RESEARCH ARTICLE
Complications and complaints in craniofacial fractures – Finnish national data for 20 years
Inka Luotamoa,b, Johanna Snällc,d and Miika Toivaric,d
aDepartment of Oral and Maxillofacial Diseases, Kymenlaakso Central Hospital, Kotka, Finland; bUniversity of Helsinki, Helsinki, Finland; cDepartment of Oral and Maxillofacial Diseases, University of Helsinki, Helsinki, Finland; dHelsinki University Hospital, Helsinki, Finland
ABSTRACT
Objective: Research on reasons for malpractice claims in oral and maxillofacial surgery is scarce. The aim of this study was to investigate the causes and prevalence of permanent harm among craniofacial fracture related malpractice claims.
Materials and methods: A retrospective register study was designed and implemented. All patients with a complaint and a diagnosis of facial or cranial fracture were included. The main outcome was the presence of permanent harm, and the predictor variable was the cause of complaint. Chi-square test was used for estimation of statistical significance.
Results: Delay in correct diagnosis was the leading cause of malpractice claims (63.2%), and permanent harm was found in 23.1% of the population. 82.4% of injuries were facial fractures in total population. 65.3% (n = 98) of facial trauma were related with delayed diagnostics (p < 0.001). Permanent harm was more frequent in patients with delayed diagnosis (71.4%) than those without (60.7%, p = 0.299).
Conclusions: Claims of craniofacial trauma are related with under-diagnostics, and un-diagnosed facial fracture can lead to a high rate of permanent harm. Systematic clinical evaluation and facial trauma specialist consultation is recommended to set early correct diagnosis for and improve treatment of craniofacial trauma patients.
KEYWORDS: Craniofacial fracture; complaint; malpractice; delayed diagnosis; permanent harm
Citation: ACTA ODONTOLOGICA SCANDINAVICA 2024; VOL. 83: 334–339. DOI: https://doi.org/10.2340/aos.v83.40570.
Copyright: © 2024 The Author(s). Published by MJS Publishing on behalf of Acta Odontologica Scandinavica Society. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 29 January 2024; Accepted: 29 March 2024; Published: 28 May 2024.
CONTACT Dr. Inka Luotamo, inka.luotamo@iki.fi Kymenlaakso Central Hospital - Oral and maxillofacial diseases, Kotkantie 41, Kotka, Kotka 48210, Finland
Competing interests and funding: The authors have no potential conflicts of interest to report.
Inka Luotamo received a grant from the Paulo Foundation. Open access funded by Helsinki University Library.
Introduction
The risk of complications and complaints is always present in medical treatment and care. A recent review concluded that 49–65% of complaints are related to general practice. However, surgery has been reported among the most high-risk specialties receiving complaints [1, 2], the risk being up to 12-fold higher than in general practice [3].
The factors which have been associated with malpractice complaints in general surgery have been history of previous claims, lack of diagnosis, heavy workload, practitioners’ older age, monitoring, and follow-up. [1, 3, 4] In addition to the factors previously mentioned, communication between practitioner and patient has a clear impact on dissatisfaction with treatment [4].
In maxillofacial surgery, malpractice complaints have been reported in relation to orthognathic surgery, facial esthetics, temporomandibular joint disorder, dental implantology and tooth extraction related complications, facial injury related sensory disturbances, and scarring [5, 6–9]. Malocclusion, scar contracture, diplopia, malunion, wound dehiscence, and infection are well-documented complications in facial trauma [10]. A recent meta-analysis revealed that mandibular fracture infections (66.7%), followed by excessive scarring (20.7%), wound dehiscence (13.8%), and insufficient reposition (13.8%) were the most common types of complications in facial fracture patients [11].
Publications focussing on the background of demographics in facial trauma malpractice and complications are a few [12, 13]. The purpose of this study was to investigate the demographics and causes leading to malpractice complaints in craniofacial fracture patients in Finland. The specific aim was to clarify the reasons for complaints and the prevalence of permanent harm. Our hypothesis was that fracture treatment-related complications are the leading group in major craniofacial injuries.
