device. Analogous to previous studies, during imaging, gel pads were used to imitate the other half of the head to achieve tissue-equivalent volumes and ensure the most lifelike absorption of radiation [16]. The heads were fixed in position by placing the throat in a tube, and they were oriented in accordance with the orientation lines specified by the manufacturer.
Probe measurements – reference standard
After radiological imaging, the gingiva was carefully removed by means of microsurgical instruments to ensure the bone was not damaged. Subsequently, in the axis of the previously milled depressions, the distance from the most apical point of the lower depression to the alveolar crest was measured on each site by means of a periodontal probe (Florida Probe, Clark Dental Equipment Systems Ltd, UK) with a 0.1 mm scale. Thus, a reference standard for bone loss (bl) measurements was established. These measurements were made by one experienced investigator (M. R.), who had previously been calibrated on a model. For calibration, the investigator had to successfully reproduce (relative agreement of 95%) the principal investigator’s (T. K.) bone-sounding measurements of clinical attachment loss at 168 sites on a standardized ex vivo reference model with a transparent gingiva (Co. M. Tech, Korea). These measurements are henceforth referred to as ‘probe measurements’ (Figure 1).
Image review
For analysis, CBCT data was exported in DICOM format to the application software OSIRIX pro (aycanOsiriX 2.06.000). Windowing and levelling were allowed. Evaluations were all performed. All evaluations were performed on the same workstation and monitor (iMac, 27 in., Apple, California, USA) in the same dark room.
Measurement procedure has already been described in an earlier publication [5]. The orientation procedure was as follows: (1) The two depressions were identified, and the axis of the coronal plane was placed through the center of the depressions. (2) The axial slice was then aligned with the lower depression. (3) In the sagittal, measurements of bl were then taken in the sagittal plane. The images were reviewed by one calibrated dentist (K.A.) in multiplanar reconstruction. The measurement procedure is explained and shown in Figure 1.
For calibration of the method, the rater performed the measurements and segmentations in 20 teeth of different CBCT datasets to the ones of this study and discussed them with another highly experience rater (MR) with more than 10 years of experience in CBCT diagnostics till consensus was found.
Additionally, the rater scored the certainty in each of the measurements as ‘confident’, ‘diagnostically acceptable’, and ‘not confident’.
Statistical analysis
For statistical analysis, the Lin’s CCC was calculated alongside 95% confidence intervals to assess the agreement between measurements obtained using LD-CBCT LV and SV as opposed to using HD-CBCT LV and SV as well as using LD-CBCT LV as opposed to using LD-CBCT SV and using HD-CBCT LV as opposed to using HD-CBCT SV. Bland-Altman plots were drawn separately per trial (method agreement) to graphically support the analysis of measurements agreement. Moreover, a Wilcoxon two-sample signed rank test was used to compare the measurements’ certainty of the rater between the modalities.
The analysis was performed using the statistical software R version 4.2.1.
Results
Figure 2A–D descriptively shows the distribution of marginal bone loss measurements of the different modalities and volumes.
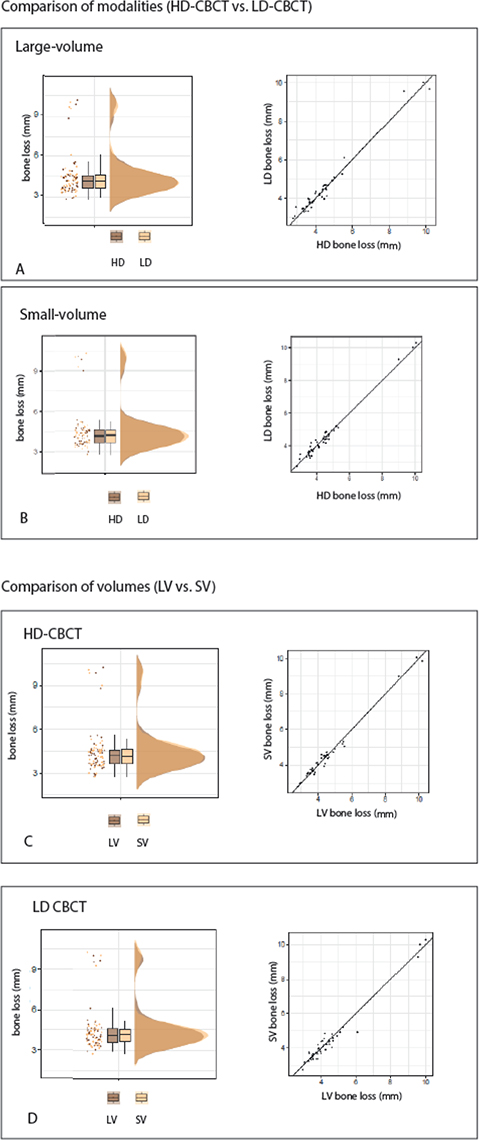
Figure 2. Descriptive statistics of the different modalities and volumes.
