ORIGINAL ARTICLE
Exploring how attachment insecurities mediate the link between sexual and partnership satisfaction in adolescents and young adults with cancer
Svenja Heynea,b, Hannah Brocka,b , Diana Richtera,b
, Diana Richtera,b , Annekathrin Sendera,b
, Annekathrin Sendera,b , Jenny Rosendahlc
, Jenny Rosendahlc , Michael Friedricha,b
, Michael Friedricha,b , Kristina Geued**
, Kristina Geued** , and Anja Mehnert-Theuerkaufa,b**
, and Anja Mehnert-Theuerkaufa,b**
aDepartment of Medical Psychology and Medical Sociology, University Medical Center Leipzig, Leipzig, Germany; bComprehensive Cancer Center Central Germany (CCCG), Leipzig, Germany; cInstitute of Psychosocial Medicine, Psychotherapy and Psychooncology, Jena University Hospital, Jena, Germany; dUniversity Clinic for Psychosomatic Medicine and Psychotherapy, University Medical Center Magdeburg, Magdeburg, Germany
ABSTRACT
Background and purpose: Comprehensive data on factors affecting partnership satisfaction among adolescents and young adult (AYA) cancer survivors are limited. Our study examines partnership satisfaction, sexual satisfaction, and attachment insecurities, exploring how attachment-related anxiety and avoidance influence the relationship between sexual and partnership satisfaction across major tumor entities in this population.
Patients and methods: We utilized data from two measurement time points (t1 and t6) of the AYA-LE study, a prospective longitudinal investigation examining the temporal course and associated factors of life satisfaction and psychological distress among AYA cancer survivors. We examined the mediating effect of attachment insecurities (ECR-RD) on the relationship between sexual satisfaction (FLZ-Sex) and partnership satisfaction (PFB), while controlling for sociodemographic and clinical characteristics, in a sample of N = 275 participants.
Results: Higher sexual satisfaction was correlated with lower attachment-related anxiety (r = -0.51, p < 0.001) and lower attachment-related avoidance (r = -0.49, p < 0.001). Both lower attachment-related anxiety and attachment-related avoidance were correlated with higher partnership satisfaction (r = -0.64, p < 0.001 and r = -0.72, p < 0.001, respectively). Sexual satisfaction partially predicted partnership satisfaction of AYA cancer survivors through attachment-related anxiety and attachment-related avoidance while the mediating effect accounted for 75% of the total effect.
Interpretation: The associations between sexual satisfaction, partnership satisfaction, and attachment highlight the need to address emotional and relational aspects in supportive care for AYA cancer survivors. There is a clear need for more targeted studies on attachment patterns, sexual satisfaction, and partnership satisfaction in this specific population to further refine and validate these approaches.
KEYWORDS: Sexual health; attachmentrelated anxiety; attachment-related avoidance; AYA cancer survivors; oncology; supportive care
Citation: ACTA ONCOLOGICA 2025, VOL. 64, 96–104. https://doi.org/10.2340/1651-226X.2025.42110.
Copyright: © 2025 The Author(s). Published by MJS Publishing on behalf of Acta Oncologica. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/).
Received: 27 September 2024; Accepted: 8 January 2025; Published: 21 January 2025
CONTACT Svenja Heyne svenja.heyne@medizin.uni-leipzig.de Philipp-Rosenthal-Str. 55, 04103 Leipzig, Germany
**KG and AMT are Joint Senior Authors.
Competing interests and funding: The authors have no relevant financial or non-financial interests to disclose.
This study was funded by German Cancer Aid (Grant No: 110948; 70112752; 70113932). The funding source was not involved in any stage of the research process.
Introduction
Adolescents and young adults (AYAs), aged 15 to 39 years at diagnosis, represent a unique group of cancer survivors facing distinct psychosocial and sexual health challenges [1, 2]. AYA cancer survivors experience several life events, including physical maturation, formation of romantic partnerships, and exploration of intimacy during a critical developmental period [3, 4]. Cancer and its treatment can interfere with or postpone these life experiences, thereby affecting the psychosexual well-being of AYA cancer survivors [1].
Romantic relationships in adulthood are influenced by early attachment styles formed in childhood [5]. Attachment anxiety (fear of abandonment) and attachment avoidance (defensive independence) are two factors underlying the concept of attachment insecurity (AI) [6]. Attachment insecurity, particularly avoidance, is linked to diminished sexual and partnership satisfaction (PSAT), likely stemming from negative thoughts and distress about sexual encounters [7–9]. Insecure attachment styles increase distress, hinder emotional intimacy, and create challenges in forming and maintaining satisfying relationships [10–12].
Cancer treatments can lead to long-term sexual dysfunctions, which can further affect self-perception [13]. These disruptions in sexual satisfaction (SSAT) are closely associated with psychological challenges, including depression and decreased self-esteem [14]. For individuals managing chronic illnesses, such as cancer, partnerships play a pivotal role in shaping health outcomes [15]. Emotional support from a partner can reduce isolation, enhance coping, and improve mental health [16] by alleviating psychological distress and fostering emotional resilience in this population [17, 18].
It is essential to understand the complex dynamics that contribute to PSAT within this population. For this young population, navigating the challenges of cancer during a critical developmental period, the interplay between attachment style and partnership outcomes may have profound implications for their overall well-being and quality of life.
Therefore, this study aims to (1) investigate the levels of PSAT, SSAT, and AI across sociodemographic and medical factors and (2) explore how AI, i.e. attachment-related anxiety (AAX) and attachment-related avoidance (AAV) influence the relationship between SSAT and PSAT among AYA cancer survivors across major tumor entities. By addressing these aims, this research enhances our understanding of the psychosocial needs of AYA cancer survivors, emphasizing the importance of encompassing not only medical aspects but also emotional and social factors.
Patients and methods
Study design and sample
We used data from the first and last measurement time point (t1: 05/2014-12/2015 and t6: 05/2021-09/2021) of the AYA-LE study, a prospective longitudinal study with six measurement time points investigating the temporal course and related factors of life satisfaction and psychological distress of AYA cancer survivors. The t6 survey focused specifically on AYA social relationships, such as partnership and sexuality [19, 20].