Materials and methods
Study design and sample description
Patient liability insurance is statutory for all companies, institutions, private entrepreneurs, and healthcare professionals engaged in health and medical care activities in Finland. The insurance centre determines whether the claim is to be compensated and whether permanent harm has occurred, and corrective instructions are given in the case of malpractice. The records of all patients with a closed complaint of facial, cranial, or craniofacial fracture treatment were reviewed from the Finnish Patient Insurance Centre from 1 January 1999 to 31 December 2019. Complaints without a definitive decision were excluded from the study.
Study variables
All patients with a diagnosed facial, cranial, or combined craniofacial fracture were included in the study. The main outcome was the presence of permanent harm (i.e., present or absent).
The primary predictor variables comprised the cause of complaint grouped as follows: (1) delay of correct diagnosis or treatment with or without other complaints, (2) complication of fracture treatment or end-result of treatment, and (3) other. In addition, the number of the following specific causes of complaints was presented: delay of correct diagnosis or treatment, complication of fracture or end-result of treatment, under-diagnostics of associated injury (AI), improper instructions or medical treatment, and impolite or unprofessional behaviour.
The explanatory variables were sex, age, mechanism of injury, type of fracture, mortality due to injuries (i.e., yes or no), and missed diagnosis of AI. The injury mechanism was classified as follows: (1) fall on the ground, (2) assault, (3) hit by blunt object, (4) bicycle accident, (5) fall from height, (6) motor vehicle accident (MVA), or (7) other. The type of fracture was classified as follows: (1) cranial, (2) facial, or (3) craniofacial.
Data analysis
Descriptive statistics were calculated for all variables. A Chi-square test was used to evaluate the statistical significance between groups.
Ethical approval
The internal review board of the patient liability insurance centre of Finland approved the study protocol (PVK16042019).
Results
Table 1 shows the descriptive statistics of 182 patients with a malpractice committee complaint. Of these patients, 53.8% were male, the average age being 38 years. The most common cause of trauma was falling on the ground (34.1%), followed by assault (24.7%). Most injuries were pure facial fractures (82.4%). Delay of correct diagnosis or medical treatment was the predominant cause of complaint (63.2%). Permanent harm was determined for 23.1% of the patients, and 71.4% (130 patients) had financial coverage for their complaint.
The associations between sex, age, mechanism, type of fracture, mortality, missed AI, and cause of complaint are presented in Table 2. The frequency of 40- to 50-year-old patients was highest in three groups with different causes of complaint, 35.7% in delay related causes, 39.6% in complication of treatment, and 42.1% in other group, (p 0.574). Falling on the ground (37.4%) was the most common cause of injury in the group complaining of delayed diagnosis or treatment, and assault (39.6%) in the group citing complication of fracture treatment or end-result of fracture treatment, the difference being significant (p = 0.026). Facial fracture was by far the most common type of injury in the delay (85.2%), complication (87.5%), and other (52.6%) groups, the difference being significant (p < 0.001). Altogether 7 of the 9 missed AIs were associated with complaints of delayed diagnosis or treatment; the association was however, not significant (p = 0.886).
