LETTER
Childhood cancer incidence and survival in the Faroe Islands, 1960 to 2019
Marnar Fríðheim Kristiansena,b,c , Elmar Ósáa, Lisa Lyngsie Hjalgrimd
, Elmar Ósáa, Lisa Lyngsie Hjalgrimd , Bjarni á Steiga,b, Guðrið Andórsdóttirb, Marin Strøm*c,e
, Bjarni á Steiga,b, Guðrið Andórsdóttirb, Marin Strøm*c,e and Maria Skaalum Petersen*c,f
and Maria Skaalum Petersen*c,f
aMedical Department, National Hospital of the Faroe Islands, J.C. Svabosgøta 41–49, Tórshavn, Faroe Islands; bGenetic Biobank of the Faroe Islands, Eirargarður 2, Tórshavn, Faroe Islands; cCentre of Health Sciences, University of the Faroe Islands, Vestara Bryggja 15, Tórshavn, Faroe Islands; dDepartment of Paediatrics and Adolescent Medicine, Juliane Marie Centre, Blegdamsvej 9, Copenhagen, Denmark; eDepartment of Epidemiology Research, Statens Serum Institut, Artillerivej 5, Copenhagen S, Denmark; fDepartment of Occupational Medicine and Public Health, The Faroese Hospital System, Sigmundargøta 5, Tórshavn, Faroe Islands
ABSTRACT
Background and purpose: This study is the first report regarding childhood cancer in the Faroe Islands and describes the incidence and survival of childhood cancer over the last 60 years in the Faroe Islands.
Material and methods: We included all Faroese children registered with a cancer diagnosis up to the age of 19 years in the Faroese Cancer Registry from 1960 to 2019 and in the Danish Childhood Cancer Registry from 1985 to 2019 in this study. We report the number of incident cancers classified according to the 12 main diagnostic groups in the International Classification of Childhood Cancer, third edition (ICCC-3), but due to small numbers some groups have been combined in the results shown. We report age-standardized incidence rates (world standard population) (ASIR). We also show all-cause survival by incidence stratified by 20-year periods.
Results: There were 114 childhood cancers in the Faroe Islands from 1960 to 2019, corresponding to an ASIR of 13.0 per 100,000 person-years. The most common cancer groups in Faroese children were brain and spinal tumors, followed by leukemias and lymphomas. All-cause survival improved for children diagnosed over time, with a 5-year survival of 43.5% for those diagnosed from 1960 to 1979 and 85.6% for children diagnosed from 2000 to 2019.
Conclusion: Childhood cancer in the Faroes was slightly rarer than in most other high-income countries. Brain and spinal tumors were the most common cancer group in Faroese children. Survival for Faroese children with cancer has improved substantially in the study period.
KEYWORDS: Cancer; childhood cancer; Faroe Islands; incidence; survival; epidemiology
Citation: ACTA ONCOLOGICA 2024, VOL. 63, 4–8. https://doi.org/10.2340/1651-226X.2024.27110.
Copyright: © 2024 The Author(s). Published by MJS Publishing on behalf of Acta Oncologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material, with the condition of proper attribution to the original work.
Received: 19 November 2023; Accepted: 20 November 2023; Published: 8 February 2024
CONTACT Marnar Fríðheim Kristiansen marfr@ls.fo The Faroese Cancer Registry, National Hospital of the Faroe Islands, J.C. Svabosgøta 41–49, Tórshavn, Faroe Islands
*Shared last author.
Competing interests and funding: The authors report there are no competing interests to declare.
This work was supported by the Research Council Faroe Islands under Grant [project 3025] and the Team Rynkeby Foundation under the Faroese Cancer Society [no grant number] and Brødrene Hartmans Fond under Grant [A33933] and Dansk Kræftforskningsfond under Grant [DKF-2019–50 – (352)] and the Danish Cancer Society under Grant [R293-A16833].
Introduction
Childhood cancers are rare, potentially life-threatening diseases with far-reaching consequences for the child and the family affected. Treatment for childhood cancer has improved substantially over the last 50 years [1]. Some cancers that previously had a very low survival have seen marked improvements, which means that today, the vast majority of children diagnosed with cancer will survive [2].