Patients were eligible for participating in the study if they (1) were between 18 and 39 years of age at diagnosis, (2) had first diagnosis of a cancer at any tumor site (C00–C97), (3) were diagnosed within the last 4 years at t1, and (4) were able to speak German and physically and cognitively able to participate. All participants gave written informed consent in accordance with the Declaration of Helsinki. The study was approved by the Research Ethics Committee of the University of Leipzig (Ref. 372–13–16,122,013).
Study recruitment and data collection
The total recruitment process in the AYE-LE study ran for a period of 88 months (from 05/14 to 09/21) in cooperation with 16 oncological acute care hospitals, two local tumor registries, and four (cancer) rehabilitation clinics specialized in treating AYA cancer survivors [21]. Patient recruitment in t6 was carried out from May 2021 to September 2021.
Patients who consented to participate received participant documents and the questionnaire by mail or could complete it online using the software LimeSurvey. Reminders were sent continuously every 10 days via email. A first postal reminder was sent after 4 weeks and a second postal reminder 3 weeks later.
Study measures
Sociodemographic and clinical characteristics
Sociodemographic characteristics, including sex at t1, age, partnership duration, and housing situation at t6, were obtained from patients’ self-reports. Clinical characteristics, including cancer diagnosis as reported by patients at t1, along with any new cancer-related complications due to cancer and its treatment, cancer recurrence, metastases, or second cancer diagnoses reported at t6 since t5-survey, were documented based on patient self-reports.
Sexual satisfaction
SSAT was assessed using the validated life satisfaction questionnaire (FLZ) – sexuality scale (FLZ-Sex) [22]. The FLZ-Sex uses seven items to quantify SSAT considering physical attraction, sexual efficiency, sexual contacts, sexual response, sexual partner interaction, communication, and sexual reactions. Participants are supposed to rate on a seven-point Likert-Scale from ‘very unsatisfied’ (1) to ‘very satisfied’ (7). The sum score of the scale ranges from 7 to 49 with higher scores indicating a higher level of SSAT [22]. The questionnaire demonstrates strong internal consistency, as indicated by a Cronbach’s alpha of 0.92 [23].
Partnership satisfaction
PSAT was assessed using the marital quality questionnaire (PFB) [24]. The PFB uses 30 items to measure marital quality on three subscales, that is tenderness (T), quarreling (Q), and togetherness/communication (TC). Each subscale contains 10 items with a four-point Likert scale asking participants to indicate whether their partner ‘never/almost never’ (0) to ‘quite often’ (3) exhibits a particular behavior. The overall quality of relationship score can be obtained with the following equation: PFB = (30 – Q) + T + TC and ranges from 0 to 90 with higher scores indicating a higher level of PSAT [24]. The questionnaire demonstrates strong internal consistency, as indicated by a Cronbach’s alpha of 0.94 [24].
Attachment insecurities
AI in adults was assessed using the validated German revised short version of the Experience of Close Relationships (ECR-RD8) [25]. The ECR-RD8 captures attachment-related cognitions and expectations with regard to romantic relationships on two scales: AAX and AAV. In the short version, each scale comprises four items to be rated on a 7-point Likert scale from ‘strongly disagree’ (1) to ‘strongly agree’ (7). Scores ranged from 8 to 56 with higher scores on one or both scales indicate an insecure romantic attachment style, whereas lower scores suggest a secure attachment style [25]. The questionnaire demonstrates good internal consistency, as indicated by a McDonald’s omega > 0,8 [25].
Statistical analysis
We applied descriptive analyses for both continuous (means, standard deviations) and categorical variables (frequencies, percentages). All four items of the avoidance subscale from the ECR were inverse coded before mean values were computed.
To examine differences in SSAT, PSAT, and AI scores between sociodemographic and clinical characteristics, t-tests or one-way analysis of variance (ANOVA) were calculated. Comparisons between participants and nonresponders were conducted using ANOVA with Bonferroni correction due to multiple comparisons (adjusted α level 0.00625). Linear correlations between two variables were examined with bivariate correlation using Pearson’s r.
We conducted parallel mediation using PROCESS model 4 with AAX (M1) and AAV (M2) as mediators and statistically significant covariates from univariate analyses (p < 0.05). Mediating effects were estimated through linear regression, following Baron and Kenny’s method [26]. First, SSAT significantly affects AAX and AAV (paths a1 and a2); second, SSAT significantly influences PSAT (path c); and third, AAX and AAV significantly affects PSAT (paths b1 and b2). If these conditions hold in the predicted direction, the effect of SSAT on PSAT in the third equation (path c’) was expected to be smaller than in the second (path c), indicating partial mediation if significant. We set bootstrap samples to 10,000 and the significance level to 0.10 for a two-sided test. The proportion mediated was calculated by dividing the indirect effect by the total effect. To test for differences in indirect effects, pairwise contrasts were conducted, with statistical significance determined by whether the confidence interval for the contrast value (C1) did not contain zero. This would indicate that the mediators have a different impact on our dependent variable PSAT.
Data analyses were performed with IBM SPSS Statistics 27 [27] and PROCESS Makro v4.2 for SPSS [28].
Results
Sample
Of the 371 eligible patients from the fifth measurement time point (t5), 341 (response rate = 91.9%) participated in the study at t6. Of these, 275 participants were in a partnership, had completed the PFB questionnaire, and were therefore included in the final analysis (Figure 1).
