CASE REPORT
CASE REPORT OF IDIOPATHIC NORMAL PRESSURE HYDROCEPHALUS: A CHALLENGING DIAGNOSIS
Lina VAN BRABANDER, MD1,2, Liesbet HUYGHEBAERT, MD1 and Marie-Sophie VERMOERE, MD1
From the 1Physical Medicine and Rehabilitation, AZ Glorieux, Ronse, Belgium and 2Physical Medicine and Rehabilitation, UZ Brussel, Jette, Belgium
Introduction: This report concerns the case of a 70-year-old man with idiopathic normal pressure hydrocephalus (iNPH). The diagnosis in the current case took more than 2 years. iNPH is characterised by ventriculomegaly with a known triad of symptoms: gait disturbance, cognitive impairments and urinary incontinence. Although this is a difficult diagnosis and other conditions must be ruled out, several points in the process could lead to a correct diagnosis. The aim of the report is to identify several reasons why the diagnosis was delayed for such a long time, as well as lessons for the future.
Case: This patient developed several symptoms over time. First, he presented with depressive mood and altered behaviour. He later developed gait difficulties and, finally, urinary incontinence. Multiple consultations and examinations failed to provide an exact explanation for all his symptoms. After 2 years, a new doctor at the hospital started from scratch and recognised the iNPH triad, and the diagnosis was confirmed by the radiologist.
Conclusion: The diagnosis of iNPH is difficult, as symptoms may manifest over time. In this case, the delay of diagnosis exceeded estimations. A broader view through interdisciplinary consultation could provide new insights and lead to earlier diagnosis.
LAY ABSTRACT
The patient experienced gait difficulties, urinary incontinence and cognitive problems, like dementia. The diagnosis was challenging and took several examinations and hospital admissions. The diagnosis took longer than expected. Several key points in the diagnostic process are evaluated, and suggestions are made to prevent such delays in the future.
Key words: idiopathic normal pressure hydrocephalus; ventriculomegaly; triad; gait impairments; gait ataxia; urinary incontinence; cognitive impairment; ventriculoperitoneal shunt; delay in diagnosis; missed diagnosis.
Citation: JRM-CC 2023; 6: jrmcc11631. DOI: https://doi.org/10.2340/jrmcc.v6.11631
Copyright: © Published by Medical Journals Sweden, on behalf of the Foundation for Rehabilitation Information. This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/)
Accepted: Oct 5, 2023; Published: Oct 30, 2023
Correspondence address: Lina Van Brabander, Physical Medicine and Rehabilitation, AZ Glorieux, Glorieuxlaan 55, 9600 Ronse, Belgium. E-mail: Lina.vanbrabander@azglorieux.be
Competing interests and funding: The authors have no conflicts of interest to declare.
Idiopathic normal pressure hydrocephalus (iNPH) is typically characterised by ventriculomegaly and a triad of symptoms, also known as the Adam’s triad or Hakim’s triad: gait disturbance, cognitive impairment and urinary incontinence (1–4). The diagnosis can be challenging. These symptoms may not all occur simultaneously, and they can emerge at different stages of the disease with varying levels of severity. Given the possibility of other coexisting conditions, the symptoms may not be completely explained by another disease. An extensive and detailed history of each of the symptoms is required (2, 5, 6). In most patients, symptoms start slowly over at least 3–6 months prior to presentation at the consultation (1).
This report represents a case in which the diagnosis took more than 2 years.
CASE PRESENTATION
A 70-year-old man presented to a neurologist in February 2020 with complaints of aggressive behaviour, depressed mood, gait problems and general deterioration.
The patient’s medical history listed chronic axonal-demyelinating sensory-motoric polyneuropathy, peripheral arterial vascular disease, chronic kidney insufficiency, hypertension and diabetes mellitus. He also had a pacemaker, due to paroxysmal atrial fibrillation. He had quit smoking in 1995. Alcohol consumption was not clearly stated.
Clinical examination revealed general weakness and areflexia in the four limbs. Electroencephalography (EEG) was normal, as was a CT scan of the brain, according to the protocol. Nerve conduction studies and electromyography (ENMG) indicated the known polyneuropathy, most probably due to diabetes mellitus.
A CT scan of the lumbar spine could not explain the impaired gait.