The Faroe Islands are a group of 18 islands in the Atlantic Ocean. The population consists of 53,882 individuals, of which 14,822 are below the age of 20 (2022). The Faroe Islands are a high-income country with a modern healthcare system [3]. However, for childhood cancers, the treatment is delivered in Denmark due to the need for highly specialized treatment, which is impossible to manage locally with approximately two incident cases per year.
Treatment for childhood cancer varies, with detailed protocols for each different type of cancer. The most common treatments are chemotherapy, and surgery while other options for some cancer types include irradiation and bone marrow transplants [1, 4].
All Faroese children with suspected cancer are sent to Denmark for specific diagnosis and treatment when relevant. Upon verification of the diagnosis, the children undergo an often lengthy stay in Denmark to receive the treatment needed, ranging from a couple of weeks for low-grade tumors removed surgically over 3 to 6 months for lymphoma up to 2.5 years for acute lymphatic leukemia (ALL). In some cases, patients can receive parts of the follow-up treatment in the Faroe Islands, mainly for children who undergo the 2.5 years regime for ALL.
For the first time in the Faroe Islands, we report on the incidence and survival of childhood cancer in Faroese children up to the age of 19 from 1960 to 2020, filling a gap in research about children in the Faroe Islands.
Methods and materials
All cancers in the Faroe Islands are registered in the Faroese Cancer Registry (FCR) [3]. Here, we include all individuals diagnosed with cancer up to the age of 19 in the FCR. However, as all treatment and diagnosis of childhood cancers are performed in Denmark, some cancers might not be registered in the FCR. Therefore, we also included Faroese children reported to the Danish Childhood Cancer Registry (DCCR) [5]. We used billing information present in the Faroese Hospital system to link the Faroese personal identifier with the one used in the danish medical journal.
We classified the cancers according to the 12 main diagnostic groups in the International Classification of Childhood Cancer, third edition (ICCC-3) [6], which are the following: leukemias, lymphomas, brain and spinal tumors, neuroblastoma, retinoblastoma, kidney tumors, liver tumors, bone tumors, soft tissue sarcomas, germ cell tumors, other carcinomas and melanomas, and other. Due to small numbers, we combined the following diagnostic groups in the results shown: neuroblastomas and retinoblastomas, kidney tumors and liver tumors, and bone tumors and soft tissue sarcomas.
We calculated age-standardized incidence rates (ASIR) using the World standard weights stratified by 10-year periods, 1960 to 1969, 1970 to 1979, 1980 to 1989, 1990 to 1999, 2000 to 2009, and 2010 to 2019. We furthermore compared the Faroese incidence specifically for the two largest cancer groups (leukemias and brain and spinal tumors) to the incidence in Sweden, by calculating the incidence rate ratio (IRR) with corresponding 95% confidence intervals for the age group 0–19 years. We chose to compare with Sweden, as all of the needed numbers were readily available for the period 1984–2010 for the age group 0–19 years in the appendix for a report published by the Swedish Childhood Cancer Registry [7].
We used R version 4.02 to produce the graphs and the R package Survminer version 0.4.9 [8] to produce Kaplan Meier estimates for all-cause survival for all cancers. For the survival analysis, we grouped patients by the time of diagnosis, 1960 to 1979, 1980 to 1999, and 2000 to 2019, and we excluded cases with a follow-up time of 0 days (n = 4 for 1960–1979; n = 10 for 1980–1999; n = 3 for 2000–2019).
The use of cancer registry data for this project was approved by the Faroese Data Protection Authority (J.nr: 19/00027-4).
Results
Over the last 60 years, 114 Faroese children have been diagnosed with cancer, 50 girls and 64 boys (Figure 1). This corresponds to about two children diagnosed with cancer every year and an ASIR for cancer of any type of 13.0 per 100,000 person-years (pyrs) for the whole period. We identified 28 cases from the DCCR in the period 1985 to 2019, two of which were not registered previously in the FCR. Within the same period and age group (up to 19), there were 70 childhood cancers reported in the FCR. The cancer incidence for boys and girls at different periods and age groups is shown in Table 1. The most common cancer type was brain and spinal tumors, with an ASIR of 3.9 per 100,000 pyrs, followed by leukemias with an ASIR of 2.3 per 100,000 pyrs. Comparing the most common cancer types with the incidence in Sweden from 1984 to 2010, we calculated the IRR of leukemias at 0.52 (95% CI 0.33–0.82) while the IRR of brain and spinal tumors was 1.00 (95% CI 0.71–1.40).