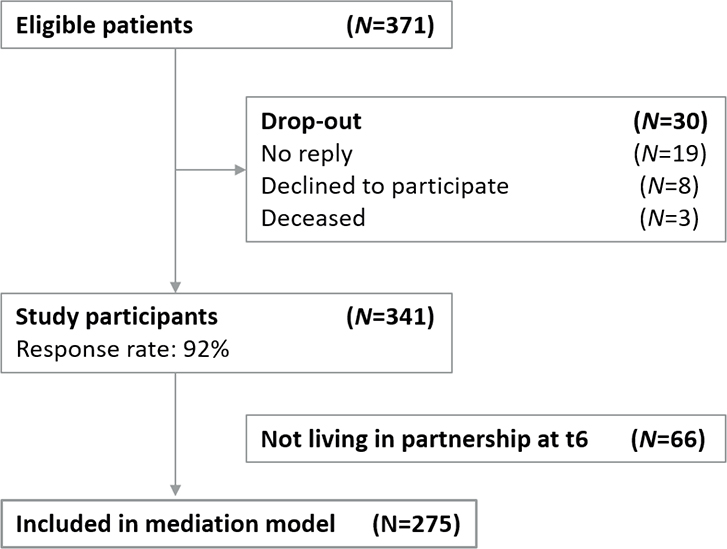
Figure 1. Flowchart of participants.
Notes. N = sample size.
Nonresponder analysis
Study participants (N = 341) at t6 were older (M = 37.10 years; SD = 6.11, p ≤ 0.001) differed in cancer entity (p = 0.012) with a higher percentage of breast cancer (28.7% vs. 9.8%) and a lower percentage of hematological cancers (6.0% vs. 14.6%) compared to nonresponders (N = 30). There were no significant differences in sex between both groups (p = 0.262).
Sample characteristics and scores of SSAT, AAX, AAV, and PSAT
Sample characteristics and differences in mean scores on the SSAT, PSAT, and both AAX and AAV across sociodemographic and clinical characteristics for participants who were in a partnership and were thus included in the final analysis are presented in Table 1. Participants had a mean age of 36.82 ± 6.23 years and an average partnership duration of 10.39 ± 7.10 years. For SSAT, the mean score on the FLZ-Sex was 31.95 ± 10.03. The mean scores on the ECR-RD for AAX and AAV were 2.26 ± 1.42 and 2.10 ± 1.27, respectively. Regarding PSAT, the mean score on the PFB total scale was 66.33 ± 16.02. For the subscales, the mean scores were 5.75 ± 5.40 for Q, 21.93 ± 6.17 for TC, and 20.18 ± 6.82 for T.
| Total sample | SSAT | PSAT2 | AI | ||
| AAX | AAV | ||||
| n (%) | M ± SD | M ± SD | M ± SD | ||
| 265 (100) | |||||
| Sociodemographic data | |||||
| Sex | |||||
| Male | 58 (21.9) | 34.34 ± 8.98 | 63.82 ± 15.33 | 2.08 ± 1.32 | 2.32 ± 1.37 |
| Female | 207 (78.1) | 31.28 ± 10.23 | 67.03 ± 16.31 | 2.31 ± 1.44 | 2.03 ± 1.24 |
| T | 2.068 | -1.349 | -1.074 | 1.533 | |
| p | 0.040* | 0.178 | 0.284 | 0.126 | |
| d | 0.31 | -0.20 | -0.16 | 0.22 | |
| Age [in yrs] | |||||
| ≤ 25 | 12 (4.5) | 34.33 ± 8.03 | 71.12 ± 12.71 | 2.06 ± 1.20 | 2.01 ± 1.29 |
| 26–30 | 62 (23.4) | 33.48 ± 9.10 | 67.42 ± 15.38 | 2.23 ± 1.59 | 1.98 ± 1.11 |
| 31–35 | 61 (23.0) | 31.21 ± 9.69 | 65.21 ± 14.56 | 2.30 ± 1.28 | 2.09 ± 1.07 |
| 36–40 | 57 (21.5) | 29.10 ± 11.98 | 62.58 ± 18.83 | 2.37 ± 1.53 | 2.24 ± 1.53 |
| > 41 | 73 (27.5) | 32.83 ± 8.15 | 61.96 ± 19.47 | 2.79 ± 1.36 | 2.50 ± 1.10 |
| F | 2.938 | 2.737 | 0.643 | 0.592 | |
| p | 0.021* | 0.029* | 0.632 | 0.669 | |
| Eta2 | 0.04 | 0.04 | 0.01 | 0.01 | |
| Partnership duration [in yrs]a | |||||
| < 5 | 61 (23.0) | 34.70 ± 9.23 | 68.83 ± 15.61 | 2.43 ± 1.60 | 2.04 ± 1.23 |
| 5–9 | 47 (17.7) | 32.55 ± 9.29 | 70.14 ± 13.49 | 1.84 ± 1.20 | 1.82 ± 0.99 |
| 10–14 | 46 (17.4) | 32.58 ± 9.74 | 68.06 ± 12.81 | 2.34 ± 1.50 | 1.94 ± 1.01 |
| 15–19 | 31 (11.7) | 28.58 ± 11.18 | 61.20 ± 18.35 | 2.39 ± 1.39 | 2.66 ± 1.56 |
| > 20 | 30 (11.3) | 29.26 ± 10.80 | 60.52 ± 16.95 | 2.13 ± 1.21 | 2.02 ± 1.18 |
| F | 2.712 | 3.224 | 1.405 | 2.454 | |
| p | 0.031* | 0.014* | 0.233 | 0.041* | |
| Eta2 | 0.04 | 0.05 | 0.02 | 0.04 | |
| Housing situation | |||||
| Alone | 27 (10.2) | 32.25 ± 10.42 | 62.87 ± 21.98 | 3.07 ± 1.65 | 2.67 ± 1.47 |
| Cohabiting with a partner | 232 (87.5) | 31.84 ± 10.05 | 66.55 ± 15.34 | 2.17 ± 1.36 | 2.04 ± 1.24 |
| Other | 6 (2.3) | 34.83 ± 8.58 | 73.33 ± 6.95 | 2.20 ± 1.48 | 1.54 ± 0.71 |
| T | 0.273 | 1.226 | 5.047 | 3.577 | |
| p | 0.762 | 0.295 | 0.007** | 0.029* | |
| Eta2 | 0.01 | 0.01 | 0.03 | 0.02 | |
| Clinical data | |||||
| Cancer Diagnosis | |||||
| Breast | 76 (28.7) | 29.02 ± 11.10 | 63.93 ± 17.04 | 2.38 ± 1.45 | 2.14 ± 1.27 |
| Gynaecological | 20 (7.5) | 31.15 ± 11.78 | 68.67 ± 16.79 | 2.62 ± 1.43 | 2.08 ± 1.29 |
| Testicular | 22 (8.3) | 32.31 ± 8.30 | 59.62 ± 16.60 | 2.22 ± 1.51 | 2.27 ± 1.07 |
| Thyroid | 17 (6.4) | 35.29 ± 6.77 | 74.16 ± 13.41 | 1.64 ± 0.97 | 1.55 ± 0.85 |
| Hematological | 92 (34.7) | 33.57 ± 8.84 | 66.33 ± 16.15 | 2.10 ± 1.29 | 2.17 ± 1.37 |