A second contact with the same neurologist took place 4 months later. The gait problems had increased, accompanied by aggressive behaviour, loss of interest and problems with executive functioning.
A second CT scan of the brain listed a ventriculomegaly, but not in the conclusion.
As treatment, the patient was advised to see a psychologist for the depressed mood and to visit a rehabilitation centre for the gait impairment. The latter recommendation was refused.
In November 2021, the patient went to the urologist because of urinary incontinence. A urodynamic study revealed an overactive bladder, which was treated with medication. There was no improvement at all.
Two months later, the patient was admitted to hospital because of generalised deterioration, acute renal insufficiency and dysregulated glycaemia. During this admission, the patient was confused and delirious. Gait problems were evident, with an increased risk of falling, as well as urinary incontinence. Rehabilitation was then started for the first time.
Less than a few weeks after discharge, May 2022, the patient was readmitted to hospital, in the intensive care unit, after a fall with rib fractures and haemothorax. He was disoriented and developed hyperactive delirium, reported as being of multifactorial origin. At this time, ethyl abuse was mentioned. This could have explained the falls, cognitive dysfunction and delirium.
On admission to the rehabilitation unit (May 2022), the patient was seen for the first time by one of the authors. He had a cognitive deficit, an impaired gait with frequent falling and urinary incontinence. Upon clinical examination, cogwheel rigidity, gait impairments and ataxia were noticed. In the absence of a diagnosis, a PET scan was requested, and the imaging was reviewed by the radiologist. Heteroanamnesis with the patient’s spouse revealed that the symptoms were progressively increasing, but alcohol consumption was not mentioned. According to the spouse, the patient was no longer the same person she used to know. The triad of symptoms was recognised, and a retrograde review of imaging confirmed the suspicion of iNPH (Figs. 1 and 2).
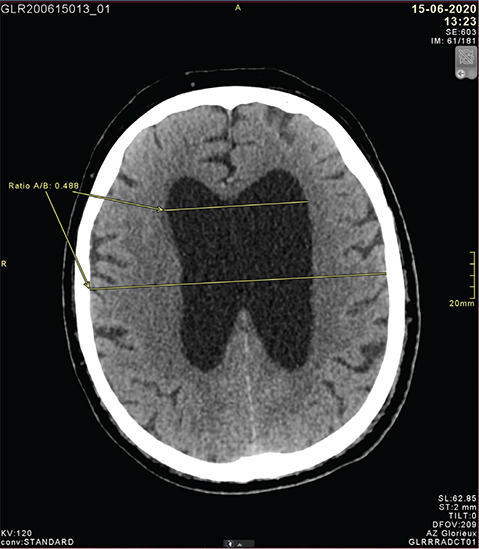
Fig. 1. A CT scan taken on June 2020 with Evans ratio calculated as 0.48.
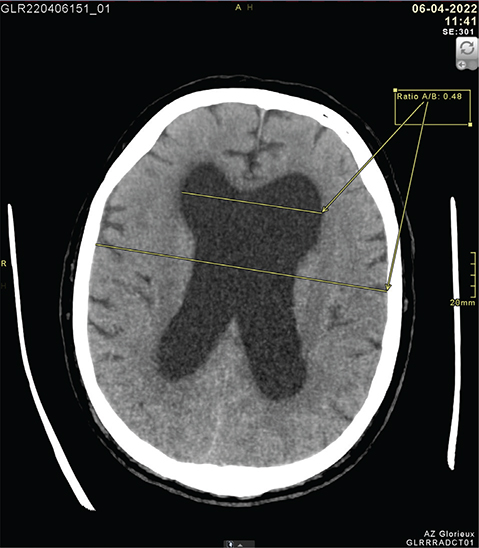
Fig. 2. A CT scan taken on April 2022 with Evans ratio calculated as 0.48.
Following the diagnosis, a diagnostic lumbar puncture was performed with drainage of 30 ml cerebrospinal fluid (CSF). Testing pre- and post-puncture indicated an increase in scores on the Mini Mental State Exam (MMSE) from 24 to 27/30. In addition, the Timed Up & Go test was significantly better. Clinical improvements were also observed in gait pattern and cognition.