Lin’s CCC of the different volumes compared with the reference measurements and Lin’s CCC of the comparison of different volumes are shown in Table 2.
Supporting Bland-Altman analysis is shown in Figure 3A–D. All means of measurements are around 0 and limits of 95% of agreements within clinically acceptable range (< 1 mm). Means of differences show no systematic over- or underestimation of any modality.
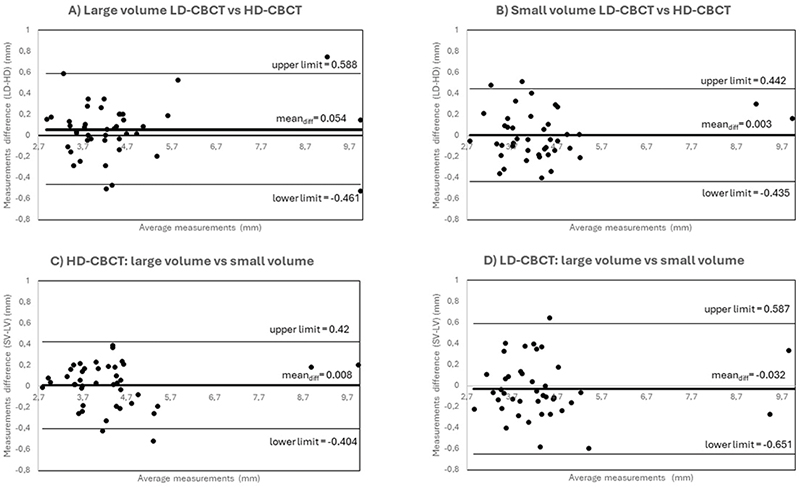
Figure 3. Bland-Altman Plots of (A) measurements of LV LD-CBCT versus HD-CBCT (B) measurements of SV LD-CBCT versus HD-CBCT (C) LV HD-CBCT measurements versus SV HD-CBCT measurements (D) LV LD-CBCT measurements versus SV LD-CBCT measurements.
Results of certainty scoring are shown in Table 3. Significant differences were only shown between the LD and HD-CBCT but not depending on the CBCT volume.
| Modalities | p | ||
| HD-CBCT LV | vs. | HD-CBCT SV | |
| 1.628 ± 0.62 | 1.721 ± 0.50 | 0.384 | |
| LD-CBCT LV | vs. | LD-CBCT SV | |
| 1.286 ± 0.67 | 1.023 ± 0.64 | 0.061 | |
| HD-CBCT LV | vs. | LD-CBCT LV | |
| 1.628 ± 0.62 | 1.286 ± 0.67 | 0.004* | |
| HD-CBCT SV | vs. | LD-CBCT SV | |
| 1.721 ± 0.50 | 1.023 ± 0.64 | < 0.001* | |
| * = significant. | |||
Discussion
The results of the study confirm both hypotheses that SV CBCT has no advantages over LV CBCT in depicting marginal bone loss, both in LD and HD protocols, and that LD CBCT is as suitable as HD CBCT for depicting marginal bone loss, both in small and large volume acquisitions. High Lin’s CCC values (> 0.9) show equal potential of LV compared to SV in both, HD-CBCT and LD-CBCT (Table 3). Bland-Altman Plots indicate means of measurements around 0 for measurements of marginal bone loss for both modalities and volume sizes showing that there is no substantial over- or underestimation of neither small nor large volume as well as LD-CBCT or HD-CBCT. The differences observed in measurements are all smaller 1 mm and within clinical tolerance values.