| Cases (N) | Crude rate per 100,000 | ASIR per 100,000 (W)* | |||
| Overall | 114 | 12.66 | 13.03 | ||
| Girls | 50 | 11.48 | 11.94 | ||
| Boys | 64 | 13.76 | 14.04 | ||
| Time period | |||||
| 1960–1969 | 12 | 8.00 | 7.99 | ||
| 1970–1979 | 20 | 12.47 | 12.97 | ||
| 1980–1989 | 23 | 14.45 | 14.28 | ||
| 1990–1999 | 27 | 18.59 | 19.45 | ||
| 2000–2009 | 17 | 11.64 | 11.36 | ||
| 2010–2019 | 15 | 10.71 | 12.23 | ||
| Age group | |||||
| 0–4 year | 40 | 17.86 | 5.36 | ||
| 5–9 years | 24 | 10.63 | 2.66 | ||
| 10–14 years | 20 | 8.68 | 1.95 | ||
| 15–19 years | 30 | 13.59 | 3.06 | ||
| Main diagnostic group I. Leukemias | 19 | 2.11 | 2.25 | ||
| II. Lymphomas | 15 | 1.67 | 1.66 | ||
| III. Brain and spinal tumors | 34 | 3.77 | 3.93 | ||
| IV. and V. Neuroblastomas and Retinoblastomas ** | 7 | 0.77 | 0.94 | ||
| VI. and VII. Kidney tumors and Liver tumors ** | 4 | 0.44 | 0.51 | ||
| VIII. and IX. Bone tumors and Soft tissue sarcomas ** | 8 | 0.88 | 0.90 | ||
| X. Germ cell tumors | 11 | 1.22 | 1.15 | ||
| XI. Other carcinomas and melanomas | 9 | 1.00 | 0.95 | ||
| XII. Other | 7 | 0.78 | 0.74 | ||
| Comparison ASIR | Both sexes | Girls | Boys | Period | Ages |
| Faroe Islands | 13.03 | 11.94 | 14.04 | 1960–2019 | 0–19 |
| Denmark [10] | 17.68 | 16.07 | 19.22 | 1977–2014 | 0–19 |
| Iceland [11] | 14.5 | 12.8 | 16.1 | 1981–2006 | 0–18 |
| Sweden [7] | 15.99 | 14.98 | 16.95 | 1984–2010 | 0–14 |
| 62 countries – The Lancet [9] | 15.58 | 14.36 | 16.32 | 2001–2010 | 0–19 |
| *Age standardized incidence rate per 100,000 using the world standard weights; **Groups have been combined due to small numbers. ASIR: age-standardized incidence rates. | |||||
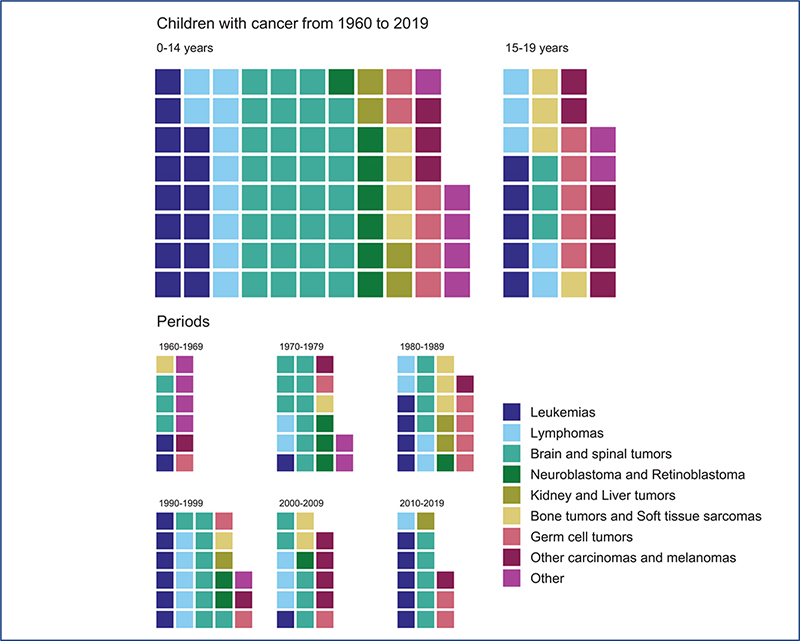
Figure 1. Childhood cancer (≤19 years) in the Faroe Islands from 1960 to 2019 by ICCC-3 main diagnostic group.