A ventriculoperitoneal shunt (VP shunt) was placed successfully: cognition improved, and both gait disturbances and urinary incontinence disappeared. Neurological examination normalised. Multidisciplinary rehabilitation was subsequently continued with favourable results, despite the long existence of the symptoms.
Upon discharge from our ward, the patient was able to walk securely and independently. Further rehabilitation was provided at home. Vertigo and fatigue remained and were followed up by the neurologist. With the improvement of urinary incontinence, medication could be tapered off.
DIAGNOSIS
The diagnostic criteria contained in international guidelines differ slightly from those in Japanese guidelines. According to both sets of guidelines, iNPH is suspected in elderly (≥ h60 years) patients with at least one of the triad criteria. Diagnosis further requires ventriculomegaly, as confirmed by brain imaging (5, 6).
Patients diagnosed with iNPH have usually experienced symptoms for 3–6 months before receiving a diagnosis. Heteroanamnesis is very useful, partly because of the cognitive impairment that patients develop (5). Gait impairment is the most frequent symptom seen in this condition, and it is usually the first to emerge (6). If this symptom is absent, other causes should be considered first. Neuroimaging can confirm the suspicion of the diagnosis, in addition to ruling out other central causes (2,5,6). On imaging, ventriculomegaly is quantified according to the Evans ratio: the maximum width of the anterior horns of the lateral ventricles, divided by the maximum width of the calvarium at the same level on an axial MRI or CT image. Definite ventriculomegaly is defined as an Evans ratio of at least 0.3 (2, 5, 7). In this case, the Evans Ratio was calculated post hoc (Figs 1 and 2).
The preferred form of imaging is MRI of the brain, as it can rule out other diseases or comorbidities (1, 2, 4, 6). Other causes of ventriculomegaly could be obstructions (e.g. due to tumour or aqueductal stenosis (6)).
If in doubt about iNPH, a CSF drainage test can confirm diagnosis. This test also has predictive value for the outcome of therapy (i.e. placement of a VP shunt). The procedure should nevertheless be considered on a case-by-case basis, given the possibility of improvement after surgery even without improvement after a CSF drainage test (6).
The test involves removing 30–50 mL of CSF by single or multiple lumbar punctures to see whether symptoms improve after 2–3 hours (1, 5).
In the differential diagnosis, the following causes should be excluded and treated. In the elderly, many health conditions may mimic this disease. Examples include medication side effects, disorders of the locomotor system, cervical myelopathy, lumbar spine stenosis, vascular dementia, Lewy body dementia, frontotemporal dementia, Parkinsonism with dementia, depression, overactive bladder syndrome, prostate problems and pelvic floor dysfunction. When other conditions are present and treated without result, a diagnosis of iNPH should be considered (6).
THERAPY
Surgery is the standard treatment to manage the symptoms of iNPH, although it is not a cure (4, 6). Removing CSF and placing a shunt typically result in faster gait, better cognitive function and fewer urinary symptoms. The most commonly used are VP shunts. Other options include lumboperitoneal shunts (LP shunts) (3, 6, 7).
The success rate is highly variable. Symptoms of iNPH improve substantially with surgery in 73–96% of all patients (1, 6). Gait impairments are most responsive to surgery. Cognitive impairments and urinary symptoms improve in 60–80% of all cases (6).
Post-operative rehabilitation can restore a patient’s functioning to the condition prior to the onset of symptoms. It is therefore always important to include such programmes in the treatment plan.
Multidisciplinary rehabilitation should include exercises for balance, fall prevention, gait rehabilitation, neuro-cognitive training, practising activities of daily living, providing aids and offering compensatory strategies (6). A few randomised controlled trials have shown that functional exercise programmes and dynamic equilibrium gait training can have beneficial effects on gait, balance and fall incidence (8, 9).
DISCUSSION
As mentioned previously, the diagnosis of iNPH is sometimes difficult. The diagnosis is particularly complicated by the number of comorbidities that could also explain the symptoms in elderly patients.
In the current case, the patient had a history of polyneuropathy, which could have explained both the gait disturbances and the urinary problems. Despite the thorough elaboration of these symptoms, no immediate explanation could be found for the patient’s problems.
As it occurred in this case, the course of the condition resulted in a very long time passing before the triad was recognised. Moreover, the radiologist’s initial report failed to mention ventriculomegaly.