| Study variables | Delay of correct diagnosis or treatment ± end result ± complication of fracture treatment | Complication of fracture or end result of treatment | Other | % | P* | ||
| n = 115 | % | n = 48 | % | n = 19 | |||
| Sex | 0.839 | ||||||
| Male | 61 | 53.0 | 24 | 50.0 | 11 | 57.9 | |
| Female | 54 | 47.0 | 24 | 50.0 | 8 | 42.1 | |
| Age (yrs.) | 0.0 | ||||||
| Range | 0–91 | 6–86 | 11–75 | ||||
| Mean | 36.84 | 39.35 | 44.63 | ||||
| Age group (yrs.) | 0.574 | ||||||
| <18 | 25 | 21.7 | 8 | 16.7 | 1 | 5.3 | |
| 19–39 | 38 | 33.0 | 16 | 33.3 | 6 | 31.6 | |
| 40–59 | 41 | 35.7 | 19 | 39.6 | 8 | 42.1 | |
| 60+ | 11 | 9.6 | 5 | 10.4 | 4 | 21.1 | |
| Mechanism | 0.026 | ||||||
| Fall on the ground | 43 | 37.3 | 13 | 27.1 | 6 | 31.6 | |
| Assault | 25 | 21.7 | 19 | 39.6 | 1 | 5.3 | |
| Hit by object | 13 | 11.3 | 3 | 6.3 | 4 | 21.2 | |
| Bicycle accident | 14 | 12.2 | 3 | 6.3 | 5 | 26.3 | |
| Fall from height | 10 | 8.7 | 2 | 4.2 | 1 | 5.3 | |
| MVA | 8 | 7.0 | 8 | 16.7 | 1 | 5.3 | |
| Other | 2 | 1.7 | 0 | 1 | 5.3 | ||
| Type of fracture | <0.001 | ||||||
| Facial | 98 | 85.2 | 42 | 87.5 | 10 | 52.6 | |
| Cranial | 11 | 9.6 | 1 | 2.1 | 7 | 36.8 | |
| Cranio-facial | 6 | 5.2 | 5 | 10.4 | 2 | 10.5 | |
| Mortality | 0.027 | ||||||
| Yes | 2 | 1.7 | 0 | 2 | 10.5 | ||
| No | 113 | 98.3 | 48 | 100.0 | 17 | 89.5 | |
| Missed AI | 0.886 | ||||||
| Yes | 7 | 6.1 | 2 | 4.2 | 1 | 5.3 | |
| No | 108 | 93.9 | 46 | 95.8 | 18 | 94.7 | |
| yrs.: years; *: chi-square; other: under diagnosis of AI, improper instruction or medical treatment, impolite or un-professional behaviour; AI: associated injury; MVA: motor vehicle accident. | |||||||
Table 3 presents the associations between sex, age, mechanism, type of fracture, mortality, missed AI, and main outcome. Statistical significance did not emerge between any of these variables. However, the proportion of men was higher in patients with permanent harm (59.5%) than in the control group (50.7%). Permanent harm was clearly more frequent in patients aged 40–59 years than in any other age group. Assault (35.7%) and fall on ground (26.2%) were the most common cause of trauma in patients with permanent harm, and their injuries were mainly (90.5%) facial fractures. The rates of mortality (n = 2) and missed AI (n = 2) were even between the two groups.
| Study variables | Permanent harm | % | Permanent harm | % | P* |
| Present | Absent | ||||
| n = 42 | n = 140 | ||||
| Sex | 0.316 | ||||
| Male | 25 | 59.5 | 71 | 50.7 | |
| Female | 17 | 40.5 | 69 | 49.3 | |
| Age (yrs.) | |||||
| Range | 11–75 | 0–91 | |||
| Mean | 39.64 | 37.94 | |||
| Age group (yrs.) | 0.302 | ||||
| <18 | 7 | 16.7 | 27 | 19.3 | |
| 19–39 | 13 | 31.0 | 47 | 33.6 | |
| 40–59 | 20 | 47.6 | 48 | 34.3 | |
| 60+ | 2 | 4.8 | 18 | 12.9 | |
| Mechanism | 0.446 | ||||
| Fall on the ground | 11 | 26.2 | 51 | 36.4 | |
| Assault | 15 | 35.7 | 30 | 21.4 | |
| Hit by object | 6 | 14.3 | 14 | 10.0 | |
| Bicycle accident | 3 | 7.1 | 15 | 10.7 | |
| Fall from height | 3 | 7.1 | 14 | 10.0 | |
| MVA | 4 | 9.5 | 13 | 9.3 | |
| Other | 0 | 3 | 2.1 | ||
| Type of fracture | 0.148 | ||||
| Facial | 38 | 90.5 | 112 | 80.0 | |
| Cranial | 1 | 2.4 | 18 | 12.9 | |
| Cranio-facial | 3 | 7.1 | 10 | 7.1 | |
| Mortality | 0.196 | ||||
| Yes | 2 | 4.8 | 2 | 1.4 | |
| No | 40 | 95.2 | 138 | 98.6 | |
| Missed AI | 0.812 | ||||
| Yes | 2 | 4.8 | 8 | 5.7 | |
| No | 40 | 95.2 | 132 | 94.3 | |
| *: chi-square; AI: associated injury; yrs.: years; MVA: motor vehicle accident. | |||||
Table 4 shows the association between the cause of complaint and the presence of permanent harm. Delayed diagnosis or treatment (71.4%) was by far the most common cause of complaint in patients with permanent harm; however, their rate did not differ significantly from patients without permanent harm (60.7%, p = 0.299).