| Sarcoma | 8 (3.0) | 31.12 ± 11.31 | 67.49 ± 14.72 | 2.40 ± 1.85 | 1.93 ± 1.38 |
| Gastrointestinal | 7 (6.5) | 31.71 ± 14.07 | 65.29 ± 21.01 | 2.50 ± 1.68 | 2.03 ± 1.61 |
| Other | 23 (8.7) | 33.34 ± 9.94 | 64.11 ± 17.78 | 2.52 ± 1.80 | 1.98 ± 1.20 |
| F | 1.658 | 1.781 | 1.032 | 0.591 | |
| p | 0.120 | 0.091 | 0.409 | 0.763 | |
| Eta2 | 0.04 | 0.05 | 0.02 | 0.01 | |
| Cancer recurrence | |||||
| No | 257 (97.0) | 31.83 ± 10.10 | 66.12 ± 16.19 | 2.26 ± 1.42 | 2.12 ± 1.28 |
| Yes | 8 (3.0) | 35.62 ± 7.34 | 73.13 ± 6.64 | 2.18 ± 1.29 | 1.43 ± 0.53 |
| T | -1.051 | -1.219 | 0.153 | 1.496 | |
| p | 0.294 | 0.224 | 0.879 | 0.136 | |
| Cohens’s d | -0.37 | -0.43 | 0.05 | 0.53 | |
| Metastases | |||||
| No | 257 (97.0) | 32.14 ± 10.01 | 66.63 ± 15.90 | 2.26 ± 1.42 | 2.08 ± 1.26 |
| Yes | 8 (3.0) | 25.62 ± 9.33 | 56.57 ± 17.98 | 2.34 ± 1.23 | 2.50 ± 1.76 |
| T | 1.818 | 1.756 | -0.162 | -0.897 | |
| p | 0.070 | 0.080 | 0.871 | 0.370 | |
| d | 0.65 | 0.62 | -0.05 | -0.32 | |
| Cancer-related complications1 | |||||
| No | 228 (86.0) | 32.65 ± 9.82 | 67.08 ± 15.63 | 2.21 ± 1.35 | 2.05 ± 1.23 |
| Yes | 35 (13.2) | 26.88 ± 10.19 | 60.66 ± 17.75 | 2.59 ± 1.77 | 2.42 ± 1.50 |
| T | 3.218 | 2.222 | -1.478 | -1.603 | |
| p | <0.001*** | 0.027* | 0.141 | 0.110 | |
| d | 0.58 | 0.40 | -0.26 | -0.29 | |
| Second cancer diagnosisb | |||||
| No | 261 (98.5) | 32.04 ± 10.04 | 66.32 ± 16.13 | 2.27 ± 1.42 | 2.09 ± 1.28 |
| Yes | 4 (1.5) | 25.50 ± 8.58 | 66.67 ± 6.94 | 1.25 ± 0.35 | 2.25 ± 0.88 |
| T | 1.297 | -0.043 | 1.440 | -0.235 | |
| p | 0.196 | 0.966 | 0.151 | 0.815 | |
| d | 0.65 | -0.02 | 0.72 | -0.11 | |
| SSAT: sexual satisfaction; PSAT: partnership satisfaction; AI: attachment insecurities; AAX: attachment-related anxiety; AAV: attachment-related avoidance; yrs: years; n: sub-sample size; M: mean; SD: standard deviation; T: t-value; p: level of statistical significance based on chi-square-tests and t-test; F: f-value;. a n/a=50, b n/a=2, 1most common complications referred to lymphedema, fatigue, hormonal imbalances, and reduced physical capacity, 2PFB – global scale, *significant on a level of p < 0.05, **significant on a level of p < 0.01, ***significant on a level of p < 0.001. |
|||||
The relationship between SSAT, AAX, AAV, and PSAT
SSAT was significantly positive correlated with PSAT (r = 0.57, p < 0.001, 95%-CI [0.482, 0.646]). SSAT was significantly negative correlated with AAX (r = -0.51, p < 0.001, 95%-CI [-0.589, -0.433]) and negative correlated with AAV (r = -0.49, p < 0.001, 95%-CI [-0.566, -0.404]). AAX was significantly negative correlated with PSAT (r = -0.64, p < 0.001, 95%-CI[-0.708, -0,566]) and AAV was significantly negative correlated with PSAT (r = -0.72, p < 0.001, 95%-CI[-0.770, -0.652]).
Mediation role of AAX and AAV on SSAT and PSAT
Table 2 shows the mediating effects of both AAX (M1) and AAV (M2) with the summarized coefficients and significance values found in the mediation model. Upon incorporating age, partnership duration and cancer-related complications as covariates in the model, given their significance in prior analyses, the mediation analysis demonstrated that SSAT exerted a significant total effect on PSAT (path c: B = 0.757, p < 0.001). After entering the mediators in the model, SSAT predicted both mediators AAX (path a1: B = -0.056, p < 0.001) and AAV (path a2: B = -0.065, p < 0.001) significantly. Both AAX (path b1: B = -6.221, p < 0.001) and AAV (path b2: B = -3.353, p < .001) predicted PSAT significantly. SSAT still had a significant effect on PSAT after controlling for both AAX and AAV (path c’: B = 0.188, p = .006, Figure 2). The relationship between SSAT and PSAT is partially mediated by AAX and AAV, combined indirect effect a1b1+a2b2 = 0.568, 95%-CI [0.397, 0.757].