Waffle plots showing the distribution of ICCC-3 main diagnostic groups in children diagnosed with cancer in the Faroe Islands. Due to small numbers some groups have been combined. Each square represents one cancer case. The upper panel shows the distribution of cancers in girls and boys by children aged 0–14 and 15–19 diagnosed from 1960 to 2019. The lower panel shows the distribution of cancers in both girls and boys for each 10-year period from 1960 to 2019. ICCC-3: International Classification of Childhood Cancer, third edition.
All-cause survival has improved over the years, with 1-year survival improving from 65.2% from 1960 to 1979 up to 90.3% from 2000 to 2019. Five-year survival improved from 43.5% to 86.7% in the same period (Figure 2).
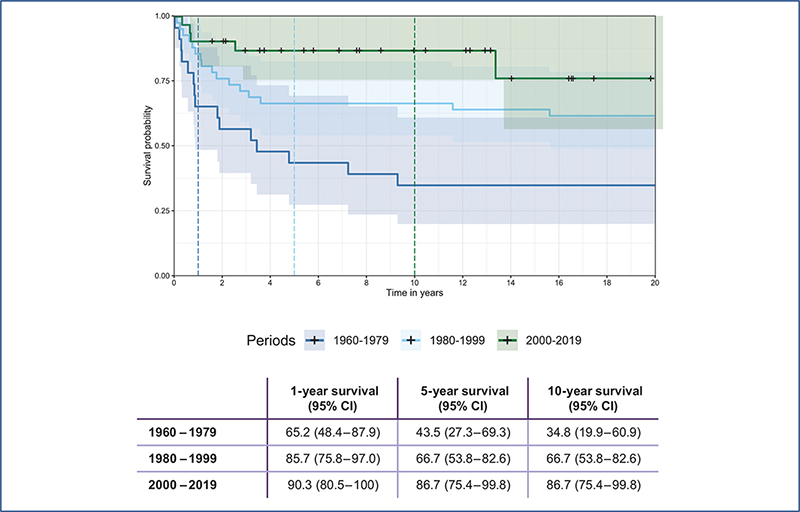
Figure 2. All-cause survival by period in Faroese children with cancer.
Kaplan Meier plot showing all-cause survival for Faroese children diagnosed with cancer, stratified by 20-year periods for the time of diagnosis. We excluded children who had a follow-up time of 0 days from the survival analysis (n = 4 for 1960–1979; n = 10 for 1980–1999; n = 3 for 2000–2019). The vertical lines in the graph represent 1-, 5- and 10-year survival, with the corresponding values shown below the graph.
Discussion
Over the last 60 years, just under two Faroese children have received a cancer diagnosis each year on average. Leukemias are the most common childhood cancer group worldwide, followed by brain and spinal tumors and lymphomas [4, 9]. However, this differed slightly for Faroese children, with the most common diagnostic group being brain and spinal tumors, followed by leukemias and lymphomas. The incidence of leukemias was almost half of the incidence in Sweden with an IRR of 0.52, while the incidence of brain and spinal tumors was very similar with an IRR of 1.00.
In a study published in The Lancet Oncology in 2017 [9], the authors compared ASIR from 152 registries in 62 different countries from 2001 to 2010. The ASIR for all cancers for children ≤19 years in The Lancet study ranged from 8.7 per 100,000 pyrs in India to 19.2 per 100,000 pyrs in Southern Europe. The combined dataset showed an overall ASIR of 15.6 per 100,000 pyrs. The ASIR in the Faroe Islands for the same period was 11.6 per 100,000 pyrs, while it was 13.0 per 100,000 pyrs for the whole study period. In a study by Grabas et al. [10], childhood cancer incidence in Denmark showed an ASIR of 17.7 per 100,000 pyrs for the years 1977 to 2014, whereas Óskarsson et al. reported an ASIR for childhood cancer up to the age of 18 in Iceland of 14.5 per 100,000 pyrs [11]. In a report from 2013 in Sweden, the ASIR was 16.0 per 100,000 pyrs in the period 1984 to 2010, but in this case the age group was from 0 to 14 years [7]. Overall, childhood cancer appears to be slightly rarer in the Faroe Islands than in in countries the Faroe Islands are often compared to as seen in table 1. [10].