Lin’s CCC was also substantial to almost perfect for all modalities compared to the clinical references (Table 2). The results are in line with other studies that have addressed the suitability of CBCT for imaging dental structures. These studies have shown not only the potential of HD-CBCT but also the significant potential of LD-CBCT in depicting periodontal bone structures [2, 5, 6, 12].
Concerning the certainty of measurements, significant differences were only seen between LD-CBCT and HD-CBCT but not dependent on the volume (Table 4). Due to the subjectively perceived poorer image quality of LD-CBCT, these results are not surprising and in line with the results of an existing study by Charuakkra et al. [13]. However, the effects on the actual measurement results are not clinically relevant. The results confirm the assumption that more experience of the examiner is necessary for a better and confidenter interpretation of LD-CBCT images as already shown for endodontic tasks in HD-CBCT [14].
Limitations
The ex vivo nature of the experiments eliminated the risk of natural motion, such as tremors, which can lead to motion artifacts that can significantly reduce the quality and information content of the image [9, 15].
Only half heads were used. To mimic the missing half, gel pads were used as described in the Methods section. However, these pads cannot imitate natural bony structures, teeth, or restorative materials or the artifacts caused by these structures. This means that the image quality may have been slightly better than it would have been for complete heads [16].
Conclusion
Accuracy of measurements of bone loss show no clinical noticeable effects depending on the CBCT volume in this ex vivo study. There appears to be no relevant advantage of SV over LV, neither in HD-CBCT nor in LD-CBCT and additionally no relevant advantage of HD versus LD in visualizing marginal bone loss. This means: choosing a smaller volume as well as HD protocols does not improve the assessability of marginal bone loss in either LD- or HD-CBCT. In accordance with European guidelines, it is clinically imperative to always employ the lowest feasible radiation dose to achieve optimal patient outcomes with respect to the indication [17]. In conclusion of the present findings, the smallest LD protocol possible in dependence of the indication should be utilized for the depiction of marginal bone loss whenever possible. For instance, to depict the entire dentition in periodontally diseased but still fully dentate patients, who require a CBCT scan before the initiation of therapy, an FOV 8 × 8 cm should be used. Conversely, for planning surgically complex procedures on a single tooth involved in furcation, a small field in low dose would suffice. However, it should be noted that this is an in vitro study, and the results need to be confirmed in vivo, not least because of the limitations discussed previously.
Acknowledgments
Special thanks to Sara Doll of the Department of Anatomy and Cell Biology of the University of Heidelberg for their support.
Author contributions
Maurice Ruetters, Holger Gehrig, Sinclair Awounvo, Ti-Sun Kim, Korallia Alexandrou, Anna Felten, Christopher Lux, and Sinan Sen contributed substantially to the study conception and design. Substantial material preparation and data collection were performed by Maurice Rütters, Korallia Alexandrou, and Sinan Sen. Substantial analysis was performed by Sinclair Awounvo, Maurice Rütters, and Sinan Sen. The first draft of the manuscript was written by Maurice Rütters and Sinan Sen; all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethical approval
All procedures involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the ethical review board of the University of Heidelberg, Germany (S-017/2020) and by the ethical review board of the medical association of Rhineland-Palatinate (Germany) (2021-15661).
Informed consent
Informed consent was not required for this study, because human donors have already given their consent beforehand for donation of their body to the Department of Anatomy and Cell Biology of the University of Heidelberg for research.