| Study variables | Permanent harm | % | Permanent harm | % | P* |
| Present | Absent | ||||
| n = 42 | n = 140 | ||||
| Cause of complaint | |||||
| Delay of correct diagnosis or treatment ± end result ± complication of fracture treatment |
30 | 26.1 | 85 | 73.9 | 0.299 |
| Complication of fracture or end result of treatment | 10 | 20.8 | 38 | 79.2 | |
| Other | 2 | 10.5 | 17 | 89.5 | |
| *: chi-square. | |||||
The frequency of solitary causes of complaint is presented in Figure 1. Delay of correct diagnosis was by far the most common cause of complaint (n = 107), followed by the end-result of treatment (n = 46), and complications of fracture treatment (n = 36). The cause of complaint could not be determined for three patients.
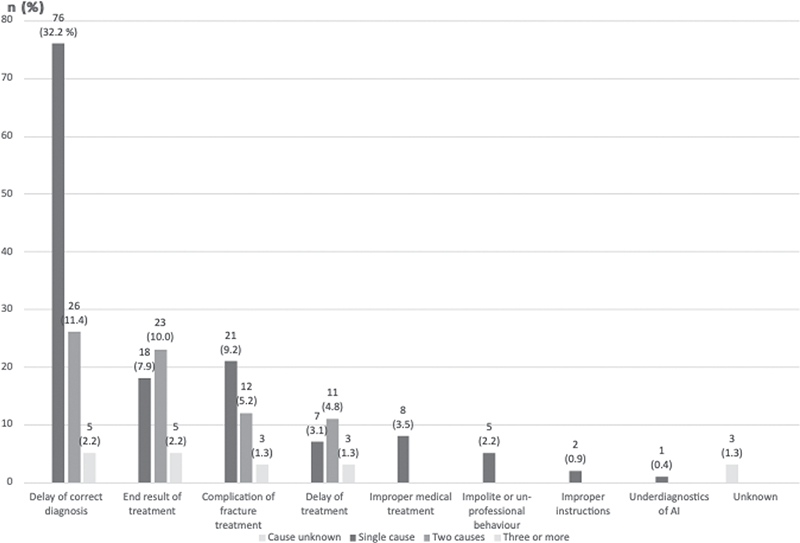
Figure 1. Number of individual causes of malpractice complaints.
Discussion
Publications focussing on facial and cranial trauma malpractice and complications are few. The purpose of this study was to investigate the demographics and causes leading to malpractice complaint in craniofacial fracture patients in Finland. We specifically aimed to clarify the reasons for complaints and whether permanent harm had occurred. The hypothesis was that fracture treatment-related complications are the leading group in major craniofacial injuries.
The hypothesis was rejected. The predominant cause of complaint in craniofacial fracture patients was delayed diagnosis or treatment with or without other complaint causes (63.2%). Delay-related complaints were more frequent in patients with permanent harm (71.4%) than in those without (60.7%), although the difference was not significant. Thus, in addition to the prevention of surgical complications, there is a marked need in the field of facial traumatology to improve the early diagnosis and initial care of these patients.
Fracture limited to the facial area was by far the most common fracture type (82.4%). Interestingly, regarding injury mechanisms, fall on ground (34.1%) and assault (24.7%) differed regarding the cause of complaint. Patients who had been assaulted complained more often of fracture complications and/or end-results, whereas patients sustaining ground level falls complained of delayed diagnosis and/or treatment (p < 0.026).