| Type | Effect | B | SE | T | p | 95% CIa | |
| LLCI | ULCI | ||||||
| Indirect effects | SSAT → AAX → PSAT | 0.218 | 0.053 | - | - | 0.122 | 0.331 |
| SSAT → AAV → PSAT | 0.350 | 0.075 | - | - | 0.215 | 0.509 | |
| Components | SSAT → AAX | -0.056 | 0.009 | -6.080 | < 0.001 | -0.074 | -0.038 |
| AAX → PSAT | -6.221 | 0.755 | -8.240 | < 0.001 | -7.709 | -4.732 | |
| SSAT → AAV | -0.065 | 0.011 | -5.953 | < 0.001 | -0.087 | -0.044 | |
| AAV → PSAT | -3.353 | 0.712 | -4.709 | < 0.001 | -4.757 | -1.949 | |
| Direct effect | SSAT → PSAT | 0.188 | 0.092 | 2.039 | 0.043 | 0.006 | 0.370 |
| Total effect | SSAT → PSAT | 0.757 | 0.114 | 6.622 | < 0.001 | 0.531 | 0.982 |
| Notes. anumber of bootstrap samples for percentile bootstrap confidence intervals: 10,000. B: standardized coefficient; SE: standard error; CI: confidence interval; LLCI: lower bounds; ULCI: upper bounds; T: t-value; p: p-value; SSAT: sexuality satisfaction; AAX: attachment-related anxiety; AAV: attachment-related avoidance; PSAT: partnership satisfaction. |
|||||||
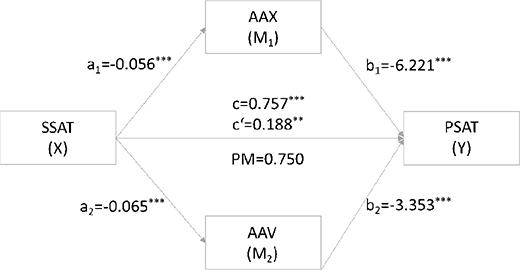
Figure 2. Mediating role of AAX (M1) and AAV (M2) on the relationship between SSAT and PSAT.
Notes. c’: direct effect of X on Y trough M1 and M2; c: total effect of X on Y. SSAT: sexual satisfaction; AAX: attachment-related anxiety; AAV: attachment-related avoidance; PSAT: partnership satisfaction; PM: proportion mediated, ratio of natural indirect to total effect, n = 275.
The proportion mediated by AAX and AAC was 0.750 (PM = 0.218+0.350/0.757), meaning that 75% of the effect of SSAT on PSAT was explained by AAX and AAV. SSAT exerts approximately equal effects on PSAT on the two mediation pathways, specific indirect effect contrast C1 = -0.131, 95%-CI [-0.042, 0.318].
Discussion
The purpose of this study was to examine the interrelations of AI on the relationship between SSAT and PSAT among AYA cancer survivors across all major tumor entities. Our findings revealed that higher SSAT was correlated with higher PSAT and lower AAX and AAV. Higher PSAT was correlated with lower AAX and AAV. Our mediation analyses further indicated that SSAT plays a partial predictive role in determining PSAT among AYA cancer survivors. This predictive influence operates through the mediation of AAX and AAV.
In our sample, the mean PSAT score was 66.33, slightly higher than the German normative score of 64.90, based on a sample of 1,114 individuals aged 18 to 50 years. However, subscale scores showed differences: higher conflict behavior (CB: M = 6.18 vs. M = 5.40), lower tenderness (T: M = 18.92 vs. M = 20.10), and comparable TC (TC: M = 20.77 vs. M = 20.10) [29]. The higher overall PSAT score suggests that AYA survivors may develop unique relational strengths, such as greater empathy and deeper connections with others. However, these findings also highlight the complexity of relationships for AYA cancer survivors, where increased conflict can coexist with overall satisfaction. Developmental challenges, such as the desire for autonomy while still depending on caregivers, can lead to tensions and emotional distress, potentially diminishing tenderness. It is important to note that not all conflicts are cancer related, as typical adolescent conflicts may also arise during this time [30].
Age significantly influenced PSAT in our sample. Specifically, younger AYA cancer survivors exhibited significantly higher satisfaction levels in their partnerships as older AYA cancer survivors (over 36 years old). This aligns with a Danish study among 151 AYA cancer survivors aged 15–29 years showing positive relationship changes in younger survivors [31], suggesting that younger survivors may exhibit greater adaptability and positive relationship dynamics. This might be due to by age-related differences in communication styles and support systems as younger adults often emphasize openness and immediacy in addressing emotions and challenges, reflecting generational shifts toward greater emotional expression. Additionally, younger survivors frequently benefit from strong support networks, including family and friends, which can alleviate cancer-related stress and enhance PSAT through emotional and practical support [32]. In contrast, older AYA survivors may face greater challenges if their support systems or communication styles are less responsive to the demands of postdiagnosis life. Furthermore, younger survivors often express a need for improved communication about cancer’s impact on their relationships, as effective communication fosters mutual understanding and support, further strengthening PSAT [33].
Our results further revealed that partnership duration significantly influenced PSAT. AYA cancer survivors in long-term partnerships (over 15 years) reported significantly lower satisfaction. Stress related to cancer treatment and survivorship can lead to decreased satisfaction, particularly in long-term partnerships where expectations diverge from postcancer realities. Communication difficulties and maladaptive coping strategies, such as withdrawal or avoidance, often contribute to relationship strain among survivors, particularly those with unsupportive or overly demanding partners [34–38].
AYA cancer survivors experiencing cancer-related complications exhibited significantly lower satisfaction with their partnerships, as ongoing health issues such as fertility concerns, body image disruptions, and mental health issues might strain AYA cancer survivors’ romantic partnerships. A study conducted in the United States involving 40 childhood cancer survivors revealed both positive and negative impacts of childhood cancer on their romantic partnerships in adulthood. However, the effects on physical intimacy were predominantly negative, with concerns related to fertility, such as feeling less desirable due to the inability to have biological children, as well as physical issues like self-consciousness about scars, hair loss, weight gain, erectile dysfunction, and premature menopause [39].