The role of the COVID-19 lockdown in this case should not be underestimated. Information from the patient’s partner was definitely lacking, as patients were required to come alone for consultations. Moreover, time was lost due to the lockdown itself, as well as to the long waiting times thereafter. It is possible that the doctors were overburdened.
In addition to the stigma it could cause, the attribution of symptoms to alcohol use was somewhat hasty, given the absence of any evidence of alcohol abuse.
A fresh look at a case can serve to break through existing patterns of thinking and contribute new perspectives. In the current case, the recognition of the triad, along with the radiologist’s review of the imaging ultimately led to the diagnosis.
The conversation with the patient’s partner was especially valuable.
The outcome of shunting depends on the duration of the symptoms. In the current case, the patient recovered well, despite the fact that the diagnosis had taken 2 years.
Post-operative results are strongly influenced by whether rehabilitation is started. This was strongly em-phasised both before and after surgery.
CONCLUSION
In the current case, the diagnosis of iNPH was made very late. Although the COVID-19 period arguably played a role in this delay, several elements in the diagnostic process influenced the time to diagnosis as well. Failure to recognise the triad, the attribution of symptoms to alcohol use, and the failure to mention the presence of ventriculomegaly were responsible for the long delay in the diagnosis. A fresh look at a case, advice from a colleague and/or interdisciplinary consultation can provide new insight. In the absence of a well-founded diagnosis, these options can be very important.
REFERENCES
- Williams MA, Malm J. Diagnosis and treatment of idiopathic normal pressure hydrocephalus. Continuum (Minneap Minn) 2016; 22(2 Dementia): 579–599. https://doi.org/10.1212/CON.0000000000000305
- Factora R. When do common symptoms indicate normal pressure hydrocephalus? Cleve Clin J Med 2006; 73: 447–456. https://doi.org/10.3949/ccjm.73.5.447
- Wang Z, Zhang Y, Hu F, Ding J, Wang X. Pathogenesis and pathophysiology of idiopathic normal pressure hydrocephalus. CNS Neurosci Ther 2020; 26: 1230–1240. https://doi.org/10.1111/cns.13526
- Gavrilov GV, Gaydar BV, Svistov DV, Korovin AE, Samarcev IN, Churilov LP, et al. Idiopathic normal pressure hydrocephalus (Hakim-Adams Syndrome): clinical symptoms, diagnosis and treatment. Psychiatr Danub 2019; 31: 737–744.
- Nakajima M, Yamada S, Miyajima M, Ishii K, Kuriyama N, Kazui H, et al. Research committee of idiopathic normal pressure hydrocephalus. Guidelines for Management of Idiopathic Normal Pressure Hydrocephalus (Third Edition): Endorsed by the Japanese Society of Normal Pressure Hydrocephalus. Neurol Med Chir (Tokyo) 2021; 61: 63–97. https://doi.org/10.2176/nmc.st.2020-0292
- Isaacs A, Williams M, Hamilton M. Current update on treatment strategies for idiopathic normal pressure hydrocephalus. Curr Treat Options Neurol 2019; 21: 65. https://doi.org/10.1007/s11940-019-0604-z
- Miyajima M, Kazui H, Mori E, Ishikawa M. on behalf of the SINPHONI-2 Investigators. One-year outcome in patients with idiopathic normal-pressure hydrocephalus: comparison of lumboperitoneal shunt to ventriculoperitoneal shunt. J Neurosurg 2016; 125: 1483–1492. https://doi.org/10.3171/2015.10.JNS151894
- Nikaido Y, Urakami H, Okada Y, Akisue T, Kawami Y, Ishida N, et al. Rehabilitation effects in idiopathic normal pressure hydrocephalus: a randomized controlled trial. J Neurol 2023; 270: 357–368. https://doi.org/10.1007/s00415-022-11362-x
- Rydja J, Kollén L, Hellström P, Owen K, Nilsson AL, Wikkelsø C, et al. Physical exercise and goal attainment after shunt surgery in idiopathic normal pressure hydrocephalus: a randomised clinical trial. Fluids Barriers CNS 2021; 18: 51. https://doi.org/10.1186/s12987-021-00287-8