An injury or its treatment can negatively impact a patient’s social encounters, mental health, and ability to work, thus lowering their quality of life [14–17]. Ji et al. [18] concluded that up to 34.6% of all patients undergoing a maxillofacial procedure sustain at least minor permanent harm, with the rate of death being up to 5.3%. Our study revealed that 23.1% of craniofacial fracture patients suffered permanent harm, 4.8% of these patients having undiagnosed AI and 2.2% dying from their injuries. Thus, the rates of malpractice complaints of craniofacial fracture patients are clearly lower than those of maxillofacial surgery patients in general.
Permanent harm was most typically found in middle-aged (47.6%) males (59.5%) sustaining their injuries from interpersonal violence (35.7%). In the literature, a fracture of the zygomatico-orbital complex has been the most typical facial fracture type in these patients. The occurrence of this fracture type was high in the 1980s and the 1990s (42.0% for both) [19], falling at the beginning of the 21st century (38.3%) [20]. The complications reported in the literature, for example, in orbital blow-out fractures have been diplopia, infraorbital nerve injury, and esthetics which are fortunately often transient but affect the quality of life severely [21]. One of the factors proven to diminish long-lasting neurosensory disturbance has been short delay (<1 week) to surgical intervention when surgery is clinically indicated [22].
Indeed, the current study revealed that a delay-related cause was by far the most common cause of malpractice complaint (63.2%), compared with other causes. The result of previous publications on facial trauma complaints (1.9–34.8%) were clearly different [13, 18]. One explanation for the discrepancy may be different legal processes; for example, the study by Ji et al. examined material including claims settled before court and at court [18], whereas the Finnish malpractice complaint process is an assisted process with a low contact threshold, not court-related, and even the suspicion of a treatment-related harm is evaluated. The diagnostic delay can have contributory factors such as trauma scene, geographical location, influence of alcohol or other intoxicant substances, and arrestment which can affect to the time span from injury to correct diagnosis and treatment path [23, 24]. In addition to the previous, literature has shown that 8.8% of medical mistakes are related to the event of negligence [7], which should not be involved in medical care.
Under-diagnostics and under-triage are well-known problems. For example, the rate of under-diagnostics of geriatric general trauma varies from 15.0 to 69.1% under the primary trauma triage [25–28]. In relation to facial fracture diagnostics, Kannari et al. [29] stated that up to 20.1% of patients at least 60 years of age do not receive correct fracture diagnosis under primary evaluation after the injury. In the present study, 63.1% of patients with a mean age of 36.81 years made a complaint related to diagnostic delay. Ugboko [23] reported a complication rate of 22.9% combined with a primary contact within the first 7-day period from injury for 83.4% of the study population, whereas the more recent results of Stanford-Moore [24] reveal that 81.0% of complications were found after a delay of 3 days from injury. The delay in diagnosis can lead to functional deficiencies, increased risk of infection, malunion, and unnecessary pain [23]. Proper education for facial injury diagnostics, meticulous repeated status, and low-threshold facial traumatologist consultation are recommended to avoid under-diagnostics of facial fractures in middle-aged patients also.
The main strength of this study was coverage of both private and public sector complaints over a 20-year period in Finland. Our study highlights fracture diagnostics as the primary cause of complaints.
A limitation of the study is its retrospective nature: Firstly, a prospective study would have given more detailed information on solitary complications. Secondly, the study compares the malpractice claims to the site of facial trauma (upper, middle, and lower facial third), whereas the specific type of facial fracture would have given even more information.
In conclusion, our hypothesis of fracture treatment-related complaints being the leading cause of malpractice claims was rejected. Low-threshold facial traumatologist consultation is recommended to establish appropriate diagnosis of facial fracture, to prevent harmful delay in diagnostics and fracture treatment, and to avoid under-diagnostics and permanent harm also in middle-aged men suspected of having a craniofacial fracture.