The mean scores for AAX and AAV in our study were 2.26 and 2.10, respectively. These values are slightly lower than those reported in a German evaluation study involving 1,006 healthy individuals with a mean age of 28.92 years, where the mean AAX and AAV scores were 2.77 and 2.36, respectively [40]. These lower scores may reflect adaptive responses to adversity, as cancer survivors often reevaluate relationships and priorities, potentially leading to stronger bonds with family and friends. This enhanced social support can reduce feelings of anxiety and avoidance in relationships, thereby reducing AI [33, 41].
Our mediation analyses indicated that SSAT plays a partial predictive role in influencing PSAT among AYA cancer survivors. Specifically, a higher level of SSAT corresponded to an elevated level of PSAT. This observation aligns with the outcomes of a Polish study involving 237 cancer-free young adults aged 18–25 years, where SSAT emerged as a primary predictor of PSAT in both sexes [42]. This implies that the connection between SSAT and PSAT is not exclusively driven by health status but represents a fundamental aspect of relationship satisfaction in young adults. SSAT holds a similar significance for AYA cancer survivors as it does for noncancer populations, despite the unique health-related challenges they face. The predictive impact operates via the mediation of AAX and AAV. More precisely, an elevated level of SSAT is associated with a decreased level of AAX and AAV. Reduced AAX and AAV aligns with increased PSAT. Findings from a systematic literature review revealed a consistent association between AI (avoidance and anxiety) and decreased SSAT across various relationship types in noncancer populations [43].
Study strengths and limitations
Although this study involved a considerably large sample size demonstrating similar age distribution and representation of tumor entities to the broader German AYA population types [21], it is essential to interpret our findings within the context of the following limitations.
As we examined PSAT in a cross-sectional setting, this does not allow interferences on causality and potential changes over time could not be considered, thus further studies on longitudinal effects should be conducted.
In our study, frequency of occurrence estimation was based on self-reports. Sexual health and its vulnerability are an issue prone to stigmatization. It is also possible that self-reported data is biased toward underestimation or is a subject to social acceptability bias. On this topic, however, it should be noted that this problem may be masked by patients in face-to-face interviews, so that the assessment by self-report may provide even more valid data.
Clinical implications
AYA cancer survivors require age-appropriate and flexible care, as well as informational needs and treatment-related education that foster autonomy for long-term survivorship [44]. The observed associations among SSAT, PSAT, and attachment-related factors underscore the necessity for a comprehensive and nuanced approach in designing and implementing psychosocial support interventions for AYA cancer survivors, given the current absence of tailored interventions.
In order to facilitate the targeted development of effective therapeutic interventions, it is essential to assess attachment styles. This can be achieved through the Adult Attachment Interview (AAI) [45]. Rather than focusing on the degree of security or insecurity in childhood attachments, this assessment is concerned with how adults reflect on their early attachment experiences and how they interpret these experiences within the context of their current relationships. Working through unresolved attachment issues with a trained therapist can lead to healthier attachment patterns. Interventions should therefore primarily focus on promoting secure attachment patterns, as securely attached individuals demonstrate superior emotion regulation capabilities, exhibiting a more balanced approach to both positive and negative affective states [46]. This balanced emotional regulation is crucial for maintaining healthy interpersonal relationships and overall psychological well-being. By fostering secure attachment, interventions may facilitate the development of more effective emotion regulation skills, such as reducing worry and rumination, and enhancing pleasure and satisfaction, potentially leading to improved outcomes in both sexual and relational domains for AYA cancer survivors and their partners [6].
Therapeutic interventions addressing sexual concerns should emphasize sexual emotions, such as pleasure, satisfaction, and related states of anxiety and worry, as well as the relational goals associated with sexual activity, rather than focusing on sexual performance. These interventions should also incorporate the perspectives of partners to enhance relational stability and adapt to changing roles in challenging situations. It is further important to explore factors that may help to fix maladaptive and insecure attachment styles and to nourish attachment security, as this is an important protective factor for sustained satisfaction in sexual and romantic partnerships.
Future research should prioritize longitudinal studies on attachment and emotion regulation to examine how attachment styles evolve over time in AYA cancer survivors and their impact on emotional regulation and relationship satisfaction. Such research could identify critical periods for targeted interventions. Our findings further highlight the need for research on how specific cancer-related complications affect relationships and on identifying vulnerable partnership stages. Such investigations could help to inform the development of targeted programs focusing on managing caregiving-related stress in long-term partnerships or enhancing communication skills in newer relationships impacted by cancer. These targeted approaches could lead to more personalized interventions that mitigate the negative impact of these factors and promote healthier relationship dynamics in survivors. Further investigation should also assess the effectiveness of interventions that actively involve partners in the therapeutic process, including the potential benefits of couple-based therapy for enhancing relationship satisfaction and sexual well-being.
By addressing these areas, future research can significantly contribute to the development of effective, nuanced, and comprehensive support systems for AYA cancer survivors, ultimately enhancing their quality of life and long-term survivorship outcomes.
Conclusions
The identified associations between SSAT, PSAT, and attachment-related variables highlight the importance of addressing both emotional and relational dimensions in supportive care interventions tailored for AYA cancer survivors. There is a clear need for more targeted studies on attachment patterns, SSAT, and PSAT in this specific population to further refine and validate these approaches.
Acknowledgements
The research team gratefully acknowledges the patients who participated in the study. The authors acknowledge the support by the Open Access Publishing Fund of Leipzig University, supported by the German Research Foundation within the program Open Access Publication Funding.