ORCID
Maurice Ruetters,  https://orcid.org/0000-0001-9945-7286
https://orcid.org/0000-0001-9945-7286
References
[1] Ludlow JB, Timothy R, Walker C, et al. Effective dose of dental CBCT-a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofac Radiol. 2015;44(1):20140197. https://doi.org/10.1259/dmfr.20140197
[2] Yeung AWK, Jacobs R, Bornstein MM. Novel low-dose protocols using cone beam computed tomography in dental medicine: a review focusing on indications, limitations, and future possibilities. Clin Oral Investig. 2019 Jun;23(6):2573–2581. https://doi.org/10.1007/s00784-019-02907-y
[3] Horsch L, Labis C, Trebing CT, et al. Predictability and image quality of low-dose cone-beam computed tomography in computer-guided implantology: an experimental study. J Dent. 2021 Sep;112:103744. https://doi.org/10.1016/j.jdent.2021.103744
[4] Ruetters M, Gehrig H, Kim TS, et al. Imaging furcation defects with low-dose cone beam computed tomography. Sci Rep. 2022 Apr 26;12(1):6824. https://doi.org/10.1038/s41598-022-10781-0
[5] Ruetters M, Gehrig H, Kronsteiner D, et al. Low-dose CBCT imaging of alveolar buccal bone adjacent to mandibular anterior teeth – a pilot study. Clin Oral Investig. 2022;26(5):4173–4182. PMCID: PMC9072474 PMID: 35103838 https://doi.org/10.1007/s00784-022-04389-x
[6] Schwindling FS, Hilgenfeld T, Weber D, et al. In vitro diagnostic accuracy of low-dose CBCT for evaluation of peri-implant bone lesions. Clin Oral Implants Res. 2019 Dec;30(12):1200–1208. https://doi.org/10.1111/clr.13533
[7] Cederhag J, Iskanderani D, Alstergren P, et al. Visibility of anatomical landmarks in the region of the mandibular third molar, a comparison between a low-dose and default protocol of CBCT. Acta Odontol Scand. 2023 2023/08/18;81(6):449–455.
[8] Ting S, Attaia D, Johnson KB, et al. Can modifying shielding, field of view, and exposure settings make the effective dose of a cone-beam computed tomography comparable to traditional radiographs used for orthodontic diagnosis? Angle Orthod. 2020 Sep 1;90(5):655–664. https://doi.org/10.2319/072819-496.1
[9] Kiljunen T, Kaasalainen T, Suomalainen A, et al. Dental cone beam CT: a review. Phys Med. 2015 2015/12/01/;31(8):844–60. https://doi.org/10.1016/j.ejmp.2015.09.004
[10] Heinz-Theo Lübbers KD. Digitale volumentomographie. Vol. 1. Berlin HSBH, editor. 2021. https://doi.org/10.1007/978-3-662-57405-8
[11] Cortellini P, Bissada NF. Mucogingival conditions in the natural dentition: narrative review, case definitions, and diagnostic considerations. J Clin Periodontol. 2018 Jun;45 Suppl 20:S190–S198. https://doi.org/10.1111/jcpe.12948
[12] Ruetters M, Gehrig H, Kronsteiner D, et al. Ex-vivo imaging of buccal and oral periodontal bone with low-dose CBCT in porcine jaws. Dentomaxillofac Radiol. 2022 Jan 1;51(1):20210233. https://doi.org/10.1259/dmfr.20210233
[13] Charuakkra A, Mahasantipiya P, Lehtinen A, et al. Comparison of subjective image analysis and effective dose between low-dose cone-beam computed tomography machines. Dentomaxillofac Radiol. 2023 Jan;52(2):20220176. https://doi.org/10.1259/dmfr.20220176
[14] Parker JM, Mol A, Rivera EM, et al. Cone-beam computed tomography uses in clinical endodontics: observer variability in detecting periapical lesions. J Endod. 2017 Feb;43(2):184–187. https://doi.org/10.1016/j.joen.2016.10.007
[15] Brüllmann D, Schulze RKW. Spatial resolution in CBCT machines for dental/maxillofacial applications – what do we know today? Dentomaxillofac Radiol. 2015;44(1):20140204. https://doi.org/10.1259/dmfr.20140204
[16] McGarry CK, Grattan LJ, Ivory AM, Leek F, Liney GP, Liu Y et al. Tissue mimicking materials for imaging and therapy phantoms: a review. Phys Med Biol. 2020 Dec 16;65(23). PMID: 32998112. https://doi.org/10.1088/1361-6560/abbd17
[17] Commission E, Energy D-Gf. Cone beam CT for dental and maxillofacial radiology – evidence-based guidelines. Publications Office; 2012.