References
[1] Austin EE, Do V, Nullwala R, et al. Systematic review of the factors and the key indicators that identify doctors at risk of complaints, malpractice claims or impaired performance. BMJ Open. 2021 Aug 24;11(8):e050377. https://doi.org/10.1136/bmjopen-2021-050377.
[2] Anupam BJ, Seabury S, Lakdawalla D, et al. Malpractice risk according to physician specialty. N Engl J Med. 2011 August 18;365(7):629–636. https://doi.org/10.1056/NEJMsa1012370.
[3] Tibble HM, Broughton NS, Studdert DM, et al. Why do surgeons receive more complaints than their physician peers? ANZ J Surg. 2018;88:269–273. https://doi.org/10.1111/ans.14225.
[4] Hanganu B, Iorga M, Muraru I-D, et al. Reasons for and facilitating factors of medical malpractice complaints. What can be done to prevent them? Medicina (Kaunas). 2020 May 27;56(6):259. https://doi.org/10.3390/medicina56060259.
[5] Gil LF, Granato R, Marin C, et al. Assessment of complaints and their relationship with facial profiles in patients undergoing orthognathic surgery. Int J Oral Maxillofac Surg. 2011;40(10):1085–1085. https://doi.org/10.1016/j.ijom.2011.07.201.
[6] Green MA, Resnick CM, Mercuri LG. Characteristics of medical malpractice claims involving temporomandibular joint surgery in the United States 2022. J Oral Maxillofac Surg. 2022 Jul;80(7):1153–1157. https://doi.org/10.1016/j.joms.2022.04.003.
[7] De Brauwer F, Bertolus C, Goudot P, et al. Chaine causes for litigation and risk management in facial surgery: a review of 136 cases. J Stomatol Oral Maxillofac Surg. 2019 Jun;120(3):211–215. https://doi.org/10.1016/j.jormas.2018.12.003.
[8] Bordonaba-Leiva S, Gómez-Durán EL, Balibrea JM, et al. Twenty four years of oral and maxillofacial surgery malpractice claims in SpaIn: patient safety lessons to learn. Oral Maxillofac Surg. 2019 Jun;23(2):187–192. https://doi.org/10.1007/s10006-019-00756-3.
[9] Pauli N, Grinups M, Folkestad L, et al. Patient-reported symptoms after midfacial trauma. Surg J (NY). 2022 Jan 17;8(1):e22–e27. https://doi.org/10.1055/s-0041-1742174.
[10] Morris LM, Kellman M. Complications in facial trauma. Facial Plast Surg Clin N Am. 2013;21:605–617. https://doi.org/10.1016/j.fsc.2013.07.005.
[11] Bonitz L, Wruck V, Peretti E, et al. Long-term evaluation of treatment protocols for isolated midfacial fractures in a German nation-wide craniomaxillofacial trauma center 2007–2017. Sci Rep. 2021 Sep 14;11(1):18291. https://doi.org/10.1038/s41598-021-97858-4.
[12] Gulati A, Herd MK, Nimako M, et al. Litigation in National Health Service oral and maxillofacial surgery: review of the last 15 years. Br J Oral Maxillofac Surg. 2012 Jul;50(5):385–388. https://doi.org/10.1016/j.bjoms.2011.06.003.
[13] Mozeika AM, Sachdev D, Asri R, et al. Sociological and medical factors influence outcomes in facial trauma malpractice. J Oral Maxillofac Surg. 2019 May;77(5):1042.e1–1042.e10. https://doi.org/10.1016/j.joms.2019.01.005.
[14] Ukbong DI, Ugboko VI, Ndukwe KC, et al. Health-related quality of life in Nigerian patients with facial trauma and controls: a preliminary survey. Br J Oral Maxillofac Surg. 2008 June;46(1):297–300. https://doi.org/10.1016/j.bjoms.2007.09.013.
[15] Piper JP, Barreto Rocha DF, Hayes DS, Grandizio LC. Formal patient complaints and malpractice events against pediatric orthopaedic surgeons. J Pediatric Orthop. 2021;41:e585–e589. https://doi.org/10.1097/BPO.0000000000001840.