Author contributions
KG, DR, HB, and AS contributed to the manuscript conception and design. Material preparation and data collection were performed by KG, HB, DR, and AS. Data analysis was conducted by SH and MF. The first draft of the manuscript was written by SH, supervised and edited by AMT and JR, all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Data availability
The datasets presented in this article are not readily available because of data protection regulations concerning patient information (which assures participants that the data will not be passed on to third parties) but are available from the corresponding author upon reasonable request.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Approval was granted by the Ethics Committee of University of Leipzig (Ref. No: 045/20-ek).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
References
[1] Reinman L, Coons HL, Sopfe J, Casey R. Psychosexual care of adolescent and young adult (AYA) cancer survivors. Children (Basel). 2021;8(11):1074. https://doi.org/10.3390/children8111074
[2] National Cancer Institute. Adolescents and young adults with cancer [Internet]. 2024 [cited 2024 Dec 5]. Available from: https://www.cancer.gov/types/aya
[3] Levin NJ, Zebrack B, Cole SW. Psychosocial issues for adolescent and young adult cancer patients in a global context: A forward-looking approach. Pediatr Blood Cancer. 2019;66(8):e27789. https://doi.org/10.1002/pbc.27789
[4] Cherven B, Sampson A, Bober SL, Bingen K, Frederick N, Freyer DR, et al. Sexual health among adolescent and young adult cancer survivors: a scoping review from the Children’s Oncology Group Adolescent and Young Adult Oncology Discipline Committee. CA Cancer J Clin. 2021;71(3):250–63. https://doi.org/10.3322/caac.21655
[5] Bowlby J. The making and breaking of affectional bonds. I. Aetiology and psychopathology in the light of attachment theory. An expanded version of the Fiftieth Maudsley Lecture, delivered before the Royal College of Psychiatrists, 19 November 1976. Br J Psychiatry. 1977;130:201–10. https://doi.org/10.1192/bjp.130.3.201
[6] Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research, and clinical applications. New York: The Guilford Press; 2016, 1068 p.
[7] Heresi Milad E, Rivera Ottenberger D, Huepe Artigas D. Associations among attachment, sexuality, and marital satisfaction in adult Chilean couples: a linear hierarchical models analysis. J Sex Marital Ther. 2014;40(4):259–74. https://doi.org/10.1080/0092623X.2012.751076
[8] Khoury CB, Findlay BM. What makes for good sex? The associations among attachment style, inhibited communication and sexual satisfaction. J Relatsh Res. 2014;5:e7. https://doi.org/10.1017/jrr.2014.7
[9] Little KC, McNulty JK, Russell VM. Sex buffers intimates against the negative implications of attachment insecurity. Pers Soc Psychol Bull. 2010;36(4):484–98. https://doi.org/10.1177/0146167209352494
[10] Ramos K, Leo K, Porter LS, Romano JM, Baucom BRW, Langer SL. Attachment in couples coping with cancer: Associations with observed communication and long-term health. Int J Environ Res Public Health. 2023;20(7):5249. https://doi.org/10.3390/ijerph20075249
[11] Lehmann V, Keim MC, Ferrante AC, Olshefski RS, Gerhardt CA. Psychosexual development and satisfaction with timing of developmental milestones among adult survivors of childhood cancer. Psychooncology. 2018;27(8):1944–9. https://doi.org/10.1002/pon.4728
[12] do Rosário Ramos Nunes Bacalhau M, Pedras S, Da Graça Pereira Alves M. Attachment style and body image as mediators between marital adjustment and sexual satisfaction in women with cervical cancer. Support Care Cancer. 2020;28(12):5813–9. https://doi.org/10.1007/s00520-020-05423-y
[13] Bober SL, Varela VS. Sexuality in adult cancer survivors: challenges and intervention. J Clin Oncol. 2012;30(30):3712–9. https://doi.org/10.1200/JCO.2012.41.7915
[14] Olsson M, Steineck G, Enskär K, Wilderäng U, Jarfelt M. Sexual function in adolescent and young adult cancer survivors – a population-based study. J Cancer Surviv. 2018;12(4):450–9. https://doi.org/10.1007/s11764-018-0684-x
[15] Kiecolt-Glaser JK. Marriage, divorce, and the immune system. Am Psychol. 2018;73(9):1098–108. https://doi.org/10.1037/amp0000388
[16] Warner EL, Nam GE, Zhang Y, McFadden M, Wright J, Spraker-Perlman H, et al. Health behaviors, quality of life, and psychosocial health among survivors of adolescent and young adult cancers. J Cancer Surviv. 2016;10(2):280–90. https://doi.org/10.1007/s11764-015-0484-5
[17] Obertson EG, Sansom-Daly UM, Wakefield CE, Ellis SJ, McGill BC, Doolan EL, et al. Sexual and romantic relationships: Experiences of adolescent and young adult cancer survivors. J Adolesc Young Adult Oncol. 2016;5(3):286–91. https://doi.org/10.1089/jayao.2015.0061
[18] Stinson JN, Jibb LA, Greenberg M, Barrera M, Luca S, White ME, et al. A qualitative study of the impact of cancer on romantic relationships, sexual relationships, and fertility: perspectives of Canadian adolescents and parents during and after treatment. J Adolesc Young Adult Oncol. 2015;4(2):84–90. https://doi.org/10.1089/jayao.2014.0036
[19] Leuteritz K, Friedrich M, Nowe E, Sender A, Stöbel-Richter Y, Geue K. Life situation and psychosocial care of adolescent and young adult (AYA) cancer patients – study protocol of a 12-month prospective longitudinal study. BMC Cancer. 2017;17(1):82. https://doi.org/10.1186/s12885-017-3077-z
[20] Geue K, Mehnert-Theuerkauf A, Stroske I, Brock H, Friedrich M, Leuteritz K. Psychosocial Long-term effects of young adult cancer survivors: Study protocol of the longitudinal AYA-LE long-term effects study. Front Psychol. 2021;12:688142. https://doi.org/10.3389/fpsyg.2021.688142
[21] Leuteritz K, Friedrich M, Nowe E, Sender A, Taubenheim S, Stoebel-Richter Y, et al. Recruiting young adult cancer patients: Experiences and sample characteristics from a 12-month longitudinal study. Eur J Oncol Nurs. 2018;36:26–31. https://doi.org/10.1016/j.ejon.2018.07.003
[22] Henrich G, Herschbach P. Questions on life satisfaction (FLZM) – a short questionnaire for assessing subjective quality of life. Eur J Psychol Assess. 2000;16(3):150–9. https://doi.org/10.1027//1015-5759.16.3.150
[23] Schumacher J, Laubach W, Brähler E. Wie zufrieden sind wir mit unserem Leben? Soziodemographische und psychologische Prädiktoren der allgemeinen und bereichsspezifischen Lebenszufriedenheit. Zeitschrift für Medizinische Psychologie. 1995;4:17–26.