Established risk factors for the development of childhood cancers are scarce. Lifestyle factors that cause a high proportion of adult cancers do not generally cause childhood cancer [12]. Some of the known risk factors for childhood cancer are affected fetal growth [13], genetics [14], and parental exposures [15]. Some of the differences observed between countries are expected to be caused by different access to diagnostic tools required for diagnoses such as brain and spinal tumors [16], leading to a lower likelihood of receiving a cancer diagnosis. However, we find underdiagnosing an unlikely explanation for the slightly lower incidence observed in the Faroe Islands due to the generally high standard of health care and free access to health care. There might be a risk that some childhood cancers would not have been registered in the FCR since all children are sent abroad for treatment and diagnosis. We obtained data from the DCCR to address this potential limitation, where all Faroese children diagnosed after 1985 are expected to be registered.
Worldwide, survival for childhood cancer has improved considerably over time as treatments have improved. Acute lymphatic leukemia is one example of a cancer diagnosis where 5-year survival was below 10% in the 1960s and has increased to above 90% in some countries today [2]. The number of cases in the Faroe Islands is low, complicating any meaningful stratification by the type of cancer. Therefore, we grouped all childhood cancers for survival calculations and observed a markedly improved all-cause survival over time.
Even though survival has improved, survivors may experience a wide range of long-term effects after a childhood cancer diagnosis [16, 17]. These long-term effects vary by cancer type but include secondary cancers [17, 18], increased risk of diabetes [19], lung and cardiac effects [17] as well as affected fertility [17, 20]. Research within this area is scarce in the Faroe Islands and is warranted.
A cancer diagnosis is a significant burden for any child and their family [21–24]. This burden might be exacerbated for Faroese families because the treatment is only given abroad. The family must deal with a severe medical diagnosis in their child in addition to either separating the family or moving the whole family to a new country.
The low number of cases in our data limits the certainty of any conclusion we can reach in this report. However, we believe that the national and lengthy coverage provides a robust evaluation of the childhood cancer rate in the Faroe Islands over time.
Childhood cancers are rare, and treatment advances mean that most children with cancer will survive. Research into the long-term somatic and socioeconomic effects of childhood cancer among survivors in the Faroe Islands should be considered.
Data availability statement
The data supporting this study’s findings are available from the corresponding author, Marnar Fríðheim Kristiansen, upon reasonable request and appropriate approvals.
Acknowledgments
We are grateful to the Danish Childhood Cancer Registry for providing access to data about the Faroese children.
References
[1] Erdmann F, Frederiksen LE, Bonaventure A, et al. Childhood cancer: survival, treatment modalities, late effects and improvements over time. Cancer Epidemiol. 2021;71:101733. https://doi.org/10.1016/j.canep.2020.101733
[2] Cools J. Improvements in the survival of children and adolescents with acute lymphoblastic leukemia. Haematologica. 2012;97:635. https://doi.org/10.3324/haematol.2012.068361
[3] Kristiansen M, Mikkelsen RM, Kristiansdóttir T, et al. Cancer in the Faroe Islands from 1960–2019 – incidence, mortality, and comparisons with the other Nordic countries. Acta Oncol. 2022;61(8):907–15. https://doi.org/10.1080/0284186X.2022.2082885
[4] Kaatsch P. Epidemiology of childhood cancer. Cancer Treat Rev. 2010;36:277–85. https://doi.org/10.1016/j.ctrv.2010.02.003
[5] Schrøder H, Rechnitzer C, Wehner PS, et al. Danish childhood cancer registry. Clin Epidemiol. 2016;8:461–4. https://doi.org/10.2147/CLEP.S99508