[16] Conforte JJ, Alves CP, Sanchez MDPR, et al. Impact of trauma and surgical treatment on the quality of life of patients with facial fractures. Int J Oral Maxillofac Surg. 2016 May;45(5):575–581. https://doi.org/10.1016/j.ijom.2015.11.022.
[17] Ahmed A, McGoldrick DM, Elledge R. Clinical negligence claims in oral and maxillofacial surgery over the last 10 years. Br J Oral Maxillofacial Surg. 2021 Dec;59(10):1259–1263. https://doi.org/10.1016/j.bjoms.2021.05.012.
[18] Ji YD, Peacock ZS, Resnick CM. Characteristics of national malpractice claims in oral and maxillofacial surgery. J Oral Maxillofac Surg. 2020 Aug;78(8):1314–1318. https://doi.org/10.1016/j.joms.2020.03.015.
[19] Kontio R, Suuronen R, Ponkkonen H, et al. Have the causes of maxillofacial fractures changed over the last 16 years in Finland? An epidemiological study of 725 fractures. Dent Traumatol. 2005;21(1):14–19. https://doi.org/10.1111/j.1600-9657.2004.00262.x.
[20] Toivari M, Helenius M, Suominen AL, et al. Etiology of facial fractures in elderly Finns during 2006–2007. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014 Nov;118(5):539–45. https://doi.org/10.1016/j.oooo.2014.06.016.
[21] Rajantie H, Kaukola L, Snäll J, et al. Health-related quality of life in patients surgically treated for orbital blow-out fracture: a prospective study. Oral Maxillofacial Surg. 2021 Sep;25(3):373–382. https://doi.org/10.1007/s10006-020-00923-x.
[22] Haapanen A, Thorén H, Apajalahti S, et al. Neurosensory recovery after trauma to the orbital floor: a prospective trial with dexamethasone. Br J Oral Maxillofac Surg. Nov;56(9):810–813. https://doi.org/10.1016/j.bjoms.2018.08.017.
[23] Ugboko VI, Odusanya SA, Fagade VI. Maxillofacial fractures in a semi-urban Nigerian teaching hospital. A review of 442 cases. Int J Oral Maxillofac Surg. 1998 Aug;27(4):286–289. https://doi.org/10.1016/S0901-5027(05)80616-2.
[24] Stanford-Moore GB, Niyigaba G, Tuyishimire G, et al. Effect of delay of care for patients with craniomaxillofacial trauma in Rwanda. OTO Open. 2022 Apr 22;6(2):2473974X221096032. https://doi.org/10.1177/2473974X221096032.
[25] Hung KK, Yeung JHH, Cheung CSK, et al. Trauma team activation criteria and outcomes of geriatric trauma: 10 year single centre cohort study. Am J Emerg Med. 2019;37(3):450–456. https://doi.org/10.1016/j.ajem.2018.06.011.
[26] Garwe T, Stewart K, Stoner J, et al. Out-of-hospital and inter-hospital under-triage to designated tertiary trauma centers among injured older adults: a 10-year statewide geospatial-adjusted analysis. Prehosp Emerg Care. 2017 Nov–Dec;21(6):734–743. https://doi.org/10.1080/10903127.2017.1332123.
[27] Harvey LA, Close JC. Traumatic brain injury in older adults: characteristics, causes and consequences. Injury. 2012;43(11):1821–1826.https://doi.org/10.1016/j.injury.2012.07.188.
[28] Rogers A, Rogers F, Bradburn E, et al. Old and undertriaged: a lethal combination. Am Surg. 2012;78(6):711–715. https://doi.org/10.1177/000313481207800628.
[29] Kannari L, Marttila E, Toivari M, et al. Paediatric mandibular fracture – a diagnostic challenge? Int J Oral Maxillofac Surg. 2020 Nov;49(11):1439–1444. https://doi.org/10.1016/j.ijom.2020.06.008.