[24] Hahlweg K. Konstruktion und Validierung des Partnerschafts fragebogens PFB. Z Klin Psychol. 1979;8:17–40. https://doi.org/10.1027//0044-3409.08.1.17
[25] Ehrenthal JC, Zimmermann J, Brenk-Franz K, Dinger U, Schauenburg H, Brähler E, et al. Evaluation of a short version of the experiences in close relationships-revised questionnaire (ECR-RD8): results from a representative German sample. BMC Psychol. 2021;9(1):140. https://doi.org/10.1186/s40359-021-00637-z
[26] Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82. https://doi.org/10.1037/0022-3514.51.6.1173
[27] IBM Corp. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp; 2019
[28] Hayes AF. The PROCESS macro for SPSS, version 4.2. [Internet]. 2022. Available from: https://www.processmacro.org.
[29] Hinz A, Stöbel-Richter Y, Brähler E. Der Partnerschaftsfragebogen (PFB): Normierung und soziodemographische Einflussgrößen auf die Partnerschaftsqualität [The “Partnerschaftsfragebogen” (marital quality questionnaire): Psychometric norms and sociodemographic influences on partnership quality]. Diagnostica. 2001;47(3):132–41. https://doi.org/10.1026//0012-1924.47.3.132
[30] Kay JS, Juth V, Silver RC, Sender LS. Support and conflict in relationships and psychological health in adolescents and young adults with cancer. J Health Psychol. 2019;24(4):502–17. https://doi.org/10.1177/1359105316676629
[31] Graugaard C, Sperling CD, Hølge-Hazelton B, Boisen KA, Petersen GS. Sexual and romantic challenges among young Danes diagnosed with cancer: results from a cross-sectional nationwide questionnaire study. Psychooncology. 2018;27(6):1608–14. https://doi.org/10.1002/pon.4686
[32] Acquati C, Miller-Sonet E, Zhang A, Ionescu E. Social wellbeing in cancer survivorship: A cross-sectional analysis of self-reported relationship closeness and ambivalence from a community sample. Curr Oncol. 2023;30(2):1720–32. https://doi.org/10.3390/curroncol30020132
[33] Janssen SHM, van der Graaf WTA, van der Meer DJ, Manten-Horst E, Husson O. Adolescent and young adult (AYA) cancer survivorship practices: An overview. Cancers (Basel). 2021;13(19):4856. https://doi.org/10.3390/cancers13194856
[34] Borstelmann NA, Rosenberg SM, Ruddy KJ, Tamimi RM, Gelber S, Schapira L, et al. Partner support and anxiety in young women with breast cancer. Psychooncology. 2015;24(12):1679–85. https://doi.org/10.1002/pon.3773
[35] Carpentier MY, Fortenberry JD, Ott MA, Brames MJ, Einhorn LH. Perceptions of masculinity and self-image in adolescent and young adult testicular cancer survivors: implications for romantic and sexual relationships. Psychooncology. 2011;20(7):738–45. https://doi.org/10.1002/pon.1780
[36] Lewis PE, Sheng M, Rhodes MM, Jackson KE, Schover LR. Psychosocial concerns of young African American breast cancer survivors. J Psychosoc Oncol. 2012;30(2):168–84. https://doi.org/10.1080/07347332.2011.651261
[37] Robinson L, Miedema B, Easley J. Young adult cancer survivors and the challenges of intimacy. J Psychosoc Oncol. 2014;32(4):447–62. https://doi.org/10.1080/07347332.2014.917138
[38] Thompson AL, Long KA, Marsland AL. Impact of childhood cancer on emerging adult survivors’ romantic relationships: a qualitative account. J Sex Med. 2013;10(Suppl 1):65–73. https://doi.org/10.1111/jsm.12058
[39] Nahata L, Morgan TL, Lipak KG, Olshefski RS, Gerhardt CA, Lehmann V. Romantic relationships and physical intimacy among survivors of childhood cancer. J Adolesc Young Adult Oncol. 2020;9(3):359–66. https://doi.org/10.1089/jayao.2019.0114
[40] Ehrenthal JC, Dinger U, Lamla A, Funken B, Schauenburg H. Evaluation der deutschsprachigen Version des Bindungsfragebogens “Experiences in Close Relationships--Revised” (ECR-RD). Psychother Psychosom Med Psychol. 2009;59(6):215–23. https://doi.org/10.1055/s-0028-1103294
[41] Link C, Qi S, Thompson S, DeIure A, McKillop S, Watson L. Understanding the symptoms and concerns of adolescents and young adults with cancer in Alberta: A comparative cohort study using patient-reported outcomes. J Adolesc Young Adult Oncol. 2023;12(2):199–206. https://doi.org/10.1089/jayao.2022.0079
[42] Józefacka NM, Szpakiewicz E, Lech D, Guzowski K, Kania G. What matters in a relationship-age, sexual satisfaction, relationship length, and interpersonal closeness as predictors of relationship satisfaction in young adults. Int J Environ Res Public Health. 2023;20(5):4213. https://doi.org/10.3390/ijerph20054213
[43] Stefanou C, McCabe MP. Adult attachment and sexual functioning: a review of past research. J Sex Med. 2012;9(10):2499–507. https://doi.org/10.1111/j.1743-6109.2012.02843.x
[44] Barnett M, McDonnell G, DeRosa A, Schuler T, Philip E, Peterson L, et al. Psychosocial outcomes and interventions among cancer survivors diagnosed during adolescence and young adulthood (AYA): a systematic review. J Cancer Surviv. 2016;10(5):814–31. https://doi.org/10.1007/s11764-016-0527-6
[45] George C, Main M, Kaplan N. Adult Attachment Interview (AAI) [database record]. APA PsycTests. 1985. Available from: https://doi.org/10.1037/t02879-000.
[46] Mikulincer M, Shaver PR. Attachment in adulthood: structure, dynamics, and change. 2018th ed. New York: The Guilford Press; 2018.