[6] Steliarova-Foucher E, Stiller C, Lacour B, et al. International classification of childhood cancer, third edition. Cancer. 2005;103:1457–67. https://doi.org/10.1002/cncr.20910
[7] Gustafsson G, Kogner P, Heyman M. Childhood cancer incidence and survival in from the Swedish Childhood Cancer Registry [Internet]. 2013 [cited 10-05-2022]. Available from: http://www.forskasverige.se/wp-content/uploads/ChildhoodCancerIncidenceandSurvivalinSweden1984_2010.pdf
[8] Kassambara A, Kosinski M, Biecek P. survminer: drawing survival curves using ‘ggplot2’ [Internet]. 2021. Available from: https://cran.r-project.org/package=survminer [cited 2021-11-01]
[9] Steliarova-Foucher E, Colombet M, Ries LAG, et al. International incidence of childhood cancer, 2001–10: a population-based registry study. Lancet Oncol. 2017;18:719–31. https://doi.org/10.1016/S1470-2045(17)30186-9
[10] Grabas MR, Kjaer SK, Frederiksen MH, et al. Incidence and time trends of childhood cancer in Denmark, 1943–2014. Acta Oncol. 2020;59:588–95. https://doi.org/10.1080/0284186X.2020.1725239
[11] Oskarsson T, Jonsson OG, Kristinsson JR, et al. [Childhood cancer in Iceland 1981–2006]. Laeknabladid. 2010;96:21–6. https://doi.org/10.17992/lbl.2010.01.04
[12] American Cancer Society. Risk factors and causes of childhood cancer [Internet]. 2019 [cited 10-05-2022]. Available from: https://www.cancer.org/content/dam/CRC/PDF/Public/9180.00.pdf
[13] Bjørge T, Sørensen HT, Grotmol T, et al. Fetal growth and childhood cancer: a population-based study. Pediatrics. 2013;132:e1265–75. https://doi.org/10.1542/peds.2013-1317
[14] Robin NH, Hurst ACE. Chapter 2. The genetic evaluation of a child with cancer. Editor(s): Nathaniel H. Robin, Meagan B. Farmer, Pediatric Cancer Genetics, Elsevier, 2018, Pages 21-31, ISBN 9780323485555, https://doi.org/10.1016/B978-0-323-48555-5.00002-8.
[15] Schüz J, Erdmann F. Environmental exposure and risk of childhood leukemia: an overview. Arch Med Res. 2016;47:607–14. https://doi.org/10.1016/j.arcmed.2016.11.017
[16] WHO Regional Office for Europe. Childhood cancer inequalities in the WHO European Region [Internet]. 2022 [cited 10-05-2022]. Available from: https://apps.who.int/iris/bitstream/handle/10665/351857/9789289057615-eng.pdf?sequence=2&isAllowed=y
[17] Landier W, Armenian S, Bhatia S. Late effects of childhood cancer and its treatment. Pediatr Clin North Am. 2015;62:275–300. https://doi.org/10.1016/j.pcl.2014.09.017
[18] Olsen JH, Möller T, Anderson H, et al. Lifelong cancer incidence in 47 697 patients treated for childhood cancer in the Nordic countries. J Natl Cancer Inst. 2009;101:806–13. https://doi.org/10.1093/jnci/djp104
[19] Holmqvist AS, Olsen JH, Andersen KK, et al. Adult life after childhood cancer in scandinavia: diabetes mellitus following treatment for cancer in childhood. Eur J Cancer. 2014;50:1169–75. https://doi.org/10.1016/j.ejca.2014.01.014
[20] Green DM, Kawashima T, Stovall M, et al. Fertility of male survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2010;28:332–9. https://doi.org/10.1200/JCO.2009.24.9037
[21] Mader L, Hargreave M, Frederiksen LE, et al. The impact of childhood cancer on parental separation, divorce, and family planning in Denmark. Cancer. 2020;126:3330–40. https://doi.org/10.1002/cncr.32901
[22] Mader L, Hargreave M, Bidstrup PE, et al. The impact of childhood cancer on parental working status and income in Denmark: patterns over time and determinants of adverse changes. Int J Cancer. 2020;147:1006–17. https://doi.org/10.1002/ijc.32867
[23] Gerhardt CA, Salley CG, Lehmann V. The impact of pediatric cancer on the family BT. In: Abrams AN, Muriel AC, Wiener L, eds. Pediatric psychosocial oncology: textbook for multidisciplinary care. Cham: Springer International Publishing, 2016: pp. 143–55. https://doi.org/10.1007/978-3-319-21374-3_9
[24] Erker C, Yan K, Zhang L, et al. Impact of pediatric cancer on family relationships. Cancer Med. 2018;7:1680–8. https://doi.org/10.1002/cam